download-link
advertisement

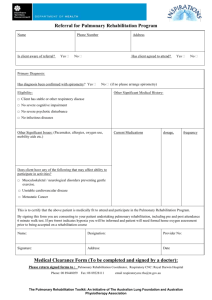
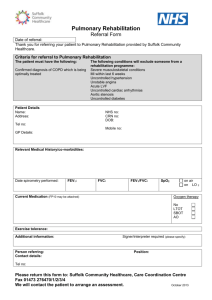
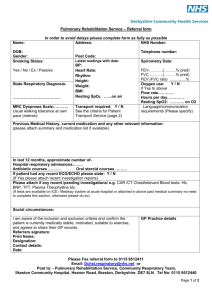
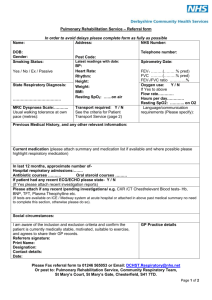
PULMONARY REHABILITATION Asthma/COPD Study Day 11/12/13 Fran Butler Respiratory Physiotherapist 1 Session Objectives • • • • • Background of pulmonary rehabilitation How it runs in York Outcomes of recent York groups Barriers to rehab Service development projects 2 Definition of Pulmonary Rehabilitation (PR) • ‘Pulmonary rehabilitation can be defined as an interdisciplinary programme of care for patients with chronic respiratory impairment that is individually tailored and designed to optimise each patient’s physical and social performance and autonomy. Programmes comprise individualised exercise programmes and education’. BTS (2013) 3 Guidelines NICE (2010) • People with COPD meeting appropriate criteria are offered an effective, timely and accessible multidisciplinary pulmonary rehabilitation programme 4 NICE GUIDELINES • Structure • a) Evidence of local arrangements to provide multidisciplinary pulmonary rehabilitation programmes. • b) Evidence of local arrangements to ensure effectiveness of multidisciplinary pulmonary rehabilitation programmes, by collection and audit of health outcome data. • c) Evidence of local arrangements to ensure multidisciplinary pulmonary rehabilitation programmes can be accessed in a timely manner. • d) Evidence of local arrangements to ensure multidisciplinary pulmonary rehabilitation programmes are geographically accessible. Aims of Pulmonary Rehabilitation Increase exercise tolerance and reduce dyspnoea Increase muscle strength and endurance (peripheral and respiratory) Improve health related quality of life Increase independence in daily functioning Increase knowledge of lung condition and promote self-management Promote long term commitment to exercise 6 Research The British Thoracic Society (BTS) guideline 2013 recommends that: • A program of exercise training of the muscles of ambulation is recommended as a mandatory component of pulmonary rehabilitation for patients with chronic obstructive pulmonary disease (COPD). • Pulmonary rehabilitation improves the symptom of dyspnea and improves Health Related Quality of Life in patients with COPD. • Six to 12 weeks of pulmonary rehabilitation produces benefits in several outcomes that decline gradually over 12 to 18 months. • Both low- and high-intensity exercise training produce clinical benefits for patient with COPD. Unsupported endurance training of the upper extremities is beneficial in patients with COPD and should be included in pulmonary rehabilitation programs. • Lower-extremity exercise training at higher exercise intensity produces greater physiologic benefits than lower-intensity training in patients with COPD. • The scientific evidence does not support the routine use of inspiratory muscle training as an essential component of pulmonary rehabilitation. • Education should be an integral component of pulmonary rehabilitation. Education should include information on collaborative self-management and prevention and treatment of exacerbations. • Pulmonary rehabilitation is beneficial for some patients with chronic respiratory diseases other than COPD. Examples of Effectiveness It has been found that following a course of pulmonary rehab patients demonstrated a significant reduction in health care utilization, both in hospital admissions and out patient attendances. Cost Analysis • For 1 patient to attend a rehab course costs approximately £375. • Average or 1.85 inpatient days saved At a average cost of £943.87 saved per patient • Average of 1 clinic appointment per patient saved at a cost of £59 • Total average saving per patient £1002.87 • So reduction in spending of £627.87 per patient Current provision for Pulmonary Rehabilitation in York • • • • Capacity of 10 programmes a year 4 in Selby (40 places) 4 in Wigginton (48 places) 2 in Foxwood (24 places) • Total capacity 112 11 Referral Sources • • • • • Respiratory Consultants Respiratory Nurses GP’s Practice Nurses Physiotherapists 12 Triage appointment • Explain concept of course to the patient • Check mobility • Check patient is on optimum treatment (not smoking) • Offer choice of location • Start home exercise programme and give breathing control advice • Additional advice about Chest clearance • Baseline SpO2 and Heart Rate • MRC scale Medical Research Council dyspnoea scale Grade Degree of breathlessness related to activities 1 Not troubled by breathlessness except on strenuous exercise 2 Short of breath when hurrying or walking up a slight hill 3 Walks slower than contemporaries on level ground because of breathlessness, or has to stop for breath when walking at own pace 4 Stops for breath after walking about 100m or after a few minutes on level ground 5 Too breathless to leave the house, or breathless when dressing or undressing • Adapted from Fletcher CM, Elmes PC, Fairbairn MB et al. (1959) The significance of respiratory symptoms and the diagnosis of chronic bronchitis in a working population. British Medical Journal 2:257-66. Triaging Possible exclusion criteria: 1. Loco motor problems 2. Significant cardiac disease 3. Cognitive impairment 4. Preferably non-smokers Non-compliance 1. Behavioural 2. Lack of social support 3. Continued smoking 4. Location and transport 15 Programme Format • Pre-course assessment • Two sessions of exercise and one education session per week for a total of six weeks • Post course assessment 16 Pulmonary Rehabilitation Programme Components Exercise programme (to continue at home) Education about the disease Self management strategies Breathing control techniques Effective chest clearance techniques Relaxation Energy saving strategies Benefits and social support Dietary advice 17 Assessments for the Pulmonary Rehabilitation Programme 1. CRDQ-Chronic Respiratory Disease Questionnaire 2. Incremental Shuttle Walk test 3. Spirometry 4. Pulse Oximetry 18 CRDQ • Measures the quality of life in patients with chronic lung disease. The questions are divided into four areas: • Dyspnoea • Fatigue • Emotional function • Mastery 19 Borg Scale Assessment of perceived breathlessness Level of breathlessness Score Nothing at all…………………………………………………………..0 Very, very slight (just noticeable)…………………………………....0.5 Very slight……………………………………………………………...1 Slight……………………………………………………………………2 Moderate…………………………………………………………….…3 Somewhat severe……………………………………………………..4 Severe…………………………………………………………………..5 / 6 Very severe………………………………………………………….... 7 / 8 Very, very severe (almost maximal)………………………………… 9 Maximal…………………………………………………………………10 20 Exercises • • • • Timed Circuit based exercise class Try to be functional Alternate arms then leg based exercise Can be progressed to remain challenging for patients • Able to adapt for patients with pre existing musculoskeletal problems • Most exercises can be replicated within the patients home 21 Non Completers • • • • • • • • Change in social circumstances (job) Exacerbation / hospital admission Transport issues Not for them Other health problems Lack of motivation RIP before course starts Unwell family member Maintenance of benefits Depends on: 1. 2. 3. 4. Patient motivation Disease deterioration Lifestyle/Behavioural change Frequency of exacerbations 23 On Going support • York HEAL Programmes • Breathe easy support and exercise group • Re referral back to group at later date • Home exercise programme/DVD 24 Pulmonary rehab in past 2 years Year 2011/2012 Offered Rehab 110 2012/2013 109 Completed Drop out Rehab rate 67 40% 65 40% 25 Outcomes of programmes 20112013 Year Greatest Average Improvement improvement in Shuttle Walk in Shuttle Walk 2011/ 240m 92m 2012 % improved MRC by at least 1 73% 2012/ 210m 2013 69% 69m 26 CRDQ results 2011-2013 % improvements Year Dyspnoea Fatigue Emotional Mastery Function 20112012 52% 74% 52% 61% 2012- 62% 2013 72% 63% 69% 27 Limitations to the Service - 2013 • Limited to 3 locations • Not a rolling programme • Limited availability to maintenance courses • Timing of referrals – patients having to wait several months for a course • Limited places due to hall space and staff to patient ratio Referrals to Rehab Total referrals April 2012April 2013 192 Total attended triage clinic 168 Total DNA clinic Total invited to rehab 22 • This data is for rehab referrals only 109 Audit review information April 2012April 2013 Referrals to Rehab 250 Number 200 150 100 50 0 Total referrals April 2012-April 2013 Total attended triage clinic Total invited to rehab Rehab Completion Rehab to Completion 120 Number 100 80 60 40 20 0 Total invited to Total attended Total completed rehab pre Ax for rehab course Outcomes for DNA’s to rehab 2012-2013 Outcomes for non-attendance at rehab RIP DNA Triage Clinic HEP only Declined Outcomes for DNA’s to rehab 2012-2013 • Some patients do not fit the inclusion criteria therefore are given a home exercise programme only • Some patients decline the programme and are also given a home exercise programme only • Some patients repeatedly DNA clinic appointments so are never triaged or given a home exercise programme Future Plans • Continued audit of the service • Starting a rolling programme in Selby – February 2014 • Capture as many COPD patients on the ward and refer to triage clinic for Ax for suitability for rehab • Education to referrers to improve uptake • PhD study into adherence in Pulmonary Rehabilitation – literature review into adherence, motivational/behavioural assessment tools, use of CBT in PR.