Antibiotics
advertisement

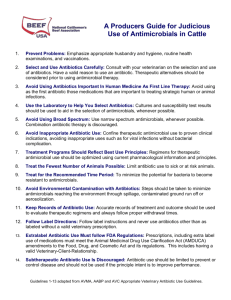
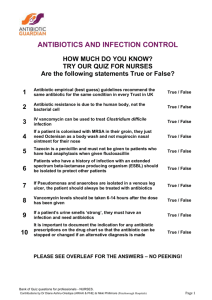
Treatment of Infection Professor Mark Pallen Treatment of Infection How Do Antimicrobials Work? • Key concept: selective toxicity – the antimicrobial agent blocks or inhibits a metabolic pathway in a microorganism which is either absent or is radically different in the mammalian cells of the human host Principle of antibiotic spectrum • Different antibiotics target different kinds of bacteria – i.e., different spectrum of activity • Examples: – Penicillin G (= original pen.) mainly streptococci (narrow spectrum) – Vancomycin only Gram-positive bacteria (intermediate spectrum) – Carbapenems many different bacteria (very broad spectrum) Treatment of Infection Anti-Microbial Drug Targets Antimicrobials acting on the bacterial cell wall • Interfere with synthesis of peptidoglycan layer in cell wall – eventually cause cell lysis – bind to and inhibit activity of enzymes responsible for peptidoglycan synthesis • aka “penicillin-binding proteins” Antimicrobials acting on the bacterial cell wall • Beta-lactams: Penicillins – – – – benzylpenicillin flucloxacillin ampicillin piperacillin a house with a garage R beta-lactam ring Antimicrobials acting on the bacterial cell wall • Beta-lactams: Cephalosporins – Orally active • cephradine • cephalexin – Broad spectrum • • • • cefuroxime cefotaxme ceftriaxone ceftazidime Cephalosporins a house with a garage & basement synthetic side chains change the spectrum of action Antimicrobials acting on the bacterial cell wall • Unusual beta-lactams – Carbapenems • Imipenem, meropenem – very wide spectrum – Monobactams • Aztreonam – only Gram-negatives • Glycopeptides – only Gram-positives, but broad spectrum – vancomycin – teicoplanin Antimicrobials acting on nucleic acid synthesis • Inhibitors Of Precursor Synthesis – sulphonamides & trimethoprim are synthetic, bacteriostatic agents • used in combination in co-trimoxazole – Sulphonamides inhibit early stages of folate synthesis • dapsone, an anti-leprosy drug, acts this way too – Trimethoprim inhibits final enzyme in pathway, dihydrofolate synthetase. • pyramethamine, an anti-toxoplasma and anti-PCP drug acts this way too Antimicrobials acting on nucleic acid synthesis • Inhibitors of DNA replication – Quinolones (e.g ciprofloacin) inhibit DNA-gyrase – Orally active, broad spectrum • Damage to DNA – Metronidazole (anti-anaerobes), nitrofurantoin (UTI) • Inhibitors of Transcription – rifampicin (key anti-TB drug) inhibits bacterial RNA polymerase – flucytosine is incorporated into yeast mRNA Antimicrobials acting on protein synthesis • Binding to 30s Subunit – aminoglycosides (bacteriocidal) 30s subunit mRNA • streptomycin, gentamicin, amikacin. – tetracyclines • Binding to the 50s subunit – chloramphenicol – fusidic acid – macrolides (erythromycin, clarithromycin, azithromycin) 50s subunit protein Antimicrobials acting on the cell membrane • amphotericin binds to the sterol-containing membranes of fungi • polymyxins act like detergents and disrupt the Gram negative outer membrane. – Not used parenterally because of toxicity to mammalian cell membrane • fluconazole and itraconazole interfere with the biosynthesis of sterol in fungi Mechanisms of resistance • Resistance can arise from chromosomal mutations, or from acquisition of resistance genes on mobile genetic elements – plasmids, transposons, integrons • Resistance determinants can spread from one bacterial species to another, across large taxonomic distances • Multiple resistance determinants can be carried by the same mobile element – Tend to stack up on plasmids Impact of antibiotic resistance • Infections that used to be treatable with standard antibiotics now need revised, complex regimens: – e.g., penicillin-resistant Strep. pneumoniae now requires broad-spectrum cephalosporin • In some instances, hardly any antibiotics left: – e.g., Multiresistant Pseudomonas aeruginosa – e.g., Vancomycin-resistant Staph. aureus • Resistance rates worldwide increasing Mims C et al. Medical Microbiology. 1998. Mechanisms of resistance • Enzymes modify antibiotic – widespread, carried on mobile elements • beta-lactamases • chloramphenicol-modifying enzymes • aminoglycoside-modifying enzymes • Permeability – antibiotic cannot penetrate or is pumped out • chromosomal mutations leads to changes in porins • efflux pumps widespread and mobile Mechanisms of resistance • Modification or bypass of target – by mutation or acquisition of extrinsic DNA – S. aureus resistance to flucloxacillin • acquires an extra PBP2 to become MRSA – S. aureus resistance to mupirocin • Chromosomal mutations in low-level resistance • Plasmid-borne extra ILTS gene in high-level resistance – Rifampicin resistance in M. tuberculosis • Point mutations in RNA polymerase gene Antibiotic susceptibility testing in the laboratory • Bacterial cultures tested on artificial media • Tests the ability to grow (or: be killed) in the presence of defined antibiotics • Provides guidance for ongoing therapy • Provides resistance rates for empiric therapy • Problems: not all results correspond with clinical success or failure Determination of MIC and MBC Mims C et al. Medical Microbiology. 1998. Disk diffusion testing Cohen & Powderly 2004; http://www.idreference.com/ Questions to ask before starting antibiotics • Does this patient actually need antibiotics? • What is best treatment? – – – – – What are the likely organisms? Where is the infection? How much, how often, what route, for how long? How much does it cost? Are there any problems in using antibiotics in this patient? • Have you taken bacteriology specimens first?! Clinical use of antibiotics Gillespie SH & Bamford KB. 2003. Medical microbiology & infection at a glance. Does this patient need antibiotics? • Is the patient even infected? – e.g. urethral syndrome vs UTI • Is it a viral infection? – e.g. the common cold • Is the infection trivial or self-limiting? – most diarrhoea • Are there more appropriate treatments? – physiotherapy for bronchitis – treatment of pus is drainage – treatment of foreign body infection is removing the foreign body Best antibiotic(s) for these organisms …? • For some organisms sensitivities are entirely predictable – e.g. Streptococcus pyogenes always penicillin-sensitive • For most organisms, sensitivity tests contribute to rational therapy – e.g. coliforms in UTI • Knowledge of local resistance problems contributes to choice of empirical therapy Best antibiotic(s) for this site of infection …? • Depends on penetration of antibiotic into tissues – e.g. gentamicin given iv does not enter CSF or gut – E.g. azithromycin accumulates in cells even though levels low in serum • Depends on mode of excretion – e.g. amoxycillin excreted in massive amounts in urine Are there any problems with this regimen in this patient? • Allergy – usually only a problem with penicillins, and, less often, with cephalosporins (~10% cross sensitivity) • Ampicillin Rash – develops if patient has glandular fever or lymphoma – Not related to general penicillin allergy Are there any problems with this regimen in this patient? • Side Effects • some occur with almost any antibiotic – Gastric upset – Antibiotic-associated diarrhoea • C. difficile infection • pseudo-membranous colitis an be fatal – Overgrowth of resistant organisms • “Thrush” in the community • VRE’s, MRS A s, Candida in ITU Are there any problems with this regimen in this patient? • Organ-specific side effects • damage to kidneys, ears, liver, bone marrow – chloramphenicol produces rare aplastic anaemia – vancomycin can cause "red man syndrome" – rifampicin discolours tears, urine contact lenses, can cause "flu-likesyndrome" – erythromycin causes gastric irritation – ethambutol can cause ocular damage – Aminoglycosides and vancomycin can cause ear and kidney damage Are there any problems with this regimen in this patient? • Care needed in patients with metabolic problems – renal failure – liver failure – genetic diseases • Drug interactions – e.g. gentamicin and frusamide • Use in pregnancy, breast feeding, children • Check in the BNF! Other Questions to Ask • • • • How much? How long for? How frequently? What route? – In general, you should avoid “overdoing it” Microbiologists spend as much time telling people when to stop antibiotics as when to start! – Switch from i-v to oral therapy as soon as you can – Treat UTIs for just three days