DRUGSTORAGESYSTEM - National Orthopaedic Hospital
advertisement

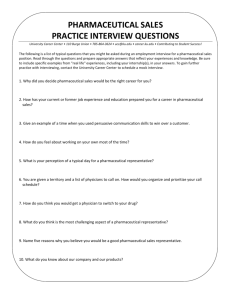
DRUG STORAGE SYSTEM IN A HOSPITAL SETTING PHARMACY DEPARTMENT NATIONAL ORTHOPAEDIC HOSPITAL, DALA-KANO 28th OCTOBER, 2015 DRUG STORAGE SYSTEM IN A HOSPITAL SETTING BY PHARM. KINGSLEY ETUMUDON OUTLINE 1.0 INTRODUCTION 1.1 DEFINITION OF TERMS 1.2 AIMS AND OBJECTIVES OF DRUG STORAGE IN THE HOSPITAL 1.3 STORAGE AREA 1.4 EFFECTS OF ENVIRONMENTAL FACTORS ON DRUG STORAGE 1.5 CONCLUSION INTRODUCTION Drugs are chemical substances with diverse Pharmacological actions. They bring about different changes in the body when they interact with biological systems. They may cause contraction, dilation of muscles, alteration of hormonal levels, and secretion from glands, modulation of nervous activity and a host of other Physiological changes. It can also be used for the prevention, diagnosis and treatment of diagnosed diseases and for the relieve of symptoms. In as much as drugs brings about changes in the body, drugs can undergo changes if not properly secured and stored under appropriate conditions. Drug storage is among the Pharmacist’s most important responsibilities. Therefore, adequate methods to ensure that these responsibilities are met, must be developed and implemented. DEFINITION OF TERMS 1. Contamination: -This is the undesired introduction of impurities of chemical or microbiological nature, or of foreign matters, into or onto a starting material or intermediate or finished product during production, sampling, packaging or repackaging, storage or transports. 2. Expiry Date:- The date given on the individual container (usually on the label) of a drug product up to and including when the product is expected to remain within specification, if stored correctly., example if the expiry date is Oct. 2015, it means the drug should not be used by the end of October. 3. Labeling:- The action involving the selection of the correct label, with required information, followed by line clearance of application of label. 4. Pharmaceutical Product:- Any medicine intended for human use or veterinary product administered to food producing animals, presented with its finished dosage form or as a starting material for use in dosage forms subject to control by Pharmaceutical legislation in both exporting and importing states. 5.Storage:- The act of storing of Pharmaceutical product and materials up to their point of use. 6. Shelf–Life:- Is the length of time a drug or commodity may be stored without becoming unfit for use. WHAT IS DRUG STORAGE Drug storage is the conditions under which Pharmaceutical products and materials are kept to ensure their stable forms are retained up to the point of use or till it reaches the consumer. The loss of potency during storage may influence the efficacy and safety of Pharmaceuticals. Pharmaceutical product required control storage and transit conditions in order to ensure their quality is not compromised. Storage is an important aspect of total drug control system. Proper environment control, that is proper temperature, light and humidity, Condition of sanitation, ventilation and segregation must be maintained whenever drugs are supplied and stored in the hospital. Pharmaceutical products are to be stored under conditions that prevent contamination and as far as possible from deterioration. It could be said that, drug storage is one of the fundamental concern of Pharmacist in patient care. The conditions under which drugs are manufactured and stored can have a major impact on their quality. High temperature and relative humidity are the most important factors involved in drug degradation, and these environmental factors can all have a significant impact on the final quality of drugs and therefore, affect the Salability. All medicinal products must be stored in accordance with the manufacture’s directions and within the terms of product authorizations. Pharmaceutical stock should be stored under suitable conditions appropriate to the nature and stability of product concerned. Particularly, attention should be paid to protection from contamination, sunlight, uvrays, moisture, atmospheric moisture and extreme temperatures. Also, human factors should be checked and controlled by avoiding clumsy arrangements, food should not be stored where drugs are kept and also, ensure proper sanitation. During storage, drugs should be retained in the manufacture’s original packaging. Good storage practice is applicable in all circumstances where Pharmaceutical products are stored throughout distribution process. AIMS AND OBJECTIVES OF DRUG STORAGE IN HOSPITAL To ensure drug safety and maintenance of its integrity throughout its shelf life. To prevent wastage Protect from pilferage/theft. Secure drugs from an unauthorized persons, so that the conditions of storage are not tampered with. To protect the health of the public (to avoid contamination). Prevent infestation of pests and vermin (any of the common types of insects or animals which causes harm), e.g. flies, lice, mice and rats. Importantly, to promote patient care and improve quality of life. STORAGE AREA Storage area should be of sufficient capacity to allow orderly arrangement of the various categories of materials and products like startup and packaging materials, intermediate, bulk and finished products. Products in quarantine, released, rejected, returned or recalled products. Storage areas should be designed or adapted to ensure good storage conditions in particular. They should be clean, dry and maintained within acceptable temperature limits. Where special storage are required (e.g. temperature and humidity) these should be provided, checked and monitored. Receiving and dispatch bays should protect materials and products from the weather. Where quarantine status is ensured, storage is in a separate area, such area must clearly marked and their access restricted only to authorized personnel. THE EFFECTS OF ENVIRONMENTAL FACTORS ON DRUGS STORAGE Ingredients in a Pharmaceutical preparations, either the active ingredients or pharmaceutical excipients can be affected by some environmental factors which can affect the stability of the drug or dosage form. TEMPERATURE:- High temperature accelerate oxidation, reduction and hydrolysis which lead to drug degradation. HUMIDITY/MOISTURE:- Water catalyzes chemical reactions as oxidation, hydrolysis and reduction reaction. It also promotes microbial growth. These effects causes instability problems on different formulation as highlighted below: a). Oral solutions: the instability problems are: Loss of flavour. Change in taste. Presence of off flavours due to interaction with plastic bottle . Loss of dye. Precipitation. Discolouration. b). Parenteral solutions:- Interaction of the contents with container and changes in chemical composition. Instability problems: Discolouration Presence of precipitate due to interaction with container. Clouds: Cloud will appear in the product due to: Chemical changes (an ester, e.g. polysorbate may hydrolyses by producing an acid which is poorly soluble). - Effects: Change in appearance and in bioavailability. c). Suspensions:- Instability problems Settling. Caking. Crystal growth. Effects: Loss of drug content uniformity in different doses from the bottle and loss of elegance. d). Emulsions:- Instability problems Creaming Cracking. Phase invasion Effects: Loss of drug content uniformity in Different doses from the bottle and loss of elegance. e). Tablets:- Instability problems Disintegration time. Dissolution profile. Hardness. Appearance. Effects: Change in release. f). Capsules:- Instability problems Change in appearance. Dissolution. Strength. Effects: Change in drug release. Finally, maintaining proper storage conditions at hospital is essential to reduce such impact caused by environmental factors. The Pharmaceutical products will retained their potency when stored in Pharmacies having good storage facilities. Hence, there is need to highlights the importance of maintaining good storage condition in the hospital Pharmacy. Also, to ensure that drugs still retain their stable form even after hospital storage to the point when it reaches the consumer. The Pharmacist plays a role as part of his responsibilities to counsel the patient on the importance of proper drug storage he/she is given. WORLD HEALTH ORGANISATION GUIDELINES ON STORAGE OF PHARMACEUTICAL PRODUCTS BY PHARM. SANI M. MUSTAPHA OUTLINE 1.0 INTRODUCTION 1.1 OBJECTIVE OF THE GUIDELINES 2.0 STORAGE PERSONNEL 3.0 STORAGE PREMISES AND FACILITIES 3.1 STORAGE AREA 3.2 STORAGE CONDITIONS 3.3 MONITORING OF STORAGE CONDITIONS 4.0 STORAGE REQUIREMENTS 4.1 DOCUMENTATION 4.2 STORAGE AND LABELLING CONDITIONS 4.3 NORMAL CONDITIONS 4.4 STOCK CONTROL 5.0 CONCLUSION WHO GUIDELINES TO GOOD STORAGE OF PHARMACEUTICAL PRODUCTS INTRODUCTION This WHO Guide is intended for those involved in storage, transportation distribution or sales Pharmaceuticals. It is closely linked to other existing guides recommended by the WHO Expert Committee on Specifications for Pharmaceutical preparations, such as: a. Good Trade Distribution Practice (GTDP) of Pharmaceutical starting materials. b. Good Manufacturing Practices (GMP). c. The cold chain especially for vaccines and Biologicals. d. The International Pharmacopoeia etc. The above guide was prepared in close collaboration with the International Pharmaceutical Federation (FIP). OBJECTIVE The objective of this guide is to supplement the above mentioned documents by describing the special measures considered appropriate for STORAGE and TRANSPORTATION of Pharmaceuticals. They may be adapted to meet individual needs where necessary, provided that the desired standards of quality are met. The guidelines are applicable to Manufacturers Importers Contractors Wholesalers Community Pharmacies Hospital Pharmacies NOTE: The guidelines may be adjusted in line with the type of activity where the storage of the Pharmaceuticals is taking place, but National or Regional Regulations must be followed. STORAGE PERSONNEL At each storage site (e.g. Hospital Pharmacy Store) there should be an adequate number of qualified personnel to achieve Pharmaceutical quality assurance objectives. National Regulations on qualifications should by followed (e.g. Registered Pharmacist must be incharge). All personnel should receive proper training in relation to good storage practice regulations procedures and safety. All members of staff should be trained in and observe high levels of personal hygiene and sanitation. Personnel employed in storage areas should wear suitable protective or working garments (e.g. Lab Coats or Overalls) appropriate for the activities they perform. STORAGE PREMISES AND FACILITIES STORAGE AREA Precautions must be taken to prevent unauthorized persons from entering storage areas (A notice may be put in place for this purpose). Storage areas should be of sufficient capacity to allow for orderly storage of various categories of Pharmaceutical products (including but not limited to received, rejected, dispatched or recalled products). Storage areas should be designed or adapted to ensure good storage conditions. They should be clean and dry. Maintained at acceptable temperature limits (depending on the products requirements). Where special conditions are required by the label (e.g. relative humidity), these must be provided, checked, monitored and recorded. Materials should be stored off the floor (pallets must be provided for heavy cartons, e.g. I.V fluids), and suitably spaced for easy cleaning and inspection. Pallets must be kept in good state, cleaned and repaired when broken. Storage areas must be kept clean from accumulated wastes and vermin (insects, pests, rhodents etc). A written sanitation programe should be available, indicating frequency of cleaning and methods. There should be written programe for pest control. Pest control agents should be safe, with no risk to contamination or cross-contamination of Pharmaceutical products. There should be appropriate procedures for cleaning of spillage to ensure complete removal to avoid contamination. Receiving and Dispatch bays should be available and should protect materials and products from whether, extreme temperatures and theft. There should be physical or other equivalent methods for validation (e.g. electronic, computerized) and seggregation of rejected, expired, recalled or returned products. Highly active radioactive materials, Narcotics and other Hazardous, sensitive and/or dangerous Pharmaceutical products, as well as substances which pose potential risks of abuse, fire or explosion should be stored in a dedicated area, with additional safety and security. Pharmaceutical products and materials should be stored in a manner that will prevent contamination, mix-ups, and crosscontamination. The “First Expired–First Out”(FEFO) principle should be followed. Narcotics should be stored in compliance with international conventions, National Laws and Regulations on Narcotics. Broken or damaged items should be separated and withdraw from usable stock. Storage Area should be adequately lighted to enable all operations to be carried out accurately and safely. STORAGE CONDITIONS Storage conditions for Pharmaceutical products should be in compliance with the LABELLING which is based on the results of stability testing. MONITORING STORAGE CONDITIONS Recorded Temperature monitoring date should be available for review (e.g. Wall Thermometers should be used to check internal temperatures at all times). All monitoring records should be kept for at least the shelf life of the stored product plus one (1) year, or as required by the National Legislation. Equipment for monitoring should be calibrated at defined intervals. STORAGE REQUIREMENTS DOCUMENTATION: Written Instruction and Records should be available, which documents all activities in the storage areas, including handling of expired stock. Permanent information, written or electronic, should exist for each stored product, indicating: Storage conditions, etc. Records must be kept for each delivery, and this should include: Description of goods. Quality. Quantity. Supplier. Supplier’s Batch Number. Receipt Date. Expiry Date. N.B:- This information is normally found on each drug Tally or Bin Card Where National Regulations require that records must be kept or retained for a certain period, this must be observed, otherwise such record should be retained for a period equal to the shelf-life of the material, plus one (1) year. Comprehensive records should be maintained showing all receipts and issues according to a specific system, e.g. by Batch Number. STORAGE AND LABELLING CONDITIONS NORMAL CONDITIONS: Storage in dry, well ventilated premises at temperatures of 15250c, or depending on climatic conditions, up to 300c. Extraneous odours, other indications of contamination, and intense light must be excluded. DEFINED STORAGE INSTRUCTIONS Drug products must be stored under defined conditions require appropriate storage instructions. Unless otherwise specifically stated (e.g. continuous maintenance of cold storage), deviation may be tolerated only during short term interruptions, (e.g. during local transportation). The use of the following Labeling instructions are recommended. ON THE LABEL - “Do not store over 300c - “Do not store over 250c - “Do not store over 150c - “Do not store over 80c - “Do not store below 80c - “Protect from Moisture”: WHAT IT MEANS From + 20c to + 300c From + 20c to 250c From + 20c to 150c From + 20c to 80c From + 80c to + 250c No more than 60% Relative Humidity in Normal Storage Conditions to be provided to the patient in moisture resistant container. - “Protect from Light”: To be provided to the patient in light Resistant container. STOCK CONTROL * Periodic stock reconciliation should be performed by comparing the actual (Physical) stock and the recorded stock (on the stock or Tally/Bin Card). *Each container should be carefully inspected for possible contamination, Tampering or damaged. All significant stock discrepancies should be investigated as a check against in advertent mix-ups and/or incorrect issue. Damaged containers should not be issued unless quality of the material is shown to be unaffected. Any action taken should be documented. All stock should be checked regularly for Obsolete and outdated products. Precautions should be taken to prevent the issue of outdated products. On receipt, each incoming deliver should be checked against the relevant purchase order and each container physically verified e.g. Label, Batch, Expiry Date, etc. Returned Goods: All returned goods, including recalled goods should be handled in accordance with approved procedure, and records should be maintained. DISPATCH AND TRANSPORTATION Pharmaceutical products should be transported in such a way that their integrity is not impaired and storage conditions are maintained. Special care should be used when cold chain is required. Devices should be used to monitor temperatures where necessary. Pharmaceuticals should be transported when receipt of delivery order is obtained and both dispatch and receipt must be documented. Records of dispatch should be retained, and should state at least -Dispatch Date. - Patient/Customers name and address. Product description (e.g. Name, Dosage form, strength etc). - Transport and Storage Conditions. All records should be accessible, available and readable. Finally, the World Health Organisation recommends that all stake holders in the Pharmaceutical Products Cycle should comply to some extent, with these recommended guidelines. Therefore, the hospital is no exemption. As we have seen, drug storage system does not solely rely on the storage area, but things like personnel, storage conditions, security, storage record as well as transportation of the product play a very important role in maintaining the integrity, efficacy and quality of the product up to the point of use. But even though institutions are expected to comply with such regulations and guides, they are by no means rigid, as there are room for customization and adaption by local bodies, depending on local regulations, as long as the standards and quality of the products are not impaired. DRUG STORAGE SYSTEM: THE NOHD EXPERIENCE BY PHARM. HAMZA ISA MUHAMMAD OUTLINE - PERSONNEL STORE ARRANGEMENT DRUGS ARRANGEMENT RECORD/QUARANTINE CHALLENGES CONCLUSION RECOMMENDATION PERSONNEL The Pharmacy store is over seen by a Single registered Pharmacist and strictly out of bounds to unauthorized persons. STORE ARRANGEMENT The store has fifteen aluminium shelves, arranged to make four rows to allow for easy access, cleaning as well as inspection. It has one fully functioning AC and the other partially functioning to maintain the drugs at room temperature and there is adequate lighting. DRUGS ARRANGEMENT The drugs are arranged on the shelves using a combination of Pharmacological and dosage form manner where by drugs are classified as Analgesic/Anti Inflammatory Agents, e.g. Aceclofenac, Diclofenac Sodium, Diclofenac Potassium, Ketoprofen, Meloxicam, Celecoxib and various dosage forms are segregated as Capsules, Tablets, Injections, Syrups, Creams/Ointments. - Antibiotics/Anti Infectives, e.g. Ciprofloxacin, Cefuroxime, Ceftriaxone, Levofloxacin, Clindamycin, Gentamicin. - Cardiopulmonary:-Antihypertensives – Amlodipine, Methyldopa, - Antidiabetics – Metformin, Glibenclamide, - Bronchodilators – Salbutamol inhaler. - Antimalarials – Artemeter/Lumefantrin, Artemeter Injection, Sulfadoxine/Pyrimethamine. - Antacids – Omeprazole, Ranitidine, Aluminium Hydroxide + Magnesium Hydroxide + Simethicone. - Vitamins/Minerals/Anti Oxidants, e.g Ascorbic acid, Calcitriol, Pyridoxine, Folic acid. - Anaesthetic Agents – Halothane, Isoflurane, Ketamine, Sodium Thiopentone. -Narcotics are kept in a dedicated area under lock and key, and are issued on request. The issues are recorded in a Poison/DDA register as required by law. -Thermolabile Drugs: Insulin, Vaccines (T. T. ATS). Bupivacaine, Propofol are kept in the refrigerator to maintain their temperature between 2 to 80c. - Intravenous Infusions, e.g. Normal Saline, 5% Dextrose water, 5% Dextrose Saline, 4.3% Dextrose Saline, Ringers Lactate, Mannitol, Darrows Solution are kept in a separate store on wooden pallets. The store is small in size but has functional Air-conditioning system. RECORDS/QUARANTINE All medicines coming into the Pharmacy are initially quarantined in a separate area (within the store) before they are checked for correctness of quantity, batch number, expiry dates, after necessary checks they are transferred to their respective storage locations. - Shelves are checked at a predetermined period (monthly) to ensure removal of medicines whose expiry date is approaching and the principle of FIRST EXPIRE–FIRST OUT (FEFO) during issuance is adhered to. When drugs are expired, they are being separated, to prevent mix up, and are subsequently burnt after approval by the Board of Survey. All relevant store records are being kept on the store documents SIV, SRV LEDGERS, BIN/TALLY CARDS, and there is periodic (monthly) Stock Taking. The department has other Units: Accident and Emergency, NHIS, SOPD, as well as INPATIENT in which the electricity coverage is inadequate, because the Air-conditions are switched off after the close of work. The units are without sufficient storage areas because they are smaller in capacity. CHALLENGES SPACE: The present store is too small (especially the IV fluid store) to adequately accommodate all the drugs, we are therefore having some storage space challenges. POWER SUPPLY: Sometimes the power supply is rationed and Pharmacy department is cut off. STAFF: There is only one pharmacist in the store and the department now has five units with nine (9) pharmacists which is grossly inadequate. LACK OF MONITORING EQUIPMENTS: Wall thermometer to monitor the temperature, and hygrometer to monitor the relative humidity. RECOMMENDATION - The general public should make sure that they obtain their drugs from the hospital Pharmacy/ Community Pharmacy where there is good storage facilities. The management should provide 24 hours power supply to the department and to allow us to put our AC’s on even after closing hours. The management to build a bigger store to accommodate all the drugs. The management to provide wall thermometer to monitor the temperature in the store. The hospital community and the general public should abide by the instructions given by the Pharmacist on the proper handling and storage of their medicines at home and in the ward. CONCLUSION Drugs serves as an important and integral products in the treatment and prophylaxis of many medical ailments of which they are required to be used at their maximum standard requirements, good Pharmaceutical storage is part of the quality management system that ensures the quality of the Pharmaceutical products. It is therefore the responsibility of Pharmacists and other health care providers to ensure that Pharmaceutical products are properly handled and stored and also adequately provided when required. THANK YOU ALL FOR LISTENING REFERENCES WHO Technical Report Series No. 908, 2003. WHO Expert Committee on Specifications for Pharmaceutical preparation. 34th Report. Geneva, World Health Organisation, 1996 (WHO Technical Report Series. No.863). The International Pharmacopocia, 3rd Ed. Vol. 1, General Methods or Analysis; Vol: Quality Specifications Vol. 3: Quality Specifications: Vol. 4: Tests, Methods and General Requirements. Geneva, World Health Organization, 1979 – 2002. Good Storage Practice: Joint Report of The Committee for Official Laboratories and Medicinal Control Services and The Industrial Pharmacists Section of The International Pharmaceutical Federation (FIP). Pharm. Ind., 1980; 42: 1082 – 1085. Management of drug Purchasing, Storage and Distribution. Manual for Developing Countries. Geneva, World Health Organization, 1992. Survey of drug Storage Practices in Homes, Hospitals and Patent Medicine Stores in Nsukka, Nigeria, Scientific Research and Essay Vol. 4 (11); 1354 -1359. Bajaj S. Singla D, Sakhuja N. Stability Testing of Pharmaceutical Products J. of Applied Pharmaceutical Sciences Vol. 02 (03), 2012, 129 – 138. Next Week (November 4th, 2015): WHITE TEAM Fortnight (November 11th, 2015): LEGAL UNIT …Have a Nice Day