09a-Reproductive Hormones-2010 Update - mr-youssef-mci
advertisement

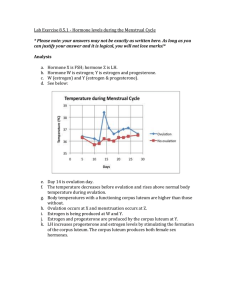
http://www.youtube.com/watch?v=WGJsrGmWeKE&feature=related Male Reproductive Hormones 1. androsterone 2. testosterone (Urinary bladder) Seminal vesicle (Rectum) (Pubic bone) Erectile tissue of penis Vas deferens Ejaculatory duct Prostate gland Urethra Bulbourethral gland Vas deferens Epididymis Glans penis Testis Scrotum Prepuce Seminal vesicle (behind bladder) (Urinary bladder) Prostate gland Urethra Scrotum Glans penis Bulbourethral gland Erectile tissue of penis Vas deferens Epididymis Testis Male Reproductive Hormones both hormones are released from testes Testes Cells 1. Leydig interstitial cells synthesize hormones (between seminiferous tubules) 2. Sertoli cells synthesize sperm within seminiferous tubules Testosterone Role stimulates spermatogenesis (production of mature sperm cells) – life time process develops male characteristics at puberty Gonadotropic Hormones gonadotropic hormones regulate gonad development (male and female) produced in the anterior pituitary; released upon hypothalamus signal 1. follicle stimulating hormone (FSH) 2. luteinizing hormone (LH) Male Gonad Development 1. Hypothalamus secretes gonadotropinreleasing hormone (GnRH) 2. Anterior pituitary gland releases FSH & LH 3. FSH stimulates Sertoli cells to form mature sperm 4. LH stimulates Leydig cells to secrete testosterone Male Gonad Development Role of testosterone: 1. promotes Sertoli cell activity - increases sperm cell production 2. negative feedback on hypothalamus - inhibits the hypothalamus by decreasing the secretion of FSH and LH from the anterior pituitary gland To Much Testosterone Stronger sex drive may lead to risky behaviours More impulsive and more aggressive Mood changes irritability and depression Stimuli from other areas in the brain Hypothalamus GnRH from the hypothalamus regulates FSH and LH release from the anterior pituitary. If testosterone levels get too high Anterior pituitary Negative feedback FSH acts on the Sertoli cells of the seminiferous tubules, promoting spermatogenesis. LH stimulates the Leydig cells to make testosterone, which in turn stimulates sperm production. Leydig cells make testosterone Primary and secondary sex characteristics Sertoli cells Figure 46.14 Spermatogenesis Testis Female Reproductive System 1. estrogen 2. progesterone Female Reproductive System both produced in the ovaries Ovaries Oviduct Follicles Uterus Uterine wall Endometrium Corpus luteum Cervix Vagina Female Reproductive System comparatively more complicated than male reproductive system Each ovary contains about 400,000 follicles at puberty Only about 400 eggs will mature and go through ovulation throughout a woman’s life Monthly cycle until menopause (~12 x 50 yrs) = 400450 cycles female hormones responsible for oogenesis (development of mature egg cells) and ovulation Ovary Follicle Cells 1. primary oocyte fertilized by sperm 2. granulosa cells provide nutrients for primary oocyte Female Reproductive System Female Gonad Development GnRH, FSH and LH involved 1. Hypothalamus secretes gonadotropin-releasing hormone (GnRH) 2. Anterior pituitary gland releases FSH & LH 3. FSH matures follicle 4. LH causes ovulation and causes corpus luteum maturation Menstrual/Ovarian Cycle Menstrual Cycle menstruation (flow phase) 1. Shedding of the endometrium Occurs only if there is no ovum fertilization estrogen and progesterone levels low follicular phase 2. Development of follicles estrogen secretion by granulosa cells Estrogen signals the endometrium to thicken Menstrual Cycle 3. ovulation ovum leaves ovary granulosa cells become corpus luteum corpus luteum begins to secrete progesterone estrogen levels start to decrease b Ovary Uterus Endometrium (a) From ovulation to implantation Endometrium Inner cell mass Cavity Blastocyst (b) Implantation of blastocyst Trophoblast Menstrual Cycle 4. luteal stage corpus luteum secretes progesterone & small amount of estrogen progesterone encourages endometrium development for embryo If no fertilization occurs = no embryo corpus luteum degenerates after about 10 days and produces a scar (corpus albicans) Concentrations of estrogen and progesterone decrease Causing weak uterine contractions (marking the beginning of the flow phase) http://www.youtube.com/watch?v=WGJsrGmWeK E&feature=related Can a female get pregnant before she has had her first period? YES! By the time she has reached puberty 400,000 follicles (no Corpus Luteum) Hypothalamus GnRH AP FSH, LH FSH induces development of follicles Ovulation occurs before menstruation! What regulates the events of the menstrual/ovarian cycle? Varying levels of LH and FSH determined by varying levels of estrogen and progesterone Many different positive and negative feedback mechanisms involved 1. Follicular Phase Low level of estrogen inhibits production of LH and FSH (keeping their levels low) Inhibits AP to prevent ovulation 2 3 1 2. Ovulation High estrogen stimulates LH and FSH production (more effect on LH than FSH) Stimulates AP to cause ovulation 3. Luteal Phase High levels of progesterone and estrogen inhibits LH and FSH production Inhibit AP and Hypothalamus 2 1 3 Menopause ovaries lose responsiveness to FSH and LH usually occurs between ages 46 and 54 most other mammals do not undergo menopause thought to allow human females to take care of grandchildren rather than continue to reproduce Man-opause? Andropause male menopause Decreased levels of testosterone Sex drive decreased Increase in memory loss Breast enlargement Body composition = more fat, less muscle More fat = more testosterone is converted to estrogen In class work Lab Exercise 8.5.1 (Hormone Levels During the Menstrual Cycle) Homework Section 8.5 – Page 399 #1—5,7-13