bilateralendocardial heart tubes
advertisement

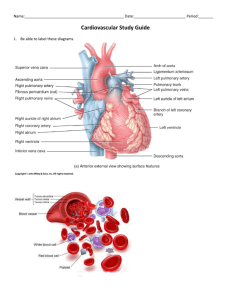
Development of the heart and vascular system begins very early in mesoderm both within (embryonic) and outside (extra embryonic, yolk sac and placental) the embryo. Vascular development therefore occurs in many places, the most obvious though is the early forming heart, which grows rapidly creating an externally obvious cardiac "bulge" on the early embryo. The heart forms initially in the embryonic disc as a simple paired tube inside the forming pericardial cavity, which when the disc folds, gets carried into the correct anatomical position in the chest cavity. Throughout the mesoderm, small regions differentiate into "blood islands" which contribute both blood vessels (walls) and fetal red blood cells. These "islands" connect together to form the first vessels which connect with the heart tube. Forms initially in splanchnic mesoderm of prechordal plate region - cardiogenic region Day 22 - 23, begins to beat in humans heart tube connects to blood vessels forming in splanchnic and extraembryonic mesoderm Week 2 - 3 pair of thin-walled tubes Week 3 paired heart tubes fuse, truncus arteriosus outflow, heart contracting Week 4 heart tube continues to elongate, curving to form S shape Week 5 Septation starts]], atrial and ventricular growth and folding of the embryo moves heart ventrally and downward into anatomical position Septation continues, atrial septa remains open, foramen ovale Week 37-38 At birth, pressure difference closes foramen ovale leaving a fossa ovalis Myocardium: forms from splanchnic mesoderm surrounding the pericardial coelom. Additional myocardial cells are added to the outflow tract during heart looping. Cardiac Jelly: gelatinous connective tissue separating the myocardium and heart tube endothelium. Endocardium: forms from the endothelium of the heart tube. Epicardium: develops from mesothelial cells arising from the sinus venosus which spread cranially over the myocardium. The heart primordium arises predominantly from splanchnic mesoderm in the cardiogenic region of the trilaminar embryo. The cardiogenic region can be thought of as bilateral fields that merge cranially to form a horseshoe-shaped field. During the third week of development (approximately day 18) angioblastic cords develop in this cardiogenic mesoderm and canalise to form bilateralendocardial heart tubes. The sinus venosus is also divided into two parts: the right horn of the sinus venosus and the left horn of the sinus venosus. By day 22, coordinated contractions of the heart tube are present and push blood cranially from the sinus venosus. As the embryo folds, the cranial ends of the dorsal aortae are pulled ventrally until they form a dorsoventral loop: the first aortic arch arteries The steps in looping can be summarised as: The straight heart tube begins to elongate with simultaneous growth in the bulbus cordis and primitive ventricle. This forces the heart to bend ventrally and rotate to the right, forming a C-shaped loop with convex side situated on the right. The ventricular bend moves caudally and the distance between the outflow and inflow tracts diminishes. The atrial and outflow poles converge and myocardial cells are added, forming the truncus arteriosus. Two endocardial cushions form on the dorsal and ventral surfaces of the AV canal, referred to as the superior and inferior cushions respectively. The cardiac jelly in this region expands while mesenchymal cells from the endocardium invade the cushions, allowing them to grow and fuse. This fusion divides the common AV canal into the right and left canals, hence partially separating the primitive atrium and ventricle. Two smaller endocardial cushions also form on the lateral walls of the AV canal, which later help to form the mitral and tricuspid heart valves. Membranous tissue forming the septum primum grows from the roof of the atrium, dividing it into left and right halves Blood flows from the right atrium through the foramen ovale and foramen secundum to the left atrium, forming a right-to-left shunt. The remaining portion of the septum primum acts as the valve of the foramen ovale. Blood cannot flow in the opposite direction, as the muscular strength of the septum secundum prevents prolapse of the septum primum Minor trabeculations appear during early development of the primordial ventricle. Following growth of the ventricles further trabeculations appear and grow as larger, muscular structures. Some researchers believe that as the trabeculations grow they coalesce resulting in the formation of the ventricular septum. However, the more commonly described theory of septation begins with the appearance of a primordial muscular interventricular (IV) ridge developing in the floor of the ventricle near the apex. As either side of the ventricle grows and dilates, their medial walls fuse forming the prominent IV septum. The foramen located between the cranial portion of the IV septum and the endocardial cushions: the IV foramen, closes by the end of the seventh week as the bulbar ridges (see next section) fuse with the endocardial cushions. Active proliferation of neural crest mesenchymal cells in the bulbus cordis during the fifth week creates bulbar ridges which are continuous in thetruncus arteriosus. The neural crest cells migrate through the primordial pharynx and over the aortic arch arteries to reach the outflow tract. The bulbar ridges undergo a 180° spiral to create the helical aorticopulmonary septum. As the ridges grow and develop myocardium they fuse in a distalto-proximal direction. Fusion occurs during the sixth week, allowing for cleavage of the aorta and pulmonary trunk. The spiralling nature of the ridges causes the pulmonary trunk to twist around the aorta. Note that the bulbus cordis accounts for the smooth conus arteriosus (or infundibulum) in the right ventricle and the aortic vestibule in the left ventricle. There are four valves in the adult heart, depicted below. There are two AV valves which comprise leaflets as well as the structures that tether these leaflets to the ventricular walls. The aortic and pulmonary valves, termed the semilunar valves, are located in the aorta and pulmonary trunk respectively. They are each made of three cusps. The AV valves begin to form between the fifth and eighth weeks of development. The left AV valve has anterior andposterior leaflets and is termed thebicuspid or mitralvalve. The right AV valve has a third, small, septalcusp and thus is called thetricuspid valve. The valve leafletsare attached to the ventricular walls by thin fibrous chords: the chordae tendineae, which insert into small muscles attached to the ventricle wall: the papillary muscles. These structures are sculpted from the ventricular wall The semilunar valves are formed from the bulbar ridges and subendocardial valve tissue. The primordial semilunar valve consists of a mesenchymal core covered by endocardium. Excavation occurs, thinning the valve tissue thus creating its final shape. Upon folding of the embryo the paired dorsal aortae connecting to the cranial end of the heart tube are brought ventrally to form the first aortic arches. Additional aortic arches develop over the next few weeks which are later remodelled to form the arteries of the upper body. Caudal to the arches, the paired dorsal aortae fuse to form a single median dorsal aorta which develops the following branches: Ventral (gut) branches - derived from the vitelline arteries Lateral branches - supply retroperitoneal structures Dorsolateral branches (intersegmental arteries) supply the head, neck, body wall, limbs and vertebral column The vitelline venous system gives rise to the liver sinusoids and portal system and forms the ductus venosus which acts as a shunt from the umbilical vein to the IVC. The IVC is formed during a left-to-right shift in the embryonic veins and is composed of: A hepatic segment - from the hepatic vein and sinusoids A prerenal segment - from the right subcardinal vein A renal segment - from subcardinal and supracardinal anastomosis A postrenal segment - from right supracardinal vein The main function of these shunts is to redirect oxygenated blood away from the lungs, liver and kidney (whose functions are performed by the placenta). Oxygenated blood is carried from the placenta to the foetus in the umbilical vein, most of which then passes through the ductus venosus to the IVC while some blood supplies the liver via the portal vein. Blood from the liver drains into the IVC through the hepatic veins. The blood in the IVC is a mixture of oxygenated blood from the umbilical vein and desaturated blood from the lower limbs and abdominal organs (e.g. the liver). This blood enters the right atrium where most of it is directed to the left atrium through the foramen ovale and from here to the left ventricle and aorta. The remainder of the blood in the right atrium passes with blood from the SVC (from the head and upper limbs) to the right ventricle and pulmonary artery where most of it passes to the aorta via the ductus arteriosus. The blood passes from the aorta to the hypogastric arteries, umbilical arteries and then back to the placenta. A variety of developmental defects occur as a result of prenatal exposure to alcohol (ethanol) in utero. In humans, those defects are collectively classified as Fetal Alcohol Spectrum Disorders, with Fetal Alcohol Syndrome (FAS) representing the more severe defects. FAS is defined by pre- and post-natal growth retardation, minor facial abnormalities, and deficiencies in the central nervous system (CNS). In addition to those defects, prenatal exposure to alcohol impacts cardiogenesis, the developmental stage of heart formation. Prenatal exposure to alcohol induces a variety of abnormalities in the developing heart which include: atrial and ventricular abnormalities, issues with valve formation, and a potential increase in the risk of heart disease later in adulthood. The specific defects that have been observed from prenatal alcohol exposure include defects to the atrioventricular valves (tricuspid and mitral) that allow blood to flow backward into the atria; ventricular septal defects, commonly known as a “hole in the heart” between the left and right ventricles; enlargement of the left ventricle, the primary pumping chamber in the heart; and an increased risk of developing heart disease later in adult life. http://search.medicinenet.com/search/search _results/default.aspx?Searchwhat=1&query=m esoderm&I1=Search http://www.ncbi.nlm.nih.gov/pmc/articles/P MC1767109/ http://php.med.unsw.edu.au/embryology/in dex.php?title=Cardiovascular_System_Develo pment Langman's Medical Embryology 11th ed., Sadler, T W, (Thomas W.); Langman, Jan. Philadelphia : Wolters Kluwer Lippincott Williams & Wilkins Developmental Biology, 6th ed., Gilbert, Scott F; Sunderland (MA): Sinauer Associates; 2000 Larsen's human embryology 4th ed. Schoenwolf, Gary C; Larsen, William J, (William James). Philadelphia, PA : Elsevier/Churchill Livingstone O'Neil, Erica, "Effects of Prenatal Alcohol Exposure on Cardiac Development". Embryo Project Encyclopedia (2011-04-30). ISSN: 19405030 http://embryo.asu.edu/handle/10776/2097.