Surgical Asepsis and Infection Prevention
advertisement

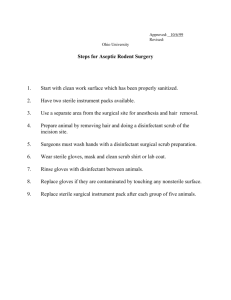
Surgical Asepsis and Infection Prevention Kathleen McMullen, MPH CIC Objectives At the completion of this activity, the learner should be able to: Use the OR observation tool presented as a template Utilize ideas offered to standardize feedback of OR observations Explain the idea of a one-page dashboard and compose a similar document for their administration Items for Discussion OR Observations Methods for completion Guidelines referenced (slides with AORN reference in the footnote) Feedback formats Thoughts on increasing compliance Background Barnes Jewish Hospital 1250 bed tertiary care hospital associated with Washington University School of Medicine St. Louis, Missouri Peri-operative services 5 suites of operating rooms, 1 ambulatory surgery center (66 total operating rooms) 40,000 inpatient and outpatient procedures in 2013 Background Hospital Epidemiology and Infection Prevention 9 Infection Preventionists (7 cover most of the OR) Surgical site infection (SSI) surveillance for 11 operative procedures at the hospital; all procedures at the ASC First Meetings: Building Relationships General tips for building relationships Be prepared Allow them to make decisions Act as a consultant, not the police Pay attention to the details! It takes time Operating Room Observations Includes 2 main sections Surgical attire – based solely on perioperative services’ surgical attire policy (AORN guidance) IP Technique General Site IP Principles Prep Anesthesiology Environment Operating Room Observations Full observations All questions answered Takes around 1-2 hours to complete Done twice a month for each OR suite Partial observations Surgical attire and environment only Takes about 10 minutes to complete Done 4 times a month per suite What should I audit? Many AORN standards Biggest bang: Its likely to have variety Don’t have forcing functions Smaller, non-obvious errors OR Observation Tool Surgical Attire Include all personnel who enter the OR room at any time during the observation Main personnel: nursing, surgeons, anesthesia, anesthesia techs and vendors Give the number compliant over the number observed Observe scrubs, mask, hat, eyewear, jewelry, fingernails/hands and surgical scrub Surgical Attire Human body is a major source of microbial contamination and transmission of microbes Promote worker safety Promote a high level of cleanliness and hygiene within the perioperative environment Not intended to address sterile surgical attire worn at the surgical field or all PPE AORN Perioperative Standards and Recommended Practices, 2014 Edition Surgical Attire – What to wear Helps contain shedding of squamous epithelial cells and bacteria from the skin The material used and weave of the cloth is important to consider to maximize protection against shedding Wearing clean clothes into the OR ensures that additional contaminants aren’t shed in to the environment AORN Perioperative Standards and Recommended Practices, 2014 Edition Surgical Attire – Where to wear it Don if entering Semirestricted or Restricted areas of the surgical setting Remove when leaving the facility Even if traveling between campuses AORN Perioperative Standards and Recommended Practices, 2014 Edition OR observation – Surgical attire Facility approved scrubs not visibly soiled Scrub top should be secured at the waist, tucked in or fit close to the body Attire made of fleece should not be worn Jackets Buttoned or snapped closed, not tied around the waist Disposable jackets shall be worn over reusable jackets Personal clothing is to be contained within the surgical attire Crew neck T-shirts, v-neck T-shirts and tank top type shirts are acceptable T-shirt sleeves and tails are not to extend beyond the surgical attire Surgical Attire – Jewelry Jewelry that cannot be contained or confined within the surgical attire should not be worn Necklaces on the skin may contaminate the front of the sterile gown Wearing finger rings, nose rings, and ear piercings increases bacterial counts on skin surfaces both when the jewelry is in place and after removal. Earrings had bacterial counts more than 21 times higher beneath the earrings than on the surface of the earrings. Bacterial counts were nine times greater on the skin beneath finger and nose rings than on the rings themselves AORN Perioperative Standards and Recommended Practices, 2014 Edition OR observation – Jewelry Non-scrubbed personnel Up to three rings on one finger 1 watch 1 necklace No bracelets Earrings must be confined within surgical headgear Scrubbed personnel: all jewelry removed or confined within attire/headgear Surgical Attire – Head covers All personnel should cover head and facial hair, including sideburns and the nape of the neck, when in the semirestricted and restricted areas Head coverings contain skin squames and hair shed from the scalp AORN Perioperative Standards and Recommended Practices, 2014 Edition OR observation – Head covers Should cover head and facial hair, including sideburns and necklines Disposable bouffant hats should be worn over reusable head gear Skull caps may not be worn if hair touches shirt collar of a collared shirt Surgical Attire – Masks All individuals entering the restricted areas should wear a surgical mask when open sterile supplies and equipment are present A surgical mask is worn to protect the health care provider from contact with infectious material from the patient (e.g., respiratory secretions, sprays of blood or body fluids) and to protect the patient from exposure to infectious agents carried in the provider’s mouth or nose AORN Perioperative Standards and Recommended Practices, 2014 Edition OR observation – Masks Should be worn when open sterile supplies, sterile equipment and scrubbed personal are present Should fully cover mouth and nose and be secured in a manner that prevents venting Surgical Attire – Eye wear Health care personnel must wear eye protection when splashes, spray, spatter, or droplets of blood or other potentially infectious materials can be reasonably anticipated Appropriate eye protection includes goggles, face shields, and full-face respirators Prescription eyeglasses and contact lenses are not considered eye protection AORN Perioperative Standards and Recommended Practices, 2014 Edition OR observation – Eye wear Must be worn when a procedure is in progress Acceptable eyewear includes reusable or disposable goggles, masks with eye shields and personal glasses equipped with side shields Eyewear should be put on before surgical skin prep starts; in scrubbed personnel, it should be put on prior to the scrubbing process Surgical Attire – Fingernails Health care personnel should keep natural fingernails no more than onequarter inch long Long fingernails pose a risk of developing tears in gloves or injuring a patient during positioning and caring for the patient Chipped removed fingernail polish should be May harbor large numbers of pathogens AORN Perioperative Standards and Recommended Practices, 2014 Edition OR observation – Fingernails Must be clean, short (not to extend past fingertip), natural and healthy Nail polish should not be chipped Surgical Hand Scrub Surgical hand scrub should be performed by health care personnel before donning sterile gloves Use of either an antimicrobial surgical scrub agent intended for surgical hand antisepsis or an alcohol-based antiseptic surgical hand rub Three-minute surgical hand scrubs are as effective as five-minute AORN Perioperative Standards and Recommended Practices, 2014 Edition OR observation – Surgical Hand Scrub Masks should be worn Method of scrub Traditional scrub – minimum 3 minutes, maintain cleanliness after scrub, while drying hands Avaguard use – if hands appear socially clean, can be first scrub of the day OR Observation Tool Techniques: groups of yes/no questions (yes is always the “compliant” answer) General Infection Prevention Principles Site Prep Medications/Solutions Anesthesia Environment General Infection Prevention Hand hygiene Glove change between dirty and clean procedures Hand hygiene when gloves are changed or removed Attention to the sterile field Non-scrubbed individuals always attentive to the sterile field Sterile individuals always face the sterile field, remain sterile during X-rays General Infection Prevention OR door remained closed except when used for entry/exit Instrument used: Were instrument tray filters checked prior to placing instruments on the sterile field? (ie – filter is present, filter does not have holes/tears) All items sterilized by traditional methods (no immediate use or flash sterilization) General Infection Prevention Members of the surgical team appear to be healthy (no coughing, sneezing, etc.) Solutions used: Solutions supplied in single-use containers Solutions used are liquid or solid (i.e. - no sprays; exclude rectal cases) Vendors use a pointer to indicate instruments, etc .on the scrub tables Site Prep Operative site cleaned prior to scrub if necessary (visible soil, trauma, etc.) Hair removal done with clippers and contamination minimized Perineal area prepped or covered, if applicable Surgical site prep used, application done correctly, single use prep used, prep allowed to air dry Anesthesia Alcohol foam available for use in their area Central lines Placed with sterile technique Sterile dressing applied after Anesthesia IV therapy Needleless connectors prepped prior to injecting Stopcocks capped between use Hand Hygiene Gloves worn to start IV, intubate and measure urine Gloves removed and hand hygiene performed after these tasks Anesthesia - Components with Caveats/Removed Caveats: Needleless connectors: only need to be prepped with alcohol if a syringe or cap was not in place prior to the injection Removed: Drape between anesthesia and patient above level of anesthesiologist’s nose and mouth Do the anesthesia personnel lean over drape during a procedure Environment Free of visible dust Surfaces cleaned correctly between cases Floor mopped correctly between cases Non-essential items covered if stored in OR Environment – Cleaning details Between Cases: Break down OR table and thoroughly disinfect both sides of mattress, all hard surfaces and base, all to air dry Disinfect all equipment, including surgical lights, light switches, door handles, telephones, mayo stands and tables Single use disposable cleaning cloths used; one for the table, several others for the rest of the room Environment – Cleaning details Floor Mopping: In this order: Floor within operating field (use floor scrubber if heavily soiled), around and under OR table (table should be moved), then outside operating field For heavily soiled areas use disposable mop head Mop away wheel tracks/foot prints as exiting the room Additional Counts Number of personnel in room not directly involved in case Number of times door opened in a 10 min period while sterile packs were open Number of times door opened in a 10 min period while incision was open Still Building the Relationship Allow stakeholders to make decisions Deliver on your promises in a timely fashion Methods of Observing IP wants to build a collegial relationship with the OR staff and not be viewed as “police" Deficiencies found during the observations should be used to educate all members of the suite and not result in any punitive action In response to management feedback, OR observations include a room number and time of observation Methods of Observing Observation tool shared with staff so they are aware of what is being observed; feedback they offer is appreciated IP introduces themselves as they enter the OR Remind staff that these are routine observations Ask staff if they have any additional concerns to share Ensure you remember to follow-up on those concerns! Individual Observation Feedback Completed observation Emailed to: within 2 days of the OR nurse manager and resource nurse Anesthesia educator Anesthesia tech manager Environmental services supervisor OR Observation Dashboard Completed monthly after all observations are finished Emailed to Peri-operative Services Performance Improvement Committee which includes: OR nurse managers OR educators Director of Peri-operative Services Chief of Surgical Services Chief of Anesthesiology Feedback of Observations At the time of observation (anesthesiology only) Verbal can be problematic: Patients may be awake Providers may not take criticism well Slips of paper with results seem to work better Example – Anes Feedback Maintaining the Relationship Stay in touch by celebrating achievements The more conversations, the closer the connection Priorities and areas of interest ebb and flow Make it a standing meeting Continue to stress that you are here to consult, help Deliver on your promises in a timely fashion How to deal with setbacks Leadership change (sometimes you have to start all over!) Bad data Communication breakdowns Poor compliance Educational Efforts Annual clinical skills days Completed several times a year to catch all staff In person, hands on, small class size to facilitate discussions Newsletter articles More frequent quick blurbs with scientific or regulatory reasons for IP requirements SURGICAL MASKS INCORRECT CORRECT Masks should be worn whenever sterile supplies and equipment are open Mask straps should be tied around the top of the head and at the neck Masks should fully cover the nose and mouth and be secured in a manner that prevents venting SURGICAL EYEWEAR INCORRECT CORRECT Eyewear should be donned before an incision is made, and worn throughout the entirety of the operative procedure Acceptable eyewear includes reusable or disposable goggles, and masks with eye shields Eyewear protects healthcare workers from splashes and sprays of infectious or harmful material to the eyes Personal glasses alone (without side pieces) are NOT acceptable eyewear SURGICAL HEAD COVERING INCORRECT CORRECT Disposable bouffant and hood style covers are preferred Disposable hats should be worn over reusable cloth headgear when entering restricted and semi-restricted areas Personnel should cover head and facial hair, including sideburns and necklines Single use headgear should be removed and discarded in a designated receptacle as soon as possible after daily use HAND HYGIENE INCORRECT CORRECT Perform hand hygiene after glove removal Gloves should always be worn when: Emptying urine containers, intubating, starting IVs, drawing blood from any line, and suctioning Glove change and hand hygiene should be performed between dirty and clean tasks Hand hygiene should be performed before donning sterile gloves and after any glove removal Newsletter Articles Common errors CAUTI and CLABSI best practices Nail hygiene Process changes with OR observations and feedback New cleaner used in ORs And the journey continues… Building the business case for eyewear Need for contact isolation in the OR Use of personal bookbags Eyewear Compliance continues to be a problem Need to sell the need for eyewear as protection for the wearer Developing education with real-life examples of close-call splashes and bloodborne pathogen exposure data Contact Isolation in the OR All non-scrubbed personnel should wear gowns and gloves for contact with the patient or the patient’s stretcher IV pumps, stethoscopes and anesthesia machines should be considered potentially contaminated and gloves should be worn when in contact with them At the end of the case or when the equipment is no longer needed, it should be cleaned and disinfected Contact Isolation and Transport Gloves and gowns do not need to be worn during transport unless activities are in progress that result in contact with the patient or bed If so, a “clean” healthcare worker who is not having contact with the patient (no gown/gloves), should be designated to touch surfaces After delivery to the patient room or the PACU, gloves and gowns removed, hand hygiene performed AORN - Personal Bags Fanny packs, backpacks, and briefcases should not be taken into the semirestricted or restricted areas of the perioperative suite. Constructed of porous materials, may be difficult to clean or disinfect adequately and may harbor pathogens, dust, and bacteria. The type of environmental surface and its ability to support microbial growth will influence microbial carriage. AORN Perioperative Standards and Recommended Practices, 2014 Edition Personal Bags Have to balance healthcare workers’ need to access reference materials and items to do job well Stipulations: Require the bag be dedicated to hospital use only Be made of material that can be cleaned Be stored away from the immediate patient care area Hand hygiene be done before accessing bag Conclusions Standardization of feedback by multiple IP to multiple areas helps keep involved parties informed Compilation of multi-pages of feedback into one-page dashboards helps keep the message focused Conclusions The credibility our department has built with all groups has allowed us to tackle some more challenging topics Overall, our continued efforts have resulted in a better relationship, which leads to better care for our patients Questions, Comments, Discussion? Kathleen McMullen kmm2742@bjc.org