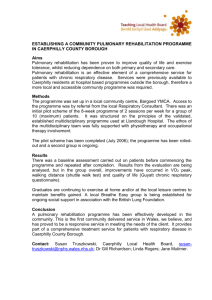
Angus Pulmonary Rehabilitation Programme
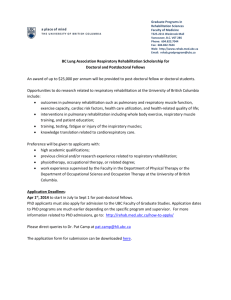
advertisement

Pulmonary Rehabilitation in COPD Maureen Fagan Respiratory Specialist Nurse “They tried to make me go to rehab, I said no, no, no....” Amy Winehouse diagnosed with emphysema From Times Online June 23, 2008 What is Pulmonary Rehabilitation? “…a multidisciplinary programme of care for patients with chronic respiratory impairment that is individually tailored and designed to optimise each patient’s physical and social performance and autonomy.” Spiral of Disability Why is it pulmonary rehabilitation important? • COPD causes 30,000 deaths per year and leads to extensive morbidity. It incurs massive costs in relation to hospital admissions, incurring nearly 6 times as many bed days of inpatient care as asthma. • Interventions which improve quality of life and level of functioning are important since few interventions except smoking cessation affect disease progression. Development of Disability in COPD • The decline in airway function may go unnoticed initially as people adapt their lives to avoid dyspnoea • Up to 50% of FEV1 may be lost before a person presents with significant symptoms • Significant disability develops late in the course of the disease when reversal of airway obstruction is not possible. • Dyspnoea , Limb muscle dysfunction, hypoxaemia , poor nutrition, steroid myopathy and loss of confidence may contribute to disability Aims • Increase exercise tolerance • Increase muscle strength and endurance • Reduce dyspnoea and perception of breathlessness • Reverse deconditioning • Increase knowledge of lung condition and management of the disease • Promote self-management and coping strategies • Improve health-related quality of life • Improve confidence in ability to exercise • Increase independence in daily functioning • Promote long-term commitment to exercise Who is it for? • All disease severities (but may not benefit if unable to walk) • …where SYMPTOMS AND DISABILITY are present (usually MRC grade 3) Who is it for? • All disease severities (but may not benefit if unable to walk) • …where SYMPTOMS AND DISABILITY are present (usually MRC grade 3) • No justification for selection on basis of age, impairment, disability, smoking status or oxygen use • Post exacerbation • Contra-indicated if recent MI/ unstable angina/ Course Content and Duration • • • • • • • • • • • The longer the better but usually 6-12 weeks Twice weekly minimum Patient assessment Baseline and outcome assessments: exercise capacity (shuttle walk), disability/health status (questionnaire) Exercise training upper limb and lower limb training/ respiratory muscle training / breathing exercises Optimal pharmacological management Educational support - can include carer Psychological support - can include carer Assessment of outcome Programme evaluation Maintenance Programme settings & staffing • Effective in inpatient, outpatient and community settings and possibly at home. • Should be held at times that suit patients in buildings that are easy to access with appropriate access for those with disabilities. Patient Safety Staff patient ratio • Exercise 1:8 • Education 1:16 Staff trained in Basic life support Ambulatory O2 Exercise Training: Which muscle groups? • Lower limb training improves exercise tolerance though no effect on measured lung function • Upper limb training improves arm strength and reduces ventilatory demand • Respiratory muscle training may influence endurance and dyspnoea but evidence is conflicting • DOESN’T HAVE TO BE HI TECH Education Programme • • • • • • • • • • • COPD – overview Breathing control, pacing and relaxation Exercise/activity Medication, devices and O2 therapy Managing exacerbations Sputum clearance OT equipment Benefits agency Holidays Palliative care Diet Psychological components • COPD is associated with anxiety and depressive symptoms which may interfere with activities of daily living (ADL’s) • Expert opinion supports the use of educational and psychological interventions in pulmonary rehab programmes • Typical goals: address depression/anxiety, teach relaxation skills, coping strategies, discuss relevant issues such as sexuality, family and work relationships Patient Feedback • • • • • • • • • • • Programme as a whole was excellent Wished it was longer Have got my life back Im now in control Much more confident Achieved goals and more Can relax better My illness no longer runs my life Can walk further My life now feels worth living again Feel better about myself Summary - Benefits of Pulmonary Rehabilitation • • • • • Improved exercise capacity (Evidence A) Improved health-related quality of life (Evidence A) Reduces perceived intensity of breathlessness (Evidence A) Reduced hospitalisations and length of stay (Evidence A) Reduced anxiety and depression associated with COPD (Evidence A) • Increased survival (Evidence B) • Benefits probably extend well beyond the period of rehab, especially if exercise training is maintained at home. (Evidence B) • Improved psychological wellbeing (Evidence C) References • NICE: National clinical guidelines on management of COPD in adults in primary and secondary care (2010) • GOLD: Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease (2009) • Nici et al. ATS/ERS Pulmonary Rehabilitation Writing Committee American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173:1390-413 • Y Lacasse, L Brosseau, S Milne, S Martin, E Wong, GH Guyatt, RS Goldstein, White J, Pulmonary rehabilitation for chronic obstructive pulmonary disease (Cochrane review). In: The Cochrane Library, issue 3, 2004. • Pulmonary Rehabilitation Joint ACCP/AACVPR Evidence-Based Guidelines. Chest/ 112 / 5 / November 1997 Resources GPIAG Best Practice Statement • www.gpiag.org/resources/gpiag_pul_rehab_bestpractice.200306.pdf IMPRESS Principles Document • www.ipmpressresp.com/portals/o/IMPRESS/PrinciplesofPR.pdf Patient Information • http://www.chss.org.uk/chest/index.php Thanks for listening. Any Questions ?