Cushing's, Addison's And Acromegaly
advertisement

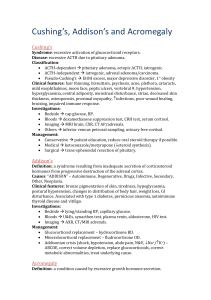
Cushing’s, Addison’s and Acromegaly Dr Edward Hutchison FY1 (Geriatrics) Phase II Objectives • 3.21: Investigations – o Request appropriately the more common tests of thyroid, adrenal and pituitary gland function, seeking advice where necessary. • 3.23: Adrenal gland hormones o Recognise signs and symptoms of Addison’s disease, confirm diagnosis and initiate immediate management of Addisonian crisis. o Recognise symptoms and signs of Cushing’s syndrome, confirm diagnosis, participat in management of Addison’s disease and Cushing’s syndrome. • 3.24: Pituitary gland hormones o Recognise the circumstances when hypopituiarism might occur, recognise possibility of hypopituitism with ‘non-specific’ symptoms, investigate causes. o Initiate investigation for posterior pituitary function in patients with polyuria. o Recognise acromegaly, initiate investigation for acromegaly, outline to patients the possible treatments for acromegaly. Aims • • • • • HPA Axis Adrenal glands Cushing’s syndrome/disease Addison’s Acromegaly HPA Axis Hypothalamus GnRH TRH Dopamine CRH GHR H Pituitary Sphenoid sinus ACTH GH FSH Anterior Pituitary Hormones TSH PRL LH ADH Posterior Pituitary Hormones Oxytocin Adrenal Glands Remember: GFR! Functions of Cortisol? • • • • • • • • • Insulin resistance/gluconeogenesis Protein catabolism Immunosuppresion CVS regulation – e.g. increasing BP CNS actions – e.g. increased appetite, impaired memory Increased bone turnover Gastric acid secretion Reduced skin collagen Fluid retention Right, now onto the stuff you actually want to know… Cushing’s… Which is which? Syndrome • Excessive activation of glucocorticoid receptors. Disease • Excessive production of ACTH caused by a pituitary adenoma. Classification ACTH-dependent Pituitary adenoma Ectopic ACTH production – e.g. small cell lung cancer, neuroendocrine tumours Iatrogenic – ACTH therapy ACTH-independent Iatrogenic – steroid therapy Adrenal adenoma/carcinoma Pseudo-Cushing’s EtOH excess Major depressive disorder Primary obesity Clinical features Symptoms • • • • • Depression Confusion Weight gain Poor glucose control (diabetics) Weakness rising from a chair (proximal myopathy) Investigation Overnight dexamethasone suppression test/ 24hr urinary cortisol Not excluded 48hr low-dose dexamethasone suppression test Confirmed Abstinence ?EtOH excess ACTH level? ACTH level High Low/normal CRH test/48hr dexamethasone suppression test Adrenal cause Suppressed MRI pituitary Not suppressed Ectopic source CXR, CT A/P, tumour markers CT adrenals ±adrenal venous sampling Management Conservative Medical Surgical Patient education Reduce oral steroid therapy if possible Inhibit biosynthesis of corticosteroids – e.g. ketoconazole and metyrapone Trans-sphenoidal resection of pituitary (requires lifelong hormone replacement). Laparoscopic resection of adrenal tumour. Ectopic ACTH: treat underlying cause ±bilateral adrenalectomy. Untreated Cushing’s disease has a 50% 5 year mortality Remember • Not only oral corticosteroids can cause Cushing’s syndrome, large amounts of topical and inhaled steroid may be absorbed into the systemic circulation. • Patients on large amounts of oral corticosteroids will require their dose to be tapered slowly to avoid an Addisonian-like crisis. • You also will need to manage the effect of longterm steroid therapy – e.g. diabetes, hypertension, thin skin, osteporosis. Addison’s disease (Or adrenal insufficiency, to be more correct). Definition? A syndrome resulting from inadequate secretion of corticosteroid hormones from progressive destruction of the adrenal cortex. Causes – autoimmune (90% of cases) – degenerative (amyloid) – drugs (e.g. ketoconazole) – infective (TB, HIV) – secondary (ACTH, hypopituitism) – other (e.g. adrenal bleeding) – neoplasia (metastases) Clinical Features Investigations Test Bedside Lying/standing BP Bloods U&Es – low Na+/high K+ Glucose – low Random serum cortisol Short synacthen test Plasma renin TFTs etc (?hypopituitism) FBC (?perncious anaemia) Gonadal function HIV test Plasma aldosterone Imaging AXR (?adrenal calcification CT or MRI of adrenals The short synacthen test • Why do we do it? • How do we do it? • What result do we see in a positive test? (Ruling out Addison’s) 250µg synacthen IM Positive test (ruling out Addisons): Serum Plasma cortisol >460nmol/L at cortisol 30 at 0 minutes minutes Serum cortisol at 30 minutes Management • Glucocorticoid replacement o Hydrocortisone BD, usually 15mg on waking/5mg around 1800hrs o Excessive weight gain = over replacement o Educate patient – increase hydrocortisone when unwell • Mineralocorticoid replacement o Fludrocortisone 50-100µg daily o Titrate according to symptoms and U&Es Addisonian Crisis Features: • Severe shock – hypotension, tachycardia • Fever, abdominal pain, nausea & vomiting • Hyponatraemia/hyperkalaemia ±hypercalcaemia, hypoglycaemia Management: ABCDE assessment • Correct volume depletion • Replace glucocorticoids • Correct metabolic abnormalities • Treat underlying cause Acromegaly Definition? • A condition caused by excessive secretion of growth hormone Most common cause? • Pituitary macroadenoma Impress your examiner… Hypopituitism Investigations Bedside Collateral Hx Serial photographs BP ECG Bloods Serum GH (unreliable) Oral glucose tolerance test Serum IGF-1 TFTs/FSH/LH/PRL etc Imaging CT/MRI brain Echo Other Colonoscopy Management • Conservative: o Patient education • Medical (second line): o Somatostatin analogues (octreotide, lanreotide) o Dopamine agonists o GH receptor antagonists (pegvisomant) • Surgery (first line): o Trans-sphenoidal surgical debulking of pituitary adenoma • Radiotherapy: o Employed if acromegaly persists after surgery References • • • • • • • • • • • • • • • • • • • Walker, BR., Colledge, NR., Ralston, SH., “Davidson’s Principles of Clinical Medicine” 21st edition, Churchill Livingstone, (2010). Kumar, P., Clarke, M. “Clinical Medicine” 7th edition, Saunders, 2009. Longmore, M. et al “Oxford Handbook of Clinical Medicine” 8th edition, Oxford University Press, 2010. http://www.fipapatients.org/pictures/big/pituitary_normal.jpg http://www.autismpedia.org/wiki/images/b/b9/Adrenal-core.gif http://www.ghorayeb.com/files/Transsphenoid_Lateral_380x332.jpg http://www.nosleeplessnights.com/wp-content/uploads/2013/03/dexamethasone.jpg http://classconnection.s3.amazonaws.com/319/flashcards/1117319/jpg/addisons_disease1332524676283.jpg http://upload.wikimedia.org/wikipedia/commons/2/2e/Addisons_hyperpigmentation.jpg http://globalvoicesonline.org/wp-content/uploads/2012/05/syringe-drawing-320x300.jpg https://lh5.googleusercontent.com/qF8wwWfCtFI/TXRv47Ax4xI/AAAAAAAABR8/4jsTaDOngtc/s1600/Synacthen.JPG http://www.gloshospitals.org.uk/SharePoint11/Pathology%20Web%20Images/Specimen%20containers/Gold_top_ with_cap.jpg http://www.sehha.com/diseases/endocrine/Addison12.gif http://www.hdwallpapersinn.com/wp-content/uploads/2012/09/bigshow-img.jpg http://www.examiner.com/images/blog/wysiwyg/image/andre-the-giant.jpg http://upload.wikimedia.org/wikipedia/commons/1/15/Bitempvf.png http://www.s2c8.co.uk/wp-content/uploads/2013/01/man-boob.jpg http://www.physio-pedia.com/images/6/61/Moon_facies_in_Cushings.jpg http://www.passpaces.com/images/acromegaly_MRCP.jpg