October 15, 2012 Dr. Megan Gonzales ND, EAMP SIOM Western
advertisement

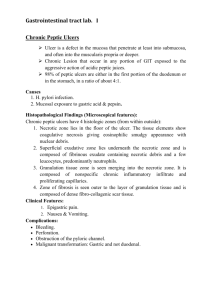
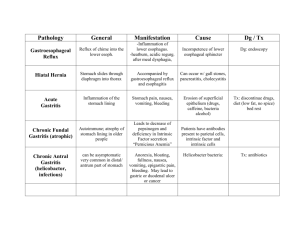
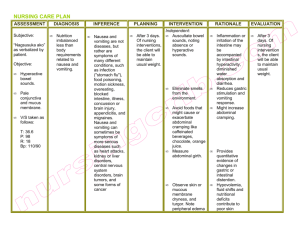
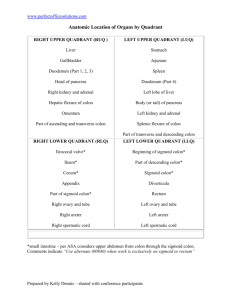
MORE GASTROINTESTINAL I just thought we needed a better symptom picture October 15, 2012 Dr. Megan Gonzales ND, EAMP SIOM Western Clinical Sciences Fall 2012 ✤ intrinsic factor is an important glycoprotein released by the gastric parietal cells that is required for B12 absorption later in the small intestine GERD ✤ Gastroesophageal Reflux Disease: ✤ backflow of gastric or duodenal contents into the esophagus past the lower esophageal sphincter ✤ there are not always symptoms - commonly heartburn relieved by antacids ✤ symptoms may be worsened by vigorous exercise, bending over and lying down ✤ the pain can mimic angina pectoris ✤ there may be pain or difficulty swallowing after long term reflux. Esophageal stricture, spasm or even esophageal bleeding. ✤ Sometimes it can waken the patient at night with coughing and choking. ✤ There may be an associated hiatal hernia ✤ Pulmonary symptoms are associated with aspiration of gastric contents. Chronic bronchitis, asthma, morning hoarseness and nocturnal wheeze. ✤ The Lower Esophageal Sphincter functions in two ways - opening by relaxation and opening based on differences in pressure gradients between the lower esophagus and stomach. The esophageal muscles can be weakened by mechanical disturbance or through sliding through the diaphragmatic hiatus (a hiatal hernia). Tight clothing or other causes of increased pressure below the diaphragm can lead to GERD (pregnancy, overweight). ✤ Factors that can increase pressure on the lower esophageal sphincter: carbohydrates, low-dose ethanol, nonfat milk, protein. ✤ Factors that lead to a lower pressure and can increase incidence of GERD: antiflatulents, chocolate, cigarette smoking, fat, high dose ethanol, lying on either side of your body, orange juice, peppermint, sitting, tomatoes, whole milk. ✤ REALLY. ✤ it’s important to avoid acid producing foods: wine, tomato, chocolate, orange juice, liquor, carbonated beverages, spicy food. ✤ Remember large meals cause increased pressure below the esophageal sphincter ✤ a person who suffers from GERD should not lie down for 2 hours post-meal ✤ Nicotine relaxes the lower esophageal sphincter and stimulates stomach acid production. Smoking decreases gastric motility and can injure the esophagus. ✤ The book states that stress is not a direct factor but I think if we were to delve more specifically into psychoneuroimmunology there would be quite a direct link to many diseases and stress. Mallory-Weiss Syndrome ✤ as we talked about earlier: esophageal tearing related to forceful and prolonged vomitting. ✤ the upper esophageal sphincter fails to relax during vomiting often related to excessive alcohol intake. More common in men than women. ✤ complications - hypovolemia and fatal shock Hiatal Hernia ✤ a defect where the diaphragm allows the stomach to slip up into the chest ✤ two types: a sliding hiatal hernia and paraesophageal hernia. SLIDING - the stomach and gastroesophageal junction slip up into the chest so the gastroesophageal junction is superior to the diaphragm. PARAESOPHAGEAL - a part of the greater curvature of the stomach rolls through the diaphragm ✤ often related to muscle weakening common with aging, diaphragmatic malformations, obesity and smoking are common risk factors. Incidence increases with age and sliding is more common than paraesophageal malfunction. ✤ can lead to dysphagia, gastroesophageal reflux, Barrett’s esophagus, esophageal adenocarcinoma ✤ often there are no symptoms, there may be a symptom of fullness in the chest and pain resembling angina pectoris (temporary pain, pressure, fullness, or squeezing in the center of the chest or in the neck, shoulder, jaw, upper arm, or upper back), if the sphincter is incompetent then symptoms are those of GERD ✤ Diagnosis: based on endoscopy, barium study, pH studies, esophageal motility studies ✤ treatment is focused on relieving symptoms Gastritis ACUTE: mucosal reddening, edema, hemorrhage, erosion CHRONIC: common in elderly people and people with pernicious anemia. ✤ ACUTE: causes - chronic indigestion, drugs like aspirin, ingestion of poison, endotoxins from infection bacteria. Can lead to stress ulcers, there is a rapid onset of symptoms of epigastric discomfort and anorexia, nausea and vomiting and hematemesis. ✤ CHRONIC: seen with peptic ulcers and gastrostomy where there is chronic reflux of pancreatic enzymes, bile and bile acids into the stomach. Environmental exposures can contribute to developing the disease - smoking, pernicious anemia, alcohol, renal disease, diabetes mellitus ✤ either can lead to hemorrhage, shock, obstruction, perforation, peritonitis and gastric ulcer ✤ Diagnosis is based on occult blood studies ✤ Treatment: focused on eliminating the cause of the disease H2 blockers, antacids, neutralizing agents, replacement of blood with severe bleeding, surgery, bland diet Peptic Ulcer Disease ✤ Factors In Developing Peptic Ulcer Disease: ✤ INCREASED ACID PRODUCTION: increased parietal and chief cells, increased sensitivity to food and other stimuli like caffeine, excess vagal stimulation, decreased inhibition of gastric secretions ✤ IMPAIRED MUCOSAL BARRIER PROTECTION: inadequate mucosal blood supply, impaired mucus production, bile or pancreatic enzyme reflux from the duodenum, aspirin/NSAID or alcohol consumption, colonization by H. pylori ✤ symptoms include - heartburn, indigestion, duodenal ulcers - well localized midepigastric pain relieved by food. Pain usually returns about 2 hours after ingestion of a meal or with eating oranges, coffee, aspirin, or alcohol. ✤ Diagnosis is based on symptoms, upper endoscopy, barium Proton Pump Inhibitors ✤ inhibits gastric parietal cell hydrogen-potassium ATPase ✤ PPIs work by entering a parietal cell, becoming activated in the lower pH environment and then binding to proton pumps inhibiting acid secretion H2 Blockers ✤ histamine 2 blockers are named based on the type of histamine receptor they affect ✤ they work by blocking histamine 2 receptors on parietal cells. These receptors, when stimulated, increase stomach acid secretion. Zollinger-Ellison Syndrome ✤ caused by tumors in the head of the pancreas and/or upper small intestine. Tumors produce gastrin - “gastrinomas” - cause an increase in stomach acid production Irritable Bowel Disease ✤ Ulcerative Colitis ✤ chronic inflammatory condition affecting the mucosa of the colon, begins lower - rectum and sigmoid colon - and moves into the entire colon. Etiology is unknown though it is thought to be related to an abnormal mucosal immune response related to food or bacteria. It occurs in young women primarily. It is one of the diseases known to predominately affect those of Ashkanazi Jewish descent. ✤ it can lead to nutritional deficiencies, perineal sepsis, anal fissures and fistulae, perirectal abscess, toxic megacolon and coagulation deficit ✤ hallmark of the disease are recurrent bloody diarrhea attacks containing pus and mucus. The patient can have upwards of 15 to 20 attacks of liquid bloody stools a day. It can lead to hemorrhage, stricture and colonic perforation. ✤ People suffering from this disorder may also have joint inflammation, ankylosing spondylitis, eye lesions, mouth ulcers, liver disease and pyoderma gangrenosum (necrotic tissue generally in the lower extremities but can be present anywhere) Ulcerative Colitis ✤ diagnosis is made with at least a sigmoidoscopy, if not colonoscopy ✤ showing increased mucosal friability, decreased mucosal detail, pinpoint hemorrhages, thick inflammatory exudate. Bx helps confirm ✤ Treatment is focused on controlling inflammation. Antispasmotics and antidiarrheals can cause extreme dilation of the colon (toxic megacolon) so are contraindicated Crohn’s Disease autoimmune inflammatory disease of the bowel ✤ Crohn’s Disease: ✤ also known as regional enteritis is an inflammation of any part of the GI tract usually the proximal end of the colon but also the terminal illeum. The inflammation extends through the entire intestinal wall. Granulomas are surrounded by normal tissue - multiple lesions are called “skip lesions” ✤ autoimmune and genetic factors play a significant role in disease development. Lacteal blockage in the intestinal wall leads to edema and inflammation, ulceration and stenosis. ✤ most prevalent in adults 20-40 again predominantly in Ashkanazi Jewish populations. ✤ Can lead to: anal fistula, perineal abscess, intestinal obstruction, nutritional deficiency and peritonitis ✤ signs can be mild and nonspecific depending on lesion location. The acute symptoms mimic appendicitis. Colicky right lower quadrant pain, cramping, tenderness, flatulence, nausea, fever and diarrhea. Marked by weakness, fatigue, clubbing of the fingers, weight loss and up to 4 episodes of diarrhea a day. ✤ Diagnosis ✤ ✤ barium enema showing segments of stricture and normal bowel. Sigmoidoscopy or colonoscopy shows patchy inflammation. Bx provides the definitive diagnosis Treatment ✤ is focused on controlling the inflammatory process. Steroids and immunomodulators are prescribed. Lifestyle changes are necessary including adequate physical rest, restricted diet, B12, elimination of dairy products. Surgery can be used to correct perforation, fistulas and obstruction. Irritable Bowel Syndrome IBS ✤ is also called spastic colon or spastic colitis. Marked by chronic or periodic diarrhea alternating with episodes of constipation and abdominal cramps. ✤ associated wit hpsychological stress but can result from physical factors like hormonal changes and diverticular disease, lactose intolerance, laxative abuse and foods like coffee and raw fruits and veggies. ✤ there is a higher incidence of people with IBS being diagnosed with colon cancer ✤ there is usually lower abdominal pain relieved by passing stool or gas, diarrhea that occurs during the day alternating with constipation, dyspepsia and abdominal distention may be present. More common in women than men. ✤ Diagnosis is made through a thorough history and rule-out of other disorders like amebiasis, diverticulitis, colon cancer and lactose intolerance. ✤ Treatment focuses on relieving symptoms and counseling to help the patient understand the relationship between stress and illness. Avoidance of food irritants can be helpful but dietary restrictions otherwise do not seem to be beneficial. Celiac Disease ✤ poor absorption and intolerance of the gluten protein present in wheat and wheat products. The intestinal wall villi which are necessary for optimal absorption of nutrients atrophy and there is a decreased amount and activity of enzymes present on the epithelium. ✤ affects 1 out of every 133 people in the United States. Due to intramucosal enzyme defect that causes an inability to digest gluten. The toxicity causes increased cell turnover, increased epithelial lymphocytes and damage to surface epithelium of the small intestine. ✤ Associated with DR3 and DQw2 two human leukocyte antigen halotypes, often considered autoimmune in nature. ✤ associated with anemia, lactose intolerance, skin disorders like dermatitis herpetaformis, type 1 diabetes, thyroid disease, down syndrome, infertility and miscarriage, osteoporosis/osteopenia, autoimmune disorders ✤ can cause anemia due to malabsorption, syncope, heart failure and angina secondary to anemia, bleeding disorders related to vitamin K deficiency, a higher incidence of intestinal lymphoma ✤ GI: steatorrhea, diarrhea, abdominal distention, stomach cramps, weakness, anorexia, malabsorption of all macronutrients - protein, fat, carbohydrates, loss of fat soluble vitamins, calcium, minerals and electrolytes ✤ Hematologic: normochromic, hypochromic, macrocytic anemia due to poor absorption of folate, B12, iron. Also, hypoprothrombinemia due to vitamin K malabsorption ✤ calcium and vitamin D malabsorption lead to osteomalacia, osteoporosis, tetany and bone pain ✤ peripheral neuropathy, seizures and paresthesias can result ✤ skin diseases like dry skin, eczema, psoriasis, acne rosacea can occur ✤ amenorrhea, hypometabolism, adrenocortical insufficiency in severe disease presentations ✤ mood changes and irritability ✤ Diagnosis: ✤ histologic changes present in small bowel on Bx ✤ Treatment: ✤ elimination of gluten for life, intestinal lining can return to normal after several months but may not Meckel’s Diverticulum ✤ a congenital anomaly where a blind tube (like the appendix) opens near the ileocecal valve. Occurs mostly in males. ✤ Can be asymptomatic ✤ complicated forms cause abdominal pain especially around the umbilicus, dark red melena or hematochezia, the lining is actually gastric mucosa ✤ it can cause peptic ulcers, perforation, peritonitis and even bowel obstruction Inguinal Hernia ✤ when part of an intestine protrudes through an opening in the abdominal wall - here along the anatomical inguinal canal. ✤ Either direct or indirect. A direct inguinal hernia develops from a weakness in the fascial floor of the inguinal canal. An indirect hernia the intestine leaves the abdominal cavity and descends through the inguinal ring following the spermatic cord or round ligament ✤ it can lead to incarceration or strangulation of the bowel, intestinal obstruction and intestinal necrosis ✤ there is usually a lump over the area of herniation, the lump normally disappears when the patient lies supine ✤ strangulation produces severe pain and can lead to obstruction and necrosis ✤ physical exam reveals the swelling, palpation while Valsalva is performed confirms ✤ Treatment: pushing by reducing, herniography Intussusception Volvulus Inactive Colon ✤ lazy colon or colonic stasis, atonic constipation ✤ usually due to lack of one of three things - dietary bulk, fluid intake, exercise. Common in bedridden people because of inactivity and relieved by fiber and exercise. Can also be due to habitual disregard of need to defecate, emotional conflict, chronic laxative use, dependence on enemas ✤ the primary symptom is chronic constipation ✤ history of dry, hard, infrequent stools. DRE reveals stool in the rectum and a palpable colon. Barium enema, fecal occult blood ✤ treatment varies depending on presenting symptoms and underlying cause. Increase fluids, add fiber. avoid fats, exercise, avoid over-use of laxatives Pancreatitis ✤ acute and chronic forms can be due to edema, necrosis, hemorrhage ✤ in men it is associated frequently with alcoholism, trauma, peptic ulcers ✤ in women it is linked to biliary tract disease ✤ prognosis is good if related to biliary tract disease but poor when related to alcoholism ✤ Acute pancreatitis increases in frequency as patient age increases. It is most commonly associated with alcoholism and biliary tract disease. It can be linked to as diverse causes as use of glucocorticoids and viral infections or pregnancy. ✤ Complications include: DM (when islets of langerhans are involved), massive hemorrhage, destruction of pancreas, shock, coma, adult respiratory distress syndrome, atelectasis, pulmonary effusion, pneumonia, GI bleeding, pancreatic abscess ✤ the first and only symptom of mild pancreatitis is steady pain centered near the umbilicus radiating to the back - between the 10th thoracic and lower lumbar vertebra, NOT alleviated by vomiting. ✤ Severe attack - extreme pain, vomiting, abdominal rigidity, diminished bowel activity, crackles in lung bases and left pleural effusion ✤ as it progresses - extreme malaise, restlessness, mottled skin, tachycardia, low grade fever, diaphoresis ✤ diagnosis: PE, thorough patient history, assessment is difficult due to location of pancreas. LABS - serum lipase elevated, fat necrosis causes decreased calcium, WBCs elevated, high glucose levels ✤ treatment - maintain circulation and fluid levels, emergency treatment, analgesics, antibiotics Pilonidal Disease ✤ a cyst forms in the intergluteal cleft. It usually contains hair and can become infected. Highest incidence in men aged 18-30. ✤ congenitally acquired or due to stretching of irritation of the sacrococcygeal region (heavy exercise, heat, perspiration and constrictive clothing) ✤ asymptomatic until infected ✤ treatment: I and D, extraction of protruding hairs, sitz baths, Proctitis ✤ acute or chronic inflammation of the rectal mucosa. Can result in discomfort, bleeding and possibly discharge and mucus or pus ✤ caused by STI, amebiasis, in children b-hemolytic strep can cause it, autoimmune proctitis is associated with UC and Crohn’s, medications, chemical agents ✤ Contributing factors: chronic constipation, habitual laxative use, emotional upset, radiation, endocrine dysfunction, rectal injury, rectal medication, bacterial infections, allergies - especially milk, food poisoning ✤ symptoms: tenesmus, constipation, feeling of rectal fullness, abdominal cramps, intense urge to defecate ✤ detailed patient history, sigmoidoscopy ✤ treatment focuses on alleviating the underlying cause of the disorder