AchillesTendonInjuries SEP RES 3
advertisement

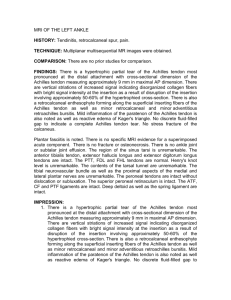
Johan Myburgh September 2011 Achilles Tendon Injuries Hippocrates “ this tendon if bruised or cut, causes the most acute fevers, induces choking, deranges the mind and at length brings death.” PATIENT • 31 year old male • Recreational soccer player • Work - oilfield worker • Healthy - no significant past hx • Played varsity soccer and football till 23 years old Injury • Came directly from work , no warm up • Previous tightness and tenderness calf few days • 5 minutes into game: Pushed off back to leg drive forward Sudden pain and weakness left leg 3 Stage Assessment 1. Clinical: • 80% acute partial Achilles tendon rupture • Previous sprain of Triceps surea • Improper warm up before activity 3 stage assessment 2. Personal: • concerned about the amount of time he is going to loose at work- no income. • positive about the outcome and wants to do proper rehabilitation to speed up his recovery 3. Contextual: • manager at work is supportive • seasonal work - needs to recover before the work season is over. • family is very supportive. Treatment • Nonoperative treatment plan o Immobilized equinis cast for 7 weeks o Removable walking splint for 6 weeks • Patient did 3 weeks o Physiotherapy starting at week 7 Progression: Week 13 physical exam: o Dorsiflexion L 96° R 105° o Tendon thickness L 30 mm R 19 mm Achilles tendon Anatomy • Formed by tendinous portion of gastrocnemius and soleus ( contribution varies) • Progresses from round to flat distally to insert on calcaneal tuberosity • Distal rotational twist (90°) o gastrocnemius fibers insert lateral o soleus fibers insert medial • Plantaris lies medial - distinct tendon (absent 6-8%) • No synovial sheath – wrapped paratenon Blood Supply o Posterior tibial artery - majority of the blood supply • Musculotendinous junction • Bone-tendon junction o Peroneal artery • Surrounding connective tissue (paratenon/mesotenon) Poor vascularization in midportion of tendon o Angiographic and histological techniques showed Achilles tendon has a poor blood supply throughout its length = small number of blood vessels per cross-sectional area(1,4) Histology • Fibroblasts (Embedded in bundles of fibrils) • Collagen comprises 70% of tendon o 95% type I o Ruptured tendon contains significant type III collagen • Collagen of granulation tissue - produced quickly by young fibroblasts before tougher type I collagen is synthesized Wavy bundles collagen Histology Collagen organized into parallel bundles of fibrils Surrounded by endotenon Units surrounded by vascular epitenon Pathology Achilles tendon disorders and overuse injuries: 1. Inflammation of the peritendinous tissue (peritendinitis,paratendinitis) 2. Degeneration of the tendon (tendinosis) 3. Tendon rupture • Partial/Complete • Acute/Chronic 4. Insertional disorders (retrocalcaneal bursitis and insertional tendinopathy) Tendinosis Degeneration with no significant inflammation: • Hypoxic or fibromatous: o most frequently seen in ruptured tendons • Myxoid o 2nd most common o May be silent prior to rupture • Lipoid o Age dependent fatty deposits that do not affect structural properties • Calcific o Calcium pyrophosphate Acute Rupture Achilles tendon Etiology – Intrinsic Factors • General • Decreased perfusion • Hyperthermia within relatively avascular Achilles tendon – more prone rupture • Systemic diseases Inflammatory and autoimmune conditions Collagen disorders Infectious disease Neurologic conditions • Age >30 • Decrease in maximum diameter & density of collagen fibrils Etiology – Extrinsic factors o General • Corticosteroids Corticosteroid injection into rabbit tendons showed necrosis and delayed healing. Several studies showed collagen damage with injected steroids. Oral steroids also implicated(2) • Fluoroquinolone(3) Etiology – Extrinsic factors • Biomechanical factors o Rapid push off Tendon obliquely loaded, muscle maximum contraction and initial short tendon length o Functional / Anatomical conditions • Imbalance agonist muscle contractions (7) • Functional overpronation on heel strike (midfoot) – whipping action on Achilles – intratendinous microtears • Poor flexibility gastroc/soleus - overpronation Etiology – Extrinsic factors • Biomechanical factors o Unequal tensile forces of different parts tendon torsional ischemic affect (transient vasoconstriction of intratendinous vessels, contribute vascular impairment already present) o Malfunction/Suppression of proprioceptive component of skeletal muscle (athletes resume training after period rest) Epidemiology • Incidence increasing significantly • 8.3 ruptures per 100 000 people(18) • Gender o Males 2:1 over females • Age (two peaks) o 30-50 – sports activity-related o > 50 – non-athletes and women • Sport o abrupt repetitive jumping o sprinting movements • Race - increased African-Americans(8) Histology of Rupture • Collagen degeneration of tendon prior to rupture(4) • Marked inflammatory reaction • Hypertrophy of tunica media and narrowing of lumen of large peritendinous vessels(1) - hypoxia All based on biopsy at time of surgical repair Site of Rupture Myotendinous Junction Midsubstance 2-6 cm proximal to insertion • Hypovascular Avulsion Diagnosis History Male between 30 and 50 years Sedentary job but in athletic activity “Weekend Warrior” Pop, “kicked” in the back of the leg Pain posteriorly in calf. Pain is variable Bruising Diagnosis Clinical dx Physical: Palpable defect Thompson Test Single leg heel raise Bruising/Swelling Weakness Thompson Test Patient prone with feet dangling - squeeze mid calf NO plantar flexion = positive Thompson test /Ruptured tendon Diagnosis • Diagnostic Tests o Ultrasound (Doubtful cases) • Helpful with Non-operative treatment Used to assess gap in tendon and apposition of torn ends of tendon o MRI (not routinely) • Show extent of tendon degeneration o X-rays • Avulsion of calcaneus suspected Ultrasound = Hematoma in Achilles tendon Most widely used U.K + Inexpensive Readily available, fast Dynamic assessment Tendon thickness Gap // torn ends − Operator dependent Miss partial tears MRI Most widely used imaging U.S + Accurate Partial tears − Not readily available High cost No dynamic assessment Classification of Achilles tendon tear/rupture (17) Nonoperative Treatment Effective for all age groups and both sedentary and sporting individuals • Wide variability among surgeons o absolute immobilization o initial range of movement exercises o progression weight bearing status • Cast immobilization 4-8 week (non-weight bearing) • Functional brace 4-6 weeks • Use ultrasound to ensure tendon apposition Nonoperative Treatment • Higher rerupture rate (13%) vs. operative repair (4-5%)(10) • Fewer overall complications ( wound infection) o Complications may be reduced with percutaneous surgery Acute Complete Rupture Surgical treatment Two Decisions Surgical technique Postoperative regime Surgical Technique • Direct Open (Incision 10-18 cm) • Mini-invasive (Incision 3-10 cm) • Percutaneous (multiple small incisions) Percutaneous Achilles Repair • vs. Open repair: o Higher rerupture rate (6.4% vs 2.7%) o Fewer complications • Allow earlier mobilization • Earlier functional rehabilitation • Sural nerve entrapment Open Repair Postero-medial incision Incision site reduce risk injury sural nerve and branches. Easier access plantaris muscle Plantaris tendon Percutaneous Repair Achillon Device Complications of Surgical Treatment • • • • • Wound healing problems/necrosis Wound infection Sural nerve injury DVT and PE Rerupture 2-5% Wound necrosis Chronic Rupture Definition: 4-6 weeks from time of injury to diagnosis and treatment • Conservative management not recommended • Fibrous tissue in gap between torn ends • Poor plantar flexion strength (2° flexors foot) • Open repair and reconstruction Postoperative Regime • Consensus Early functional weight bearing and range of motion decrease: Inpatient stay Time off from work Faster return to sport Lower complication rate • No Consensus DVT prophylaxis DVT common after Achilles tendon rupture No evidence to demonstrate benefit •Start ROM exercises Day 10 / earlier as per pt’s comfort •Day 14 weight bearing with restricted dorsiflexion Rehab Principles • Mobilization o Cycle 10-15 min/day • Loading o Treadmill Incline Walk (pain free) • Stretching o Straight, bend knee • Proprioception • Ankle eversion/inversion o Tubing Healing and Repair Mechanism Achilles Tendon Healing • Slow healing – hypovascularity + hypocellularity • Phases o o o o Inflammation Proliferation Repair Remodeling • Stress on tendon – remodeling ( similar to bones) o Stronger , stiffer o Achieved by increased collagen synthesis alteration fibre alignment • Mobilization increased inflammatory cells at rupture site(16) Tendon Healing bbbbbbbb Remodeling/Maturation Phase Remodeling/Consolidation Phase Reparative (Proliferation ) Phase Inflammatory Phase 24 hr 3 days 1 2 3 4 5 6 7 TIME - months 8 9 10 11 12 Histology healing Microscopic view of a normal Microscopic view of a tendon tendon undergoing healing wavy pink material is the collagen very few cells the white "bubble" is the suture note increase in cells Achilles Tendon Healing Important factors Tension across repair o speeds realignment fibres o increases tensile strength o minimize deformation Early motion o Accelerates nerve plasticity through regeneration and release neuromediators Sport Resumption • Time to return to sport depends level sport Average 20-24 weeks Olympic level up to nine months • Functional brace post-op 4 weeks earlier • Signs to slow down /speed up rehabilitation o Pain and swelling after activity o Delayed tissue healing - Ultrasound Sport Resumption Levels o Walking – Casted 12 weeks after surgery Brace 8 weeks after surgery o Recovery of force, speed and endurance - 4-6 weeks o Non-contact sport - 4-6 weeks o Contact sport – 4-6 weeks Take Home Message o Degeneration present at time of rupture o Early mobilization and weight bearing improved functional outcomes THANK YOU References 1. 2. 3. 4. 5. 6. 7. 8. 9. Ahmed, M. Lagopoulos, M., McConnell, P., Soarnes, R. W., Sefton, G. K Blood supply of the Achilles tendon. J. Orthop. Res. 16:591-596, 1998. Balasubramaniam P, Prathap K. The effectof injection of of hydrocortisone into rabbital calcaneal tendons. J. Bone and Joint Surgery 1972;54-B:729-734 Royer RJ, Pierfitte c, Netter P. Features of tendon disorders with fluoroquinolones. Therapie 1994;49:75-76 Weatherall, J, Mroczek, K, & Tejwani, N 2010, 'Acute Achilles tendon ruptures', Orthopedics, 33, 10, pp. 758-764 Maffulli,n, Barrass, V, Stanley W.B. Ewen, Light Microscopic Histology of Achilles Tendon Ruptures. A Comparison With Unruptured Tendons, Am J Sports Med November 2001 vol. 28 no. 6 857-863 Kannus, P., Jozsa, L. Histopathological changes preceding spontaneous rupture of a tendon. 1. Bone Joint Surg. 73-A:1507-1525, 1991. Waterson S. Subcutaneous rupture of Achilles tendon: Basic science and some aspectes of clinical practice. Br J Sports Med 1997;31:285-298 Davis JJ,Mason KT, Calrk DA. Achilles tendon ruptures stratified by age, race, and cause of injury among active duty U.S. Military members. Mil Med 1999;164:872-873 Steven B. Weinfeld, MD, Associate Professor of Orthopaedic Surgery Chief Foot and Ankle Service, Mount Sinai Medical Center, NY References 10. Lo IK, Kirkley A, Nonweiler B, Kumbare DA. Operative treatment vs non-operative treatment of acute Achilles tendon ruptures: A quantitative review. Clin J Sports Med1997;38:822-828 11. Forrester JC, ZederfeldtBH, Hayes TL. Wolff’s law in relation to the healing skin wound. Journal of Trauma-Injury Infection & Critical care 1970;10: 770-779 12. Virchenko O, Skoglund B, Aspenberg P. Parecoxib inpair early tendon repair but improves later remodeling. Am J Sports Med 2004;32;1743-1747 13. Virchenko O,Aspenberg P. How can one platelet injection after tendon injury lead to a stronger tendon after 4 weeks? Interplay between early regeneration and mechanical stimulation. Acta Orthopod 2006;77:806-812 14. Virchenko O, Lindahl T, Aspenberg P. Low Molecular Weight Heparin impairs tendon repair. J Bone Joint Surg (B) 2007: in press 15. Burssens P, steyaert A, Forsyth R, van Ovost EJ, Depaepe Y, Verdonk R. Exogenously administered substance P and neuropeptidase inhibitors stimulate fibroblast proliferation, angiogenesis and collagen organization durinf Achilles tendon healing. Foot Ankle Int 2005;26:832-839 16. Palmes et al J of Orthopaedic Research 2002 17. Kuwada GT. Classification of teno Achilles rupture with consideration of surgical repair techniques. J Foot Surg.1990;29:361-365 References 18. Suchak AA, Bostick G, Reid D, Blitz S. The incidence of Achilles tendon ruptures in Edmonton, Canada. Foot Ankle Int. 2005;26(11):932-936