Jaundice
advertisement

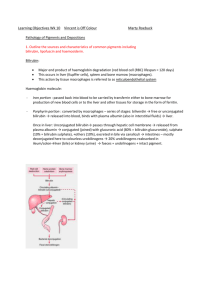
Thamer A. Bin Traiki Introduction Jaundice (icterus) is yellowish discoloration of the skin & sclera as a result of raised level of serum bilirubin . A careful clinical examination cannot detect jaundice until the serum bilirubin is more than 2 mg/dL (34 µmol/liter), twice the normal upper limit. The yellow discoloration is best seen in the periphery of the ocular conjunctivae and in the oral mucous membranes (under the tongue, hard palate). Cont… The normal serum bilirubin concentration in children and adults is less than 1 mg/dL (17 µmol/liter). Less than 5 percent of which is present in conjugated form. The measurement is usually made using diazo reagents and spectrophotometry. Cont… Conjugated bilirubin reacts rapidly ("directly") with the reagents. The measurement of unconjugated bilirubin requires the addition of an accelerator compound. Elevated serum bilirubin concentrations can be due to three causes which can sometimes coexist: Overproduction of bilirubin Impaired uptake, conjugation, or excretion of bilirubin Backward leakage from damaged hepatocytes or bile ducts FORMATION OF BILIRUBIN Bilirubin is formed by breakdown of heme present in hemoglobin, myoglobin, cytochromes, catalase, peroxidase and tryptophan pyrrolase. 80% of the daily bilirubin production (250 to 400 mg in adults) is derived from hemoglobin . The remaining 20 % being contributed by other hemoproteins and a rapidly turning-over small pool of free heme. Enhanced bilirubin formation is found in all conditions associated with increased red cell turnover such as intramedullary or intravascular hemolysis. Cont… Heme consists of a ring of four pyrroles joined by carbon bridges and a central iron atom (ferroprotoporphyrin IX). Bilirubin is generated by sequential catalytic degradation of heme mediated by two groups of enzymes: Heme oxygenase Biliverdin reductase Cont… Heme oxygenase Initiates the opening of the porphyrin ring of heme by catalyzing the oxidation of the alpha-carbon bridge . This leads to formation of the green pigment, biliverdin Biliverdin reductase Reduce the biliverdin to the orange-yellow pigment bilirubin . Iron is released in this process. The oxidized alpha-bridge carbon is eliminated as carbon monoxide (CO). Bilirubin is very poorly soluble in water at physiologic pH because of internal hydrogen bonding . Conversion of bilirubin to a water-soluble form, by disruption of the hydrogen bonds, is essential for the elimination by the liver and kidney. This is achieved by glucuronic acid conjugation of the propionic acid side chains of bilirubin. Albumin Binding of Bilirubin in Plasma Binding to albumin and, to a much lesser degree, high density lipoprotein, keeps bilirubin in solution in plasma. Only a small fraction of bilirubin circulates in the unbound state. Binding to high density lipoprotein may become significant in states of severe hypoalbuminemia. Cont… Albumin binding keeps bilirubin in the vascular space, thereby preventing its deposition into extrahepatic tissues, including sensitive tissues such as the brain, and minimizing glomerular filtration. It also transports bilirubin to the sinusoidal surface of the hepatocyte, where the pigment dissociates from albumin and enters the hepatocyte . Cont… Albumin binding of bilirubin is usually reversible. The usual tight but reversible binding to albumin precludes glomerular filtration of unconjugated bilirubin. In contrast, conjugated bilirubin is less strongly bound to albumin and can be excreted in the urine. Thus, the finding of bilirubin in the urine, in the absence of albuminuria, indicates the presence of an increased amount of conjugated bilirubin in the plasma. Cont… However, irreversible binding can occur in the presence of prolonged conjugated hyperbilirubinemia, eg, during biliary obstruction. The bilirubin fraction irreversibly bound to albumin (delta- bilirubin) is not cleared by the liver or the kidney . Uptake and Storage of Bilirubin by Hepatocytes In the liver sinusoids, the albumin-bilirubin complex dissociates, and the bilirubin is taken up efficiently by the hepatocyte while the albumin remains in the circulation. Bilirubin is taken up by hepatocytes by a process of facilitated diffusion, which is not energy-consuming; as a result, transport cannot occur against a concentration gradient, and is bidirectional. Cont… Sinusoidal bilirubin uptake requires inorganic anions, such as chloride, and is thought to be mediated by carrier proteins . Within the hepatocyte, bilirubin and other organic anions bind to glutathione S-transferases (GSTs). GST-binding reduces the efflux of the internalized bilirubin, thereby increasing net uptake . Conjugation of Bilirubin Glucuronidation of bilirubin by the enzyme glucuronyl transferase in the hepatocyte particularly in the endoplasmic reticulum . Bilirubin diglucuronide is the predominant pigment in normal adult human bile, representing over 80%of the pigment. Bilirubin glucuronides are water-soluble and are readily excreted in bile. Unconjugated bilirubin accounts for only 1 to 4 % of pigments in normal bile. Execretion of Conjugated Bilirubin Conjugated bilirubin is secreted across the bile canalicular membrane of the hepatocyte against a concentration gradient with active transport . Enhanced bile flow (eg, infusion of bile salts) or phenobarbital treatment increases the excretory capacity. Degradation of Bilirubin in the Digestive Tract Bile pigment appearing in bile is mostly (more than 98 percent) conjugated. Conjugated bilirubin is water soluble and is not absorbed across the lipid membrane of the small intestinal epithelium . The unconjugated bilirubin fraction is partially reabsorbed and undergoes enterohepatic circulation . Cont… Bilirubin is reduced by bacterial enzymes in the colon to a series of molecules termed urobilinogens . The two major urobilinoids found in stool, urobilinogen and stercobilinogen, are colorless and turn orange-yellow only after oxidation to urobilins. Urobilinogens and their derivatives are partly absorbed from the bowel, undergo enterohepatic recycling, and are eventually excreted in urine and feces . Cont… In conditions associated with elevated conjugated plasma bilirubin concentrations (eg, intrahepatic or extrahepatic cholestasis), the kidney is responsible for 50 to 90 % of conjugated bilirubin excretion. Ann Surg 1966; 163:330 N Engl J Med 1966; 274:231 However, bile remains the main excretion route for unconjugated hyperbilirubinemia. Cont… In complete biliary obstruction or severe intrahepatic cholestasis (eg, in the early phase of acute viral hepatitis), feces may take the appearance of china clay. Thus, the absence of urobilinogen in stool and urine in a jaundiced patient indicates complete biliary obstruction. The intestinal microflora influence serum levels of bilirubin. In a study in Gunn rats (which have a congenital deficiency of bilirubin UDB-glucuronsyltransferase), treatment with oral clindamycin and neomycin resulted in the disappearance of fecal urobilinoids while serum bilirubin increased dramatically. Intestinal colonization with C. perfringens led to reappearance of fecal urobilinoid production accompanied by a partial decrease in serum bilirubin levels. The authors speculated that prolonged use of certain antibiotics may lead to an increase in serum bilirubin levels in humans & patients with abnormal bilirubin conjugation may be at particular risk. J Hepatol 2005; 42:238. Delta Bilirubin Albumin-linked bilirubin fraction . Formed in the serum when hepatic excretion of bilirubin glucuronides is impaired. Delta bilirubin constituted 8 to 90% of total bilirubin in patients with hepatocellular and cholestatic jaundice. Because of its covalent binding to albumin, the clearance of delta bilirubin is approximately the same as albumin rather than the short half-life of conjugated bilirubin that is not albumin bound (12 to 24 days versus 4 hours). JAMA 1971; 218:216 Because conjugated bilirubin is excreted in the urine, patients with conjugated hyperbilirubinemia develop bilirubinuria. Some patients with conjugated hyperbilirubinemia do not exhibit bilirubinuria during the recovery phase of their disease because delta bilirubin. Late in the recovery phase of hepatobiliary disorders, virtually all the conjugated bilirubin may be in the albumin-linked form. As a result, elevated serum bilirubin levels decline more slowly than expected in some patients who otherwise appear to be recovering satisfactorily. Cont… Because delta-bilirubin gives a "direct" diazo(reagents causes breakdown of the tetrapyrrole to two azodipyrroles which can be readily measured spectrophotometrically) reaction, this may give a false impression of a persistent blockage of the bile ducts . The presence of delta-bilirubin can be inferred by the absence of bilirubin excretion in the urine despite the apparent presence of direct hyperbilirubinemia and can be identified by high performance liquid chromatography of serum . Urine Bilirubin The presence of bilirubin in the urine reflects direct hyperbilirubinemia and therefore underlying hepatobiliary disease. In contrast to conjugated bilirubin, unconjugated bilirubin is tightly bound to albumin & it is not filtered by the glomerulus. Conjugated bilirubin may be found in the urine when the total serum bilirubin concentration is normal because the renal reabsorptive capacity for conjugated bilirubin is low and the methods used can detect urinary bilirubin concentrations as low as 0.05 mg/dL (0.9 micromol/L). Cont… Thus, bilirubinuria may be an early sign of liver or biliary disease, while the clearance of bilirubin from the urine may be an early sign of recovery since, as delta bilirubin is protein-bound. For clinical purposes, the predominant type of bile pigments in the plasma can be used to classify hyperbilirubinemia into two major categories . Plasma elevation of predominantly unconjugated bilirubin due to The overproduction of bilirubin, impaired bilirubin uptake by the liver, or abnormalities of bilirubin conjugation Plasma elevation of both unconjugated and conjugated bilirubin due to hepatocellular diseases, impaired canalicular excretion, and biliary obstruction Unconjugated Hyperbilirubinemia Hx Age? Duration of the complaint? Fever or rigors? Recent outbreak of jaundice? Recent consumption of shellfish? IVDA? Sexual contact? Blood transfusion? Alcohol consumption? Drugs recently? Recent travel? Anesthesia? Family hx (is it gilberts) Recent biliary surgery? Hx of hemolytic diseases? Specific Symptoms Articaria Pruritis Dark urine Pale stool Abdominal pain charcot’s triad?? Signs Is it really jaundice or psudo? 1.carotenemia:(palms , soles & NL folds) 2.Uremic Pigmentation Chronic uremics retain the yellow urochrome pigments which normally color urine amber. 3. Industrial Staining of Skin - In a number of industries yellow pigments used may stain the exposed portions of the skin of the workers Cont… ascites, splenomegaly (tipped), spider angiomata, and gynecomastia Hepatomegaly Palplable GB Courvoisier sign : palpable GB+ jaundice=CA (not GS) Murphey’s sign hyperpigmentation in hemochromatosis. a Kayser-Fleischer ring in Wilson's disease. xanthomas in primary biliary cirrhosis. Cold sores (HSV-hepatitis) Ultrasonography The sensitivity of US for the detection of dilated bile ducts and biliary obstruction ranges in various studies from 55 to 91 % . The sensitivity increases with the serum bilirubin concentration and the duration of jaundice. Radiology 1979; 133:39 US can also demonstrate cholelithiasis and gallbladder stones; however, common duct stones may not be well seen since gas in the duodenum can obscure visualization of the distal common duct. The advantages of US are that it is noninvasive, portable, and relatively inexpensive. Endoscopic ultrasound (EUS) By placing an ultrasound transducer directly in the duodenum, EUS allows complete visualization of the common bile duct without the hindrance of overlying bowel gas, which limits traditional ultrasound. EUS has a similar accuracy to ERCP for detection of small common bile duct stones but does not carry the risk of inducing pancreatitis. EUS is also highly accurate for detecting pancreatic tumors, especially small (<3cm) tumors which are difficult to see with helical CT. The main disadvantages of EUS the semi-invasive nature of the test The inability to directly remove stones found in the bile duct. CT scan Conventional CT and US are equally effective for the recognition of obstruction and identification of the level of obstruction. Helical (spiral) CT has improved the accuracy of CT and may emerge as the preferred technique for hepatobiliary imaging . Helical CT offers a more comprehensive analysis of the liver and extrahepatic abdomen and pelvis. CT in comparison to US Not as sensitive in detecting cholelithiasis because only calcified stones are visualized. It is more expensive . ERCP ERCP permits direct visualization of the biliary tree and pancreatic ducts. It is clearly superior to US and CT for the detection of extrahepatic obstruction . It is the procedure of choice when there is suspicion of choledocholithiasis. Another advantage of ERCP is that a therapeutic intervention, such as stone extraction or papillotomy, can be performed during the procedure Cont… ERCP is more expensive than US and CT . Invasive Associated with a finite rate of mortality (0.2 %) Complications such as bleeding, cholangitis, and pancreatitis (3 %) MRCP MRCP is a potential alternative to ERCP. Although contrast material is administered, cholangiographic images can be obtained similar to those obtained with ERCP. In patients with dilated ducts, a MRCP cholangiogram is diagnostic in 90 to 100 percent of patients. It reveals the level of obstruction in 80 to 100% Has a sensitivity and specificity of 90 to 100 % for the detection of choledocholithiasis and bile duct stenosis. MRCP is as accurate as ERCP for detecting choledocholithiasis . Cont… MRCP is expensive and may eventually replace diagnostic ERCP. However, it is unlikely to replace US or helical CT as the initial imaging test in the diagnostic evaluation of jaundice . ERCP is preferred in the patient with cholangitis because it permits therapeutic drainage of the obstruction. Percutaneous transhepatic cholangiography Requires passage of a needle through the skin into the hepatic parenchyma and advancement into a peripheral bile duct. Injection of contrast media provides close to 100 % sensitivity and specificity for the diagnosis of biliary tract obstruction . Cont… It is similar to ERCP in cost and morbidity . Particularly useful when the level of obstruction is proximal to the common hepatic duct or ERCP is precluded for anatomic reasons. However, it may be technically limited in the absence of dilatation of the intrahepatic ducts .