Opioids Part 2
Pharmacology of Opioids,
Assessment and Management
of Opioid Dependence
© 2009 University of Sydney
Treating James ….
• James is a 29 yr man with >10 yr Hx heroin & other drug
use
• Presents to ED with abscess in arm, pyrexia, heart murmur
• Injects heroin 2-3 times a day for past 15 months
• Works part time. ‘Deals to friends’ to support habit.
• Girlfriend started using heroin 2 years ago. She is 5
months pregnant & now infrequently uses heroin.
• In treatment 4 times before …
– Relapsed within days after each of 3 detoxes
– Stopped using for 3/12 in rehab, but relapsed on return
to community
• Would like to stop using … fed up & desperate
• Needs admission for Ix endocarditis
Learning Objectives
To be able to:
• Describe the pharmacology of opioids
• Assess the presence of dependence on
heroin or other opioids
• Discuss the role of different treatment
options
• Describe the management of opioid
withdrawal
Overview of presentation
• Heroin and other opioids
–
–
–
–
–
Opioid pharmacology
Opioid effects and withdrawal
Overdose
Patterns of use
Features of dependence
• Assessment
• Treatment approaches
– Detoxification
– Post-detoxification responses
– Substitution treatment: methadone,
buprenorphine, prescribed heroin, LAAM
• Selecting treatment: evidence-based practice
What is heroin?
Di-acetylmorphine
• Semi-synthetic opiate, derived from opium
poppy
• Vast majority of effects = morphine
• In Australia
– Most from South East Asia
– Water soluble for injecting
– >$300 /‘gram’, 10-20% purity
Agonists, partial
agonists, antagonists
•
•
•
Opioids produce their effect by
acting at the opioid receptors in
the nervous system
– -opioid receptor most
important
Agonists
– bind to the receptor and
stimulate physiological
activity
Partial agonists
– bind to the receptor but do
not produce maximum
stimulation
Antagonists
– have no intrinsic
pharmacological effect, but
bind to the receptor and can
block the action of an
agonist
100
Full Agonists: Heroin, morphine,
methadone, codeine
Size of Opiate Agonist Effect.
.
•
0
Threshold for respiratory
depression
Partial Agonists: Buprenorphine
Antagonists: Naltrexone, naloxone
Drug Dose
Lintzeris, N (2008). Unpublished data.
Reprinted with permission.
Opioid effects & withdrawal
Opioid effects
•
•
•
•
•
•
Analgesia
Sedation
Euphoria
Pinpoint pupils
Low BP, PR, RR
Dry skin, mouth,
urine
• Constipation,
bowel action
• Nausea, vomiting
Opioid withdrawal
•
•
•
•
•
Increased pain
Agitation, poor sleep
Dysphoria
Dilated pupils
Increased BP, PR,
RR
• Sweaty, urine
• Diarrhoea, abdo
cramps
• Nausea, vomiting
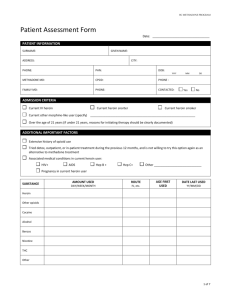
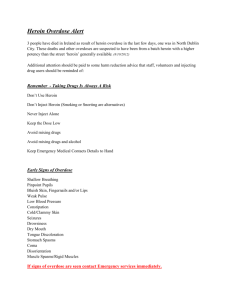
Opioid Overdose
• Signs
– Major feature - respiratory depression (slow
deep respiration 2-7/min) - risk of death
– Pinpoint pupils (but may be dilated if brain
damage occurred)
– Low BP, PR
– Low BT, skin cool, clammy
– Stuporose/comatose
• Treatment
– Reversal with naloxone (short-acting opioid
antagonist)
Source: NSW Department of Health (2007) NSW Drug and Alcohol Withdrawal Clinical Practice Guidelines
Patterns of Heroin Use
• The experimental user
• The 'recreational' or occasional user
– May or may not be associated with harms
(overdose, infections, other health risks, legal
complications)
• The dependent user
– Degrees of severity
– Severe dependence characterised by a
protracted course with multiple remissions
and relapses
Dependence (DSM IV-TR)
3 occurring at any time in the same 12 month period:
1. Tolerance
2.
Withdrawal
3.
Opioids taken in larger amounts or longer than
intended.
4.
Persistent desire or unsuccessful attempts to cut down
or control use.
5.
A great deal of time is spent in activities necessary to
obtain opioids, use opioids, or recover from their
effects.
6.
Important social, occupational, or recreational activities
are given up or reduced because of opioid use.
7.
Opioid use is continued despite knowledge of harms
caused or exacerbated by opioids.
Factors affecting drug abuse
& dependence
• Drug
• User
• Environment
Drug
•
•
•
•
•
•
•
Pharmacological effects
Onset of action
Duration of action
Route of administration
Purity
Availability
Cost
User
• Genetic predisposition or protection
• Expectancy of the effects
• Personality
– Impulsiveness, risk-taking, sensation
seeking
• Psychosocial
– Poor coping skills, low self-esteem,
history of psychological trauma
• Psychiatric co-morbidity
– Anxiety, depression, psychosis
Environment
• Family factors
– Attitudes towards substance use, parenting
skills
• Peer factors
– Attitudes towards substance use; role models
• Social factors
– School and neighbourhood attitudes towards
substance use; education; employment
status; socio-economic status; opportunities
for recreational activities; crime
‘Natural history’ of heroin
dependence
• Chronic, relapsing – remitting condition
– Usually starts several years after 1st heroin use
– 2 – 5 % remission rate per annum
• 1 – 2 % mortality rate per annum
– >10 x greater than age, gender matched non-users
– Overdose, liver disease (HCV, HBV), HIV, trauma
• 10 year outcomes (treatment seekers):
– 40 – 50% still using / imprisoned
– 30 – 40% abstinent
– 10 – 20% dead
• Most stop heroin use by late 30s to 40s.
Natural history
40 year follow-up study
Hser et al, 2001, Arch Gen Psychiatry, 58(5): 503-508, © 2001 American Medical Association.
Reprinted with permission.
Assessment
Role of assessment
Assessment serves two key functions:
• To ascertain valid information in order to
identify the most suitable management
plan;
• To engage the patient in the treatment
process
– Establishing rapport with the patient
– Facilitating treatment plans
Key features of the
assessment
• Presenting problem
• Drug use (include all drug classes)
– Quantity – frequency – route of administration
– Duration of use – when & amount last used
• Severity of dependence
– Withdrawal, tolerance, capacity to control use
• Drug related harms & risk practices
• Other conditions impacting upon treatment
– Medical / psychiatric / social
• Patient goals / expectancy
Conducting assessments
• History
• Examination
– Features of intoxication / withdrawal
– Evidence of drug use (e.g. injecting sites)
– Evidence of drug related harm (infections,
liver, heart murmurs)
• Investigations
– Urine drug screen
– Viral serology & LFTs
Evidence of drug use
Track marks provide
evidence for IDU and
last occasion of use
Stages of change model
(Prochaska & Di Clemente)
Pre-contemplation: People do not have major concerns
regarding their drug use and are not interested in
changing behaviour
Contemplation: People aware that there are both
benefits and problems arising from their drug use,
and are weighing up whether or not to make changes
- or what those changes should be
Action: People are implementing strategies in order to
change
Maintenance: holding onto the behaviour changes
Relapse: can be volitional, or triggered by physical,
emotional, social factors
Prochaska, JO et al (1985) Addict Behav, 10(4): 395-406.
ACTION
PREPARATION
MAINTENANCE
CONTEMPLATION
RELAPSE
• Some authors recognise a preparation stage before
the action stage
• In this diagram the pre-contemplation stage is merged
with relapse
Proude, E (2009), unpublished data
Treatment Options
Treatment pathways for
dependent heroin users
Dependent Heroin
User
Detox
Substitution
Maintenance
Treatment
Detox from
maintenance
treatment
Post Detox Treatment Options
Opioid withdrawal
syndrome
•
•
•
•
•
Increased pain
Agitation, poor sleep
Dysphoria
Dilated pupils
Increased BP, PR,
RR
• Sweaty, urine
• Diarrhoea, abdo
cramps
• Nausea, vomiting
Image source: NSW Department of Health (2007) NSW Drug and Alcohol Withdrawal Clinical Practice Guidelines
Objectives of detoxification
• Detox is not a ‘cure’ for heroin dependence
– Most heroin users relapse after withdrawal
– Need long-term treatment to achieve longterm changes
• Short-term intervention that aims to:
– Interrupt a pattern of heavy & regular drug
use
– Alleviate withdrawal discomfort
– Prevent complications of withdrawal
– Facilitate post-withdrawal treatment linkages
Components of detox program
• Assessment & client-treatment matching
• Supportive care
– ‘safe’ environment (inpatient / outpatient)
– patient information
– supportive counselling
– regular monitoring
• Medication
• Post-withdrawal linkages
Medication approaches for
detox
• Symptomatic medications
– Clonidine
– BZDs, NSAIDS, antiemetics, antidiarrhoeal agents,
etc.
• Methadone or buprenorphine
– Reducing doses over days / weeks
– Minimises severity of withdrawal symptoms
– Buprenorphine increasingly used internationally
• Antagonist assisted (‘rapid detox’)
– Uses naloxone / naltrexone as prelude to longer term
antagonist treatment
Heroin withdrawal
Unmedicated
Lofexidine / clonidine
Methadone (7 day)
Withdrawal severity
Buprenorphine (7 day)
Rapid detox' (naltrexone)
0
1
2
3
4
5
6
7
Day
Lintzeris, N (2008) unpublished data. Reprinted with permission.
8
9
10
Short buprenorphine detox
regimes
Inpatient
Outpatient
Day
Proposed
regime
Upper &
lower limits
1
8 mg
2
Day
Proposed
regime
Daily
dose
4 to 8mg
1
4mg BD
8 mg
12 mg
4 to 12mg
2
4mg BD
8 mg
3
10 mg
4 to 16mg
3
6 mg
4
8 mg
2 to 12mg
4mg mane
2mg nocte
5
4 mg
0 to 8mg
4
2mg BD
4 mg
6
-
0 to 4mg
5
2 mg mane
2 mg
7
-
0 to 2mg
6
No dose
Lintzeris, N et al (2006) National clinical guidelines and procedures for the use of
buprenorphine in the treatment of opioid dependence.
…but beware of limitations
of detox…
RCT BPN Maintenance vs Detox
• 40 subjects randomised to
– 1 week detox / 1 yr
maintenance
– All provided counselling for
1 year
• Heroin use
– Detox = all relapsed
– Maintenance=75% Opiate ()ve UDS
• Mortality (p=0.015)
– Detox 4/20 (20%)
– Maintenance 0/20
Reprinted from The Lancet. Kakko et al (2003) Lancet,
361:662-8 with permission from Elsevier.
RCT Methadone maintenance vs
gradual detox
• N=179 randomised to
– 1 year methadone
maintenance, or
– 6 months gradual
reduction + intensive
psychosocial
• Results: MMT had
significantly
–
–
–
–
Better treatment retention
Less heroin use
Fewer HIV risk practices
Fewer legal problems
Sees et al, 2000 JAMA, 283:1303. Copyright © 2000 American Medical
Association. All rights reserved. Reprinted with permission.
Key points about detox
• Do not expect ‘cures’ from detox programs
• Short term treatment usually = short term changes
• Medication only one aspect to good detox
• BPN optimal detox medication & increases postdetox options
NB: Detox is not a treatment for dependence but
rather a pre-treatment phase for some more
comprehensive treatments.
Treatment pathways for
dependent heroin users
Dependent Heroin
User
Detox
Substitution
Maintenance
Treatment
Detox from
maintenance
treatment
Post Detox Treatment Options
Post-withdrawal interventions
• Counselling
– Various models (supportive, behavioural,
dynamic)
– Cochrane review: limited efficacy of
outpatient counselling alone
• Residential rehabilitation (long term > 3/12)
• Self – help (Narcotics Anonymous)
• Naltrexone
– Opioid antagonist that blocks effects of heroin
use
– Effective for those who take it, but high drop
out rate (< 10% retention at 6 months)
Naltrexone : clinical issues
• Induction
–
–
–
–
>7 days after last heroin use,
>10 days after last methadone use,
1-5 days after last BPN use
Naloxone challenge test recommended (not postBPN)
• Maintenance
– Daily dosing of 25 to 50 mg per day
– Recommended duration of 6 to 12 months
• Cessation
– ? Increased sensitivity & risk of OD with opiates
• Interest in development of long-acting NTX (e.g.
depot injection, implant) to overcome problems of
poor adherence
Treatment pathways for
dependent heroin users
Dependent Heroin
User
Detox
Substitution
Maintenance
Treatment
Detox from
maintenance
treatment
Post Detox Treatment Options
Substitution treatment
• Provision of a long-acting prescribed opioid enables
patient to cease / reduce heroin use & related
behaviors
• Long term approach: opportunity for client to
distance themselves from drug-using lifestyle
• Combines medication with psychosocial services
• Medication options: methadone & buprenorphine
• Other medication options (not approved in
Australia): prescribed heroin, LAAM.
Methadone stabilisation
Reprinted from The Lancet.
Haber, PS et al (2009) “Management of injecting drug users admitted to hospital” Lancet, 374(9697):1284-93.
© 2009 with permission from Elsevier.
Principles of effective
treatment
•
•
•
•
Long duration of treatment
Adequate dose of medication
Quality of therapeutic relationship
Psycho-social supports for the patient
– Regular review, supervision & monitoring
– Participation in counselling
– Environment, family, friends, employment
Bio-psycho-social model for chronic condition
Does substitution treatment
work?
Heroin use
Despite considerable variation between programs,
almost all patients reduce heroin use
~ 1/2 of patients stop using heroin
~ 1/3 of patients use heroin infrequently
~ 1/6 of patients continue to use heroin
frequently
Does substitution treatment
work?
• Mortality rates
– Heroin users not in treatment = 1 - 2% per
annum (p.a.)
– Methadone maintenance treatment = 0.5 to 0.75
% p.a.
• HIV transmission
– Lower risk practices than users not in treatment
(placebo or wait list controls)
– Lower rates of HIV transmission
• Criminality
– Reduced crime in most patients after treatment
Methadone
•
•
•
•
Full agonist at - opioid receptor
Onset 30 - 60 min after dose, Peak after ~ 2 - 6 hrs
Long-acting: t1/2= 24-30 hrs: one dose / day
Opioid toxicity with too much methadone: sedation,
respiratory depression, death
– 1 dose of 20-40mg can kill child
– Repeated doses of 30–40mg can kill an adult
(opiate naïve)
– 1 dose of 70mg can kill an adult (opiate naïve)
• Widespread diversion & methadone related deaths
where no supervision (e.g. UK)
• Daily supervised dispensing at clinics / pharmacies
Henry-Edwards et al (2003) Clinical Guidelines and Procedures for the Use of
Methadone in the Maintenance Treatment of Opioid Dependence.
Principles of methadone
dosing
• Induction
– Require slow induction (‘start low & go slow’)
– 20-30mg / day & increase dose by 5-10mg every
3 days until reach target dose (over 2-6 weeks)
• Maintenance
– Doses of 20 – 40mg prevent opiate withdrawal
– Doses >60mg most effective in reducing heroin
use
• Withdrawal
– Gradual dose reductions (at rate of 10mg /
month)
Henry-Edwards et al (2003) Clinical Guidelines and Procedures for the Use of Methadone
in the Maintenance Treatment of Opioid Dependence.
Buprenorphine
• Partial agonist at the opioid receptor
- Low intrinsic activity only partially
activates receptors
• High affinity for the receptor
- Binds more tightly to receptors than
other opioids
- Developed in 1980s as analgesic
Classification of Opioids
100
Size of Opiate Agonist Effect.
.
Full Agonists: Heroin, morphine,
methadone, codeine
0
Threshold for respiratory
depression
Partial Agonists: Buprenorphine
Antagonists: Naltrexone, naloxone
Drug Dose
Lintzeris, N (2008). Unpublished data. Reprinted with permission.
Safety Aspects of BPN
• Less risk of overdose c/w full opiate
agonists
– Less respiratory depression & sedation than
methadone
– BPN ‘tolerated’ by individuals with low levels
of opiate dependence
• Potential concerns re: safety
– BPN related deaths reported in combination
with other sedatives (EtOH, BZDs) … BUT
less of a concern than other opiates (e.g.
methadone, heroin)
Clinical Pharmacology
• Sublingual tablets
– 0.4, 2 & 8 mg tablets available
– 3 to 10 minutes to dissolve
• Time course
– Onset: 30–60 min, peak: 1–4 hours
– Duration of action dose-related (1 dose / day)
• Side effects
– Typical for opioid class: less sedating than
methadone
• Withdrawal syndrome
– Milder than full agonists
Lintzeris et al (2006) National clinical guidelines and procedures for the use of buprenorphine in
treatment of opioid dependence.
Overview BPN Doses
Induction
• Delay first dose of BPN until early opiate withdrawal
• Commence 4 to 8 mg daily
• Frequent & rapid dose increases possible (by 2 to
8mg/day)
Maintenance
• Daily doses: 8 – 16mg (max 32mg) required initially
• Alternate day dosing possible for many clients
Withdrawal
• More rapid dose reductions possible than
methadone
(e.g. 2 – 4 mg / week usually well tolerated)
Lintzeris et al (2006) National clinical guidelines and procedures for the use of buprenorphine in
treatment of opioid dependence.
Buprenorphine-naloxone tablet
(Suboxone®)
• Sublingual tablet in 4:1 ratio (BPN:NLX)
• Naloxone (antagonist) poorly absorbed
sublingually & inactive
• Naloxone produces antagonist (withdrawal)
effects if tablet injected by heroin user
• Enables take-away doses with greater
convenience for patients & less risk of
tablet misuse
When should we stop
substitution treatment?
• Chronic condition needs long term treatment
– Premature cessation of treatment usually results in
relapse to dependent heroin use
• Consider ending treatment when:
–
–
–
–
No illicit drug use for months / years
Stable social environment
Stable medical / psychiatric conditions
Patient ‘has a life’ that does not revolve around
drugs
– Patient informed consent
• When do we stop anti
convulsants/antidepressants?
Common objections to
substitution treatment
• Swapping ‘one drug for another’
• Prolongs ‘addiction career’
• Methadone-related deaths (e.g. accidental
deaths in children)
• Cannot treat a bio-psycho-social condition
just with drugs
• Giving up on the ‘war on drugs’
• Form of ‘social control’ over minorities /
marginalised groups
Heroin Maintenance
• A controversial treatment approach
• Was limited to Britain until 1990
• Currently licensed and available for
prescription in several European
countries
• Usually prescribed IV injections of 300500mg/day in 3 divided doses
• Uncommon but serious side effects
– Seizures and respiratory depression
immediately following injection
Lintzeris N (2009) CNS Drugs, 23(6):463-476.
Heroin Maintenance (cont.)
• Effectiveness is comparable to methadone in
retaining patients in treatment and improving
health
• More effective than methadone in reducing
additional heroin use
• More expensive to deliver than methadone but
significant savings can be made in the criminal
justice sector
• The main rationale for heroin maintenance is
treatment of refractory patients who do not
respond to methadone or buprenorphine
treatment delivered under optimal conditions
Lintzeris N (2009) CNS Drugs, 23(6):463-476.
LAAM
• Levo-alpha-acetylmethadol (LAAM) is a
long acting congener of methadone.
• Two active metabolites are responsible
for most of the effect of LAAM
– nor-LAAM (half-life >30 hours)
– dinor-LAAM (half-life >100 hours)
• The parent drug (also active) and the
metabolites all have selective affinity for
the µ-opioid receptor
White JM and Lopatko OV (2007) Expert Opin Pharmacother., 8(1):1-11. Review
LAAM
• Administered as an oral solution
• LAAM can be administered every second day, or
3 times/week.
• At least as effective as methadone in opioid
maintenance treatment
• The parent drug was found to prolong QT interval
(a potential cause in cases of Torsades de
Pointes) and was subsequently withdrawn by the
manufacturer.
• There is the potential for the metabolite norLAAM to be used therapeutically, and for the reintroduction of LAAM with careful monitoring.
White JM and Lopatko OV (2007) Expert Opin Pharmacother., 8(1):1-11. Review
Selecting Treatment
Approaches
Selecting treatment modalities:
Evidence-based medicine
• Patient circumstances
– Patient goals & expectations of treatment
– Past history of what has worked before
• Available resources
– Treatment services available
– Cost of different treatment approaches
• Evidence regarding safety & effectiveness
Comparing outcomes & costs
Heroin use /
retention
Detox
<5% long term
abstinence
Mortality
Cost
? increase / no $1000 / week
change
3 – 4 fold
reduction
Maintenance
50% retention 1yr
25% no heroin use 1yr
Naltrexone
5-10% retention 1 yr. ? increase / no $4,000/year
change
Most drop outs relapse
Therapeutic
community
Few stay in Rx unless
++ motivation /
pressure
?
$10-15,000
Good retention rates
increase on
release
$40-70,000
Prison
Lintzeris, N (2008). Unpublished data. Reprinted with permission.
$3000 / year
Retention in treatment:
methadone, buprenorphine & LAAM vs.
naltrexone
Mattick RP et al. (2001) “National Evaluation of Pharmacotherapies for Opioid Dependence (NEPOD):
Report of Results and Recommendations”. National Drug and Alcohol Research Centre, Sydney.
© Commonwealth of Australia reproduced by permission.
‘Public health’ vs ‘Treatment’
models
The balance between
• Services oriented to ‘public health’ outcomes
– Increased numbers in treatment, general
reductions in drug use, mortality, HIV
transmission
– Low intensity & less expensive services
• Services oriented to maximise ‘treatment’
outcomes
– Comprehensive programs, more expensive,
fewer numbers
– Oriented towards rehabilitation
– Manage medical and psychiatric comorbidity
Conclusions
• Heroin dependence is a long term condition
• Long term conditions (e.g. heroin dependence) usually
require long-term interventions
• Public health response requires treatment approaches
that can be disseminated effectively & inexpensively
• Most treatment approaches work, as long as patients
remain in treatment
– Substitution treatment has greatest retention rates
for most patients & reduces harms associated with
heroin use
– Need range of treatment interventions to suit
different patients
Treating James ….
•
•
•
•
•
James is a 29 year old man with >10 yr history heroin use
Injects heroin 2-3 times a day
Part time-work & deals to support habit
Pregnant girlfriend using heroin infrequently
In treatment 4 times before …
– Relapsed after detox & rehab
• Presents with infected arm & ?endocarditis.
• Wants to stop using. Needs admission
• ………. detox … likely relapse
• ………. rehab … working & girlfriend pregnant
• .……… initiate BPN whilst in hospital, stabilise medical
condition & review treatment plans
Contributors
• Associate Professor Nicholas Lintzeris
Drug Health Services, SSWAHS
Central Clinical School, University of Sydney
• Dr Olga Lopatko
University of Sydney
All images used with permission, where applicable