Cell injury - Amazon Web Services
advertisement

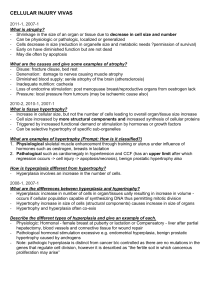
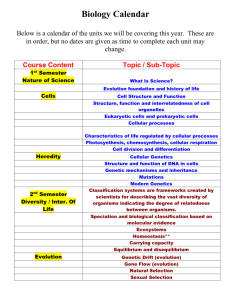
Cellular adaptation, cell injury and cell death I KAMPALA INTERNATIONAL UNIVERSITY DAR ES SALAAM COLLEGE Ssempijja Fred Anatomy Department OBJECTIVES 1. 2. 3. 4. To know the different cellular responses to injury , and its causes. To know the differents types of cell injury Explain the mechanisms and morphological changes in cell injury. To know some examples of cell injury. SUMMARY Cellular responses to injury. Definition. Cellular adaptation. Causes of cell injury. Cell injury . Mechanisms.Reversible and irreversible cell injury. Ischemic and hypoxic injury. Cellular injury by free radicals. Chemical injury. (Germany)1821- 1915. Introduced histopathology as a diagnostic branch by his cellular theory Microscopic study of the diseases is necessary for the diagnosis, each disease has specific changes in the cells and tissues. Book: Cellular pathology, 1858 Rudolf Virchow INJURY AGENT Any external or internal agent that acts over the cells and affect their capacity to keep the state called homeostasis. Cellular response to injury Nature and severity of injuriuos stimulus Cellular response Altered physiologic stimuli -Increased demand, increased trophic stimulation(grow factor, hormones) -Decreased nutrients, stimulation -Chronic irritation(chemical or physical Cellular adaptations -Hyperplasia, hypertrophy Reduced O2 supply, chemical injury, microbial infection -Acute and self-limited -Progressive and severe(including DNA damage) Cell injury -Mild chronic injury -Atrophy -Metaplasia -Acute reversible injury -Irreversible injury (cell death) •Necrosis •Apoptosis - Subcellular alteration in various organelles. Metabolic alteration, genetic or acquired Intracellular accumulations, calcifications Prolonged life span with cumulative sublethal injury Cellular aging CELL ADAPTATION Is the new but altered states of the cells’s structure and/or biochemical processes in order to achieve a new "steady state" and maintain near-normal physiologic functions (homeostasis) preserving its viability. Adaptative response NORMAL TISSUE Stimulus That increased demand Hyperplasia Stimulus that reduced demand Atrophy Hypertrophy End of stimuli Chronic irritation Metaplasia CELLULAR ADAPTATION HYPERPLASIA Is an increase in the number of parenchymal cells resulting in enlargement of the organ or tissue. Hyperplasia usually occurs together with hypertrophy. Takes place if the cellular population is capable of synthesizing DNA, thus permitting mitotic division. HYPERPLASIA Physiologic hyperplasia 1- Hormonal Proliferation of glandular epithelium of the female breast at puberty and during pregnancy 2- Compensatory After partial hepatectomy Pathologic hyperplasia 1- By excessive hormonal stimulation Endometrial hyperplasia Benign prostatic hyperplasia Endometrial hyperplasia CELLULAR ADAPTATION HYPERTROPHY Is an increase in the size of parenchymal cells resulting in enlargement of the organ or tissue, without any change in the number of cells. It may be physiologic or pathologic. HYPERTROPHY Physiologic hypertrophy • Growth of the uterus during pregnancy •Hypertrophy of breast during lactation. Pathologic Hypertrophy • Hypertrophy of cardiac muscle • Hypertrophy of smooth muscle • Hypertrophy of skeletal muscle • Compensatory hypertrophy HYPERTROPHY Normal muscle Hypertrophy muscle Cellular adaptation ATROPHY Reduction in the size of cells by loss of cell substance. When a sufficient number of cells are involved, the entire tissue or organ diminishes in size or become atrophic It may occur from physiologic or pathologic causes. ATROPHY Physiologic Atrophy • Atrophy of thymus after puberty • Atrophy of gonads after menopause • Atrophy of brain with aging • Notochord and thyroglossal duct during fetal development ATROPHY Pathologic Atrophy • Malnutrition atrophy • Denervation atrophy • Disuse atrophy • Pressure atrophy • Endocrine atrophy • Ischaemic atrophy ATROPHY CELLULAR ADAPTATION METAPLASIA Is defined as a reversible change of one type of adult cells (epithelial or mesenchymal) that are replaced by another type of adult cells, usually in response to abnormal stimuli, and often reverts back to normal on removal of stimulus. METAPLASIA • Epithelial metaplasia 1. Squamous metaplasia 2. Columnar metaplasia • Mesenchymal metaplasia 1. Osseous metaplasia 2. Cartilaginous metaplasia METAPLASIA Metaplasia, squamous, larynx, microscopic METAPLASIA If the influences that predispose to metaplasia persist, they may induce malignant transformation in metaplastic epithelium. CELL INJURY = DISEASE CELLULAR STRESS Intense of stimulus ADAPTATION Cellular vulnerability CELL INJURY Reversible Point of no return -------------------------- Irreversible CELLULAR DEATH INJURY AGENT loload ad Lesión celular irreversible IF THE LIMITS OF ADAPTIVE RESPONSE TO A STIMULUS ARE EXCEEDED OR WHEN THE CELL IS EXPOSED TO AN INJURIUS AGENT, CELL INJURY OCCUR. CELL INJURY Is the morphological and biochemical changes in the cell that occur when the cells are stressed so severely that they are no longer able to adapt or when cells are exposed to inherently damaging agents . Causes of cell injury • Hypoxia and ischemia • Physical agents • Chemical agents and drugs • Infection agents • Immunologic reactions • Genetic derangements • Nutritional imbalances Hypoxia and ischemia Hypoxia is a deficiency of oxygen, which causes cell injury by reducing aerobic oxidative respiration. Is the most common cause of cell injury. May be caused by anemia, Carbonmonoxide poisoning, cardiorespiratory insufficiency, and increased demand of tissues. Ischemia is a reduction of blood flow, compromises the supply not only of oxygen, but also of metabolic substrates, including glucose. Usually as a consequence of mechanical obstruction in the arterial system, fall in blood pressure or loss of blood. Physical agents • Mechanical trauma (e.g. road accidents); • Thermal trauma (e.g. by heat and cold); • Electricity; • Radiation (e.g. ultraviolet and ionising); • Rapid changes in atmospheric pressure. Chemicals and Drugs • Chemical poisons such as cyanide, arsenic, mercury; • Strong acids and alkalis; • Environmental pollutants; • Insecticides and pesticides; • Oxygen at high concentration; • Hypertonic glucose and salt; • Social agents such as alcohol and narcotic drugs; • Therapeutic administration of drugs. Infection agents • Bacteria; • Rickettsiae; • Viruses; • Fungi; • Protozoa; • Metazoa; • Other parasites. Immunologic reaction Immunity is a “double-edged sword” --- it protects the host against various injurious agents but it may also turn lethal and cause cell injury e.g. • Hypersensitivity reactions; • Anaphylactic reactions; • Autoimmune reactions. Genetic Derangements Genetic defects as causes of cell injury are of major interest to scientists and physicians today. • The genetic injury may result in a defect caused by a chromosomal abnormality (e.g. the congenital malformations associated with Down syndrome). • Variations in the genetic makeup can also influence the susceptibility of cells to injury by chemicals and other environmental insults. Nutritional imbalances A deficiency or an excess of nutrients may result in nutritional imbalances. • Nutritional deficiency diseases may be due to overall deficiency of nutrients (e.g. starvation), of protein calorie (e.g. marasmus, kwashiorkor), of minerals (e.g. anaemia), or of trace elements. • Nutritional excess is a problem of affluent societies resulting in obesity, atherosclerosis, heart disease and hypertension. FACTORS THAT DEPEND CELL INJURY INJURIOUS STIMULI • Type • Mechanisms of action • Duration • Severity CELL Type of cell- stable - labile - permanent • Nutritional state • • Adaptability of the cell to injury STAGES OF CELL INJURY REVERSIBLE CELL INJURY IRREVERSIBLE CELL INJURY OR CELL DEATH REVERSIBLE CELL INJURY Funtional and morphologic changes that are reversible if the damaging stimulus is removed. IRREVERSIBLE CELL INJURY Functional and morphologic changes in the cell that are irreversible at which time the cell cannot recover. Invariably undergo morphologic changes that are recognized as cell death. Essential cellular components affected in cell injury SISTEMAS INTRACELULARES VULNERABLES Integrity of cell Membranes and cytoskeleton Protein synthesis BIOCHEMICAL CHANGES STRUCTURAL CHANGES Aerobic respiration MORPHOLOGIC CHANGES Integrity of the genetic apparatus Mechanisms of cell injury • Depletion of ATP • Membrane damage • Influx of intracellular calcium and loss of calcium homeostasis • Accumulation of oxygen-derived free radicals (oxidative stress) ISCHEMIA TYPES OF CELL INJURY TOXIC FREE RADICALS Cellular swelling. ISCHEMIC Loss of microvilli Blebs ER swelling Influx of Ca2+,H2O, Na+ Myelin figures MITOCONDRIA Oxidative phosphorylation ATP Loss of K+ Na pump Glycolysis Detachment of Ribosomes Clumping of nuclear Chromatin pH Glycogen Protein synthesis REVERSIBLE INJURY Lipid deposition ISCHEMIA Membrane injury MITOCONDRIA Loss of Phospholipids Cytoskeletal alterations Leakage Enzymes, (CK, LDH) Lipids breakdown Ca2+ influx Free radicals Other Oxidative phosphorylation ATP pH Intracellular release and activation of lysosomal enzymes IRREVERSIBLE INJURY Ca2+ en las Mitocondrias Basophilia ( RNP) Nuclear changes Protein digestion Phenomena that characterize irreversibility Inability to reverse michondrial dysfunction. Profound disturbances in membrane function. Injury by free radicals Are reactive oxygen forms produced in mitochondrial respiration (O2-) Superoxide anion radical (H2O2) Hydrogen peroxide (OH) Hydroxyl ions They can damage protein, lipid and nucleid acid. Free radical- mediated damage contributes to such varied processes as : -Chemical and radiation injury -Ischemia-reperfusion injury -Cellular aging -Microbial killing by phagocytes Enzymatic metabolism Chemicals Drugs ReductionOxidation Reactions Absorption of radiant energy FREE RADICALS Transition metal Nitric oxide O2 Oxidative enzymes O2.Fe2+ O2.- superoxide H2O2 dismutase Lipid peroxidation of membranes Fe3+ OH. + OH- H2O Oxidative modification proteínas Lesion in DNA Cellular injury MECHANISMS FOR INACTIVATION FREE RADICAL REACTIONS ANTIOXIDANTS ENZYMES IRON AND COPPER CHEMICAL INJURY Induce cellular injury by two general mechanisms - Directly by combining with some critical molecular component or cellular organelle.(E.g,mercuric chloride poisoning) - Some chemical are not biologically active but must be converted to reactive toxic metabolites in the ER of the liver and other organs. CCL4 REL Chemical injury CCL3 LIPID RADICALS +O2 LIPID PEROXIDATION MEMBRANE DAMAGE (RER) DAMAGE TO PLASMA MEMBRANE -INACTIVATION: APOPROTEIN SYNTHESIS FATTY LIVER .MITOCHONDRIA . CELL ENZYMES -DESNATURATION OF PROTEINS DIRECTLY Chemical injury FREE RADICALS MORPHOLOGY OF REVERSIBLE CELL INJURY (DEGENERATION OR INTRACELLULAR ACUMULATION) •Cellular swelling • Fatty change • Hyaline change • Amyloidosis • Pigments • Pathologic calcification Cellular Swelling Cellular swelling is the first manifestation of almost all forms of injury to cells. Other synonyms of cellular swelling used in the past are: cloudy swelling (for gross appearance of the affected organ) hydropic change (accumulation of water within the cell) vacuolar degeneration (due to cytoplasmic vacuolation) Cellular swelling Grossly, the affected organ such as kidney, liver or heart muscle is enlarged due to swelling. The cut surface bulges outwards and is slightly opaque • HYDROPIC CHANGE HYDROPIC CHANGE Fatty change (Steatosis) The terms fatty change and steatosis describe abnormal accumulations of triglycerides within parenchymal cells. • Fatty change is often seen in the liver because it is the major organ involved in fat metabolism, but it also occurs in heart, muscle, and kidney. Causes: - Toxins - Protein malnutritions - Obesity - Diabetes mellitus - Anoxia Fatty change (Steatosis) Causes - Toxins Protein malnutritions Obesity Diabetes mellitus Anoxia Alcohol abuse Fatty liver Histochemical – – – – – – Sudán Oil Red Sudan Black Orange oil PAS If the stain is Negative for fat or glycogen is water, Hyaline Change • The word “Hyaline” means glassy (hyalos =glass). • Hyaline is a descriptive histologic term for glassy, homogeneous, eosinophilic appearance of material in H.E stained sections and does not refer to any specific substance. • Hyaline change is associated with heterogeneous pathologic conditions and may be intracellular or extracellular. Intracellular Hyaline • Intracellular hyaline is mainly seen in epithelial cells. For example: 1. Hyaline droplets in the proximal tubular epithelial cells in cases of excessive reabsorption of plasma. 2. Mallory’s hyaline represents aggregates of intermediate filaments in the hepatocytes in alcoholic liver cell injury. Intracellular Hyaline 3. Nuclear or cytoplasmic hyaline inclusions seen in some viral infections. 4. Russel’s bodies representing excessive immunoglobulins in the RER of the plasma cells. Extracellular Hyaline • Extracellular hyaline is seen in connective tissues. A few examples of extracellular hyaline change are: 1. Hyaline degeneration in leiomyomas of the uterus. 2. Hyalinised old scar of fibrocollagenous tissues. 3. Hyaline arteriosclerosis is renal vessels in hypertension and diabetes mellitus. 4. Hyalinised glomeruli in chronic glomerulonephritis. REFERENCE 1. 2. 3. Muir’s Textbook of Pathology, edition above 13th General Pathology by Walter and Isreal Robbins and Cotran, Pathologic Basis of disease, editions above 7th