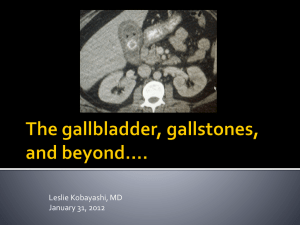
choledocholithiasis
advertisement

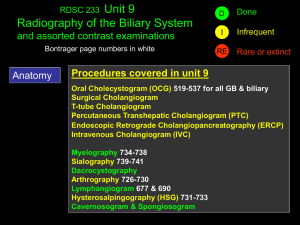
GROUP C Salazar, Riccel Salcedo, Von Saldana, Emmanuel Sales, Maria Stephanie Salonga, Cryscel September 21, 2009 Choledocholithiasis occurs as a result of either the primary formation of stones in the common bile duct (CBD) or the passage of gallstones from the gallbladder through the cystic duct into the CBD. http://www.nlm.nih.gov/medlineplus/ency/article/000274.htm Majority of the bile duct stones are cholesterol stones formed in the gallbladder which then migrates into the exrahepatic biliary tree through the cystic duct [secondary ] Obstruction of the CBD by gallstones leads to symptoms and complications that include pain, jaundice, cholangitis, pancreatits and sepsis. Harrison’s Principles of Internal Medicine 17th ed p.1999 1. Hepatobiliary parasitism or chronic, recurrent cholangitis 2. Congenital anomalies of the bile ducts 3. Dilated or sclerosed or strictured ducts 4. MD3 gene defect leading to impaired biliary phospholipids secretion Harrison’s Principles of Internal Medicine 17th ed p.1999 1. Cholesterol stones 2. Black pigment stones 3. Brown pigment stones Secondary stones are those who were formed in the gallbladder and later on migrate into the CBD Age • 25% of elderly patients may have calculi in the CBD Previous History of Gallstones • Undetected duct stones are left behind in ~1-5% of cholecystectomy patients Infection with parasites • Ascaris Lumbricoides • Clonorchis sinensis http://www.nlm.nih.gov/medlineplus/ency/article/000274.htm Can be completely asymptomatic Symptoms usually do not occur unless the stone blocks the common bile duct Symptoms and signs usually present as RUQ abdominal pain Jaundice Fever Tea colored urine Acholic stools Nausea and or Vomiting Presentation • Pain in RUQ or MUQ • Sharp, cramping or dull • Pain radiating to the back or below the scapula • Pain worsening after eating fatty/greasy food Patient • In our Patient: • - Denies of having abdominal pain • [But choledocholelithiasis can present as a painless jaundice] Presentation • Painless jaundice may occur in patients with cholelithiasis • -caused by increased bilirubin in the blood • - post hepatic/obstructive jaundice • Initially presents as Icteric sclera Patient • Positive for jaundice Presentation Patient • signifies post hepatic cause of jaundice [Obstructive Jaundice] • Positive for Tea/Dark Colored urine • Patient denies acholic stools May be acute or chronic Symptoms result from inflammation Caused by partial obstruction to the flow of bile Presence of bacteria in the bile culture in 75% of patients with acute cholangitis early in the symptomatic course CHARCOT’S TRIAD Characteristic presentation of acute cholangitis Biliary pain, jaundice and spiking fever with chills Blood cultures are frequently positive, and leukocytosis is typical Nonsuppurative acute cholangitis Most common and may respond relatively rapidly to supportive measures and to treatment with antibiotics Suppurative acute cholangitis Presence of pus under pressure in a completely obstructed ductal system leads to symptoms of toxicity ▪ REYNOLDS PENTAD ▪ Mental confusion and septic shock ▪ Biliary pain, jaundice and spiking fever with chills Response to antibiotics is poor Multiple hepatic abscesses are present Mortality rate approaches 100% ▪ Endoscopic or surgical relief of the obstruction and drainage of the infected bile Endoscopic management Effective as surgical intervention ERCP with endoscopic sphincterotomy Preferred initial procedure for both establishing a definitive diagnosis and providing effective therapy Safe Gradual obstruction of the CBD jaundice or pruritus without associated symptoms of biliary colic or cholangitis Painless jaundice Associated chronic calculous cholecystitis is very common Absence of a palpable gallbladder Biliary obstruction causes progressive dilatation of the intrahepatic bile ducts Hepatic bile flow is suppressed Reabsorption and regurgitation of conjugated bilirubin into the bloodstream Jaundice, dark urine (bilirubinuria), light-colored (acholic) stools CBD stones should be suspected in any patient with cholecystitis whose serum bilirubin level is >85.5 mol/L (5 mg/dL) Maximum bilirubin level is seldom >256.5 mol/L (15.0 mg/dL) in patients with choledocholithiasis Serum alkaline phosphatase level is almost always elevated May be a two- to tenfold elevation of serum aminotransferases, especially in association with acute obstruction Most common associated entity discovered in patients with nonalcoholic acute pancreatitis is biliary tract disease Complicates: acute cholecystitis: 15% Choledocholithiasis: >30% Common factor appears to be the passage of gallstones through the common duct Coexisting pancreatitis should be suspected in patients with symptoms of cholecystitis who develop: back pain or pain to the left of the abdominal midline prolonged vomiting with paralytic ileus a pleural effusion, especially on the left side Surgical treatment of gallstone disease is usually associated with resolution of the pancreatitis May complicate prolonged or intermittent duct obstruction with or without recurrent cholangitis May be progressive even after correction of the obstructing process Increasingly severe hepatic cirrhosis may lead to portal hypertension or to hepatic failure and death May also be associated with clinically relevant deficiencies of the fat-soluble vitamins A, D, E, and K Laboratory studies Imaging studies Ultrasonography MRC Endoscopic cholangiography Not specific for the diagnosis of choledocholithiasis Increase in serum bilirubin, alkaline phosphatase, gamma-glutamyl transpeptidase Moderate elevations on aminotranferases Ultrasonography •Commonly the first test •Useful for documenting stones in the gallbladder and determining the size of the common bile duct (90% accuracy). Shows a dilated common bile duct (>8 mm in diameter) in a patient with gallstones, jaundice, and biliary pain highly suggestive of common bile duct stones. •Detection of CBD stones is impeded by the presence of gas in the duodenum, possible reflection and refraction of the sound beam by curvature of the duct, and the location of the duct beyond the optimal focal point of the transducer MAGNETIC RESONANCE CHOLANGIOGRAPHY Very accurate in the detection of biliary tree obstruction and ductal dilatation, both intrahepatic and extrahepatic. Has a sensitivity of 75-90% in the detection of CBD stones, which makes it an essential tool in the evaluation of patients with jaundice. Capable of defining the level of the obstruction and provides information about the surrounding structures, especially the pancreas. Provides excellent anatomic detail and has a sensitivity and specificity of 95 and 89%, respectively, at detecting choledocholithiasis Cost, inconvenience, and limitations (eg, obesity, presence of metal objects, eg, pacemakers) are some of its disadvantages. Gold standard for diagnosing common bile duct stones Has a distinct advantage of providing a therapeutic option at the time of diagnosis The CBD is cannulated through the ampulla, contrast material is injected, and films are obtained. The experience of the endoscopist is the best predictor of success, which is 90-95% in expert hands. Endoscopic Cholangiography ERC from the same patient shows multiple stones in the common bile duct. Only the top one showed on ultrasound, as the other stones lie in the distal common bile duct behind the duodenum. Medical ERCP Percutaneous extraction Extracorporeal shock wave lithotripsy Surgical Open choledochotomy Transcystic exploration Drainage procedures ▪ Transduodenal sphincteroplasty ▪ Choledochoduodenostomy ▪ Choledochojejunostomy Cholecystectomy Patients with symptomatic gallstones and suspected common bile duct stones, either preoperative endoscopic cholangiography or an intraoperative cholangiogram will document the bile duct stones. If an endoscopic cholangiogram reveals stones, sphincterotomy and ductal clearance of the stones is appropriate, followed by a laparoscopic cholecystectomy. An intraoperative cholangiogram at the time of cholecystectomy will also document the presence or absence of bile duct stones Laparoscopic common bile duct exploration via the cystic duct or with formal choledochotomy allows the stones to be retrieved in the same setting. An open common bile duct exploration is an option if the endoscopic method has already been tried or is for some reason not feasible. If a choledochotomy is performed, a T tube is left in place. Stones impacted in the ampulla may be difficult for both endoscopic ductal clearance as well as common bile duct exploration (open or laparoscopic). In these cases the common bile duct is usually quite dilated (about 2 cm in diameter). Choledochoduodenostomy Roux-en-Y choledochojejunostomy Harrison’s Principles of Internal Medicine, 17th ed. http://www.nlm.nih.gov/medlineplus/ency/ar ticle/000274.htm