PowerPoint-Präsentation
advertisement

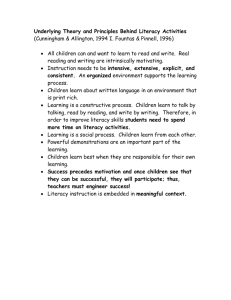
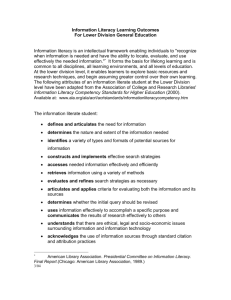
Further Developing concept and tools of the Health Literate Health Care Organization using HPH, HLS-EU and quality management methodology Jürgen M. Pelikan, Christina Dietscher, Jakob Lorenc Ludwig Boltzmann Institut Health Promotion Research, WHO-CC Health Promotion in Hospitals and Health Care LBIHPR: A-1020 Vienna, Untere Donaustraße 47, Austria | office@lbihpr.lbg.ac.at | www.lbihpr.lbg.ac.at | +43 1 2121493 -10 | FAX - 50 Like literacy, health literacy is a relational concept Source: Parker, 2009 Skills/Abilities X Demands/Complexity = Health Literacy Health Literacy Equation: Source: Brach 2013 Health Literacy = f (Personal Skills/Abilities, Situational Demands/Complexity) Source: Pelikan 2013 (in tradition of Kurt Lewin) Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 2 How can health literacy be understood? – 4 elements of a comprehensive definition used for the HLS-EU survey (Sorensen et al 2012) 1) What is the core of health literacy? 2) What general literacies does health literacy build up on? A resource for decisions of relevance to health HL Specific General Science, media, IT literacy (etc.) Knowledge (on health / disease) Health literacy Motives (on health / disease) Basic literacy and numeracy (PIACC, PISA) Competences (health knolwedge management) Proficiency in local language & culture in country of residence 3) What specific competences are needed to manage health related knowledge and information? 4) What health-related decisions and actions is health literacy needed for? To … Access Understand Appraise Apply Health Care Health-related information (Source: Sorensen et al. 2012) Disease prevention Health promotion Find / access: in data sources or by asking lays / experts Understand: texts / spoken language / pictures, tables, graphs Appraise: quality of information / of information source Apply: in own context / situation Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 3 2.1 Health Literacy as a Comprehensive Concept – Integrated Model and Definition of Health Literacy for the HLSEU Study (Sorensen et al. 2012) “Health literacy is linked to literacy and encompasses people’s knowledge, motivation and competences to access, understand, appraise, and apply health information in order to make judgments and take decisions in everyday life concerning healthcare, disease prevention and health promotion to maintain or improve quality of life during the life course.” Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 4 Low Health Literacy Levels are considerable & vary by Country! Percentage Distributions of Comprehensive HL Levels, for Countries and Total Sample (HLS-EU 2012) inadequate comp.-HL Netherlands 1.8% 10.3% Poland 10.2% 29.7% 11.0% TOTAL 12.4% Spain 0% 38.2% 30% 16.5% 33.7% 9.9% 32.6% 35.2% 20% 19.6% 36.0% 50.8% 10% 15.6% 34.1% 35.2% 26.9% 19.5% 39.6% 35.3% 7.5% 21.3% 35.9% 30.9% 18.2% Bulgaria 25.1% 38.7% 34.4% Germany excellent comp.-HL 46.3% 13.9% Austria sufficient comp.-HL 26.9% Ireland Greece problematic comp.-HL 40% 50% 26.6% 60% 70% 80% 9.1% 11.3% 90% 100% AT [N=996] BG [N=955] DE (NRW) [N=1041] EL[N=998] ES[N=981] IE[N=972] NL[N=993] PL[N=946] TOTAL [N=7883] Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 5 Examples for strengthening health literacy-friendly settings Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 6 Why is health literacy of patients important within the health care system? In the health care system health is restored by co-production (not by „compliance“!) of patients and health professionals, based on partnership in diagnosis and therapy by Shared Decision Making Collaboration in actions Requirements for co-production are Sufficient competence (i.e. health literacy of patients) for decision-making & ability to cooperate These requirements have to be guaranteed by representatives of the health care system by Enablement, empowerment & participation of patients This is necessary for normative reasons (patient rights & patients expectations etc.), for practical reasons, since co-production serves the evidence-based quality of health care (effectiveness, efficacy & sustainability). Better suitable entry to the professional health care system Better collaboration of patients regarding diagnosis & therapy Better diagnosis Better compliance in therapy Less medical errors Less clinical costs Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 7 Health literacy is important in different stages of a patient´s career 1. For healthy living: appraisal and taking into account of health risks & health resources continuously in everyday life 2. For entry to sick role: observation & appraisal of symptoms of disease 3. In sick role: Decision on self care/ use of the professional health care system 4. For entry to patient role: Decision to use of specific institutions of health care system (navigating the system) 5. In acute patient role: Description of symptoms and own life situation (& ability to ask relevant questions) during anamnesis, medical round, exit interview 6. In acute patient role : Cooperation in diagnostic tests 7. In acute patient role : Cooperation in therapy within and outside the health care system (shared decision making; compliance) 8. For role of chronic patient: self-management capacity to live a healthy life with a chronic condition Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 8 How can health literacy be integrated into health care and what specific difference does it make? Health literacy emphasizes the relevance and conditions of information & communication & decisions of all involved parties for the processes & results of health care Concerning Health Care HL is Concerning Quality HL is a developable & measurable, individual & organizational resource, which is an input as well as an output of processes & results in health care with a strong link to the concepts of shared decision making & self-care-management. A specific measurable quality of individuals and systems with a strong link to the concepts of effectiveness and efficacy resp. of user-/patient-orientation and employee-orientation Concerning Health Promotion (and Public Health) HL is A measurable core concept of HP applicable to individuals & settings with a strong link to other core concept of HP like empowerment (enablement) & participation, social determinants of health Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 9 A first proposal for a whole-systems HL approach Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 10 The concept of a health literate health care organizations „A health literate organization makes it easier for people to navigate, understand, and use information and services to take care of their health.” (Brach et al. 2012) Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 11 Ten attributes of health literate healthcare organizations (and systems) (Brach et al. 2012): A HL organization … 1. Has leadership that makes HL integral to its mission, structure, and operations 2. Integrates HL into planning, evaluation, patient safety, quality improvement 3. Prepares the workforce to be HL and monitors progress 4. Includes populations served in the design, implementation, and evaluation of health information and services 5. Meets the needs of populations with a range of HL skills & avoids stigmatization 6. Uses HL strategies in interpersonal communications and confirms understanding at all points of contact 7. Provides easy access to health information and services & navigation assistance 8. Designs / distributes print, audiovisual, social media content that is easy to understand and act on 9. Addresses HL in high-risk situations, including care transitions and communications about medicines 10. Communicates clearly what health plans cover and what individuals will have to pay for services Specific to HL Relating to specific HP principles Change / quality / risk management Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 12 The current HLO approach – yes, but … Inductively developed approach without a clear theoretical background Focused mainly on outcomes of clinical care with potential to expand the HLO impact by also addressing future decisions in relation to healthcare, self management and health-related choices in daily life Focused on patients only Insufficiently connected to other healthcare reform approaches such as quality, Health Promoting Hospitals Strongly driven by US healthcare context – legal and financial incentives such as capitation-based healthcare financing not automatically applicable to other contexts Need for further development Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 13 Learning from quality Clear differentiation between structures, processes and outcomes needed important for defining indicators, supporting measurement and continuous further development Build capacities to support CQI of HLO Focus on staff not only as service providers but as target group themselves Development of comparable indicators / standards to support learning and exchange across organizations Benchmarking Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 14 Learning from Health Promoting Hospitals and other health promotion settings In addition to focusing on cure and care, include also: Living in the hospital Future disease prevention Future health promotion not only compensate low health literacy but actually empower for better health literacy Expand target groups from patients to also Staff Community Adapt concept to local healthcare system and strategies – establish conceptual links to liaise with potential allies Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 15 Our proposal for a comprehensive whole-sale (health promoting) HLO concept Health literacy for … Acessing, living and working in the hospital Diagnosis, cure and care Disease prevention Health promotion Patients Staff Community 3 Support navigation and on-site healthy choices 4 Support healthy decisions in diagnosis, cure, care 2 Foster communication competence of staff 7.1 Support continuity and cooperation 5 Support future decisions in relation to prevention, selfcare and health promotion 6 Support future decisions in relation to prevention, selfcare and health promotion 7.2 Support future decisions in relation to prevention, selfcare and health promotion Organizational structures and processes 1 Developing a HLO management policy and supportive organizational structure 8 Involve target groups in the development and evaluation of communication strategies and tools 9 Support concept dissemination Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 16 The ISQUA process for standard development 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. Establishing need for new standards, priorities Relationships with other standards considered Standards development plan Standards based on research, guidelines, technical input Involvement of interested parties in development process Clear scope and purpose of standards Clear standards framework Clear wording of standards Testing/Piloting of standards Approval of standards by standards setting body Information and education to users and assessors Timeframes, transitional arrangements for implementation Satisfaction with standards monitored, data evaluated Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 17 Further information on health literacy concepts at this conference Plenary 2 (Thursday, 09.00-10.30): Health literacy – an emerging concept for more patient-oriented healthcare Rima Rudd (Harvard): Health Literacy – an Emerging Concept for More Patient-Oriented Healthcare Rosa Suñer (HL working group, HPH Catalunya): Making healthcare organizations more healthy – Literacy settings for patients Hans Kluge (WHO-Euro): The contribution of health literacy to patient safety Session O1.1 (Thursday, 11.00-12.30): Developing health literate healthcare systems and organizations Further Developing concept and tools of the Health Literate Health Care Organization using HPH, HLS-EU and quality management methodology? (Pelikan, Dietscher, Lorenc) Health Literacy, Chronic Illness, and Use of Primary, Secondary and Tertiary Healthcare - Making the Case for Health Literate Organizations (Levin-Zamir, Baron-Epel, Elhayany) A Path to becoming a Health Literate Organization: Lessons Learned from the Experience of a Public Health Authority in Canada (Massé, Lemieux) Health Literacy as a system strategy in Emilia-Romagna (Gazzotti, Ricco, Chiarenza, Ruozi) Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 18 References & Resources Brach, C., Keller, D., Hernandes, LM., Baur, C., Parker, R., Dreyer, B., Schyve, P., Lemerise, AJ., Schillinger, D. (2012): Attributes of Health Literate Organization, Discussion Paper, Institute of Medicine of the national academies. http://www.iom.edu/~/media/Files/Perspectives-Files/2012/DiscussionPapers/BPH_HLit_Attributes.pdf Brach, C. (2013): Becoming a Health Literate Organization: Tools for Community Health Centers. Presentation 3.April 2013 at the Center for Delivery, Organization and Markets. DeWalt, D.A., Callahan, L.F., Hawk, V.H., Broucksou, K.A., Hink, A., Rudd, R. & Brach, C. (2010). Health Literacy Universal Precautions Toolkit. (Prepared by North Carolina Network Consortium, The Cecil G. Sheps Center for Health Services Research, The University of North Carolina at Chapel Hill, under Contract No. HHSA290200710014.) AHRQ Publication No. 10-0046-EF) Rockville, MD: Agency for Healthcare Research and Quality. Kickbusch,I., Maag, D. (2008): Health Literacy. In: Heggenhougen,H.K., Quah,S.R. (Eds.), International Encyclopedia of Public Health, Vol. 3. (pp.204-211). San Diego: Academic Press. Kickbusch I, Pelikan J M, Apfel F, Tsouros A D (Eds.) (2013): Health literacy. The solid facts. Copenhagen: Copenhagen: World Health Organization – Regional Office for Europe. http://www.euro.who.int/__data/assets/pdf_file/0008/190655/e96854.pdf Levin-Zamir, D, Peterburg Y. (2001): Health literacy in health systems – perspectives on patient self-management Health Promotion International,16;1:87-94. Nutbeam,D. (2000): Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 15 (3), 259-267. Nutbeam,D. (2008): The evolving concept of health literacy. Social Science & Medicine, 67 (12), 2072-2078. Parker, R. in World Health Communication Association (2009): Health Literacy, Part 1 „The Basics“. WHCA Action Guide. Pelikan,J.M., Dietscher,C., Schmied,H. (2013): Health Promotion for NCDs in and by Hospitals: A Health Promoting Hospital Perspective. In: McQueen,D. (Ed.), Global Handbook on Noncommunicable Diseases and Health Promotion (pp.441-460). New York, Heidelberg, Dordrecht, London: Springer. Pleasant, A. & Kuruvilla, S. (2008): A tale of two literacies: public health and clinical approaches to health literacy. Health Promot. Int. 23(2) 152-159. Rudd,R. (2005): Navigating Hospitals: Literacy Barriers. Literacy Harvest Rudd, R.E. & Anderson, J.E. (2006).The Health Literacy Environment of Hospitals and Health Centers – Partners for Action: Making your healthcare facility literacy-friendly. National Center for the Study of Adult Learning and Literacy and the Health and Adult Literacy and Learning Initiative, Harvard University School of Public Health. Sorensen,K., Broucke,S., Fullam,J., Doyle,G., Pelikan,J., Slonska,Z., Brand,H., (HLS-EU) Consortium (2012): Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12 (80). WHO (1986): Ottawa Charter for Health Promotion. In World Health Organization (Ed.), Geneva: WHO. WHO (1998): Health promotion glossary. Geneva: WHO Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 19 THANK YOU FOR YOUR ATTENTION! Jürgen M. Pelikan Christina Dietscher juergen.pelikan@lbihpr.lbg.ac.at christina.dietscher@lbihpr.lbg.ac.at Pelikan, J.M., Dietscher, C. Lorenc, J. (2014): 22nd International HPH Conference Barcelona, April 23-25, Health-Literate Organization 20