The Small Intestine
advertisement

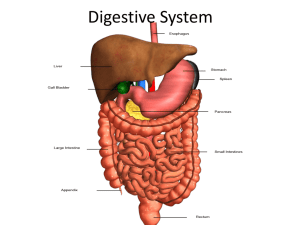
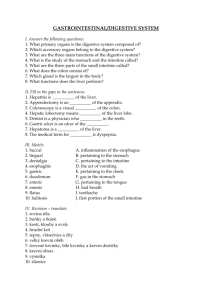
The Digestive System OVERVIEW OF THE DIGESTIVE SYSTEM The organs of the digestive system fall into two main groups: 1- Alimentary canal, also called the gastrointestinal (GI) tract or gut, It digests food—breaks it down into smaller fragments (digest = dissolved)—and absorbs the digested fragments through its lining into the blood. -The organs of the alimentary canal are the mouth, pharynx, esophagus, stomach, small intestine, and large intestine. -In a cadaver, the alimentary canal is approximately 9 m (about 30 ft) long, but in a living person, it is considerably shorter because of its muscle tone. . - Food material in this tube is technically outside the body because the canal is open to the external environment at both ends. 2- The accessory digestive organs are the teeth, tongue, gallbladder, and a number of large digestive glands—the salivary glands, liver, and pancreas. -The teeth and tongue are in the mouth, or oral cavity, while the digestive glands and gallbladder lie outside the GI tract and connect to it by ducts. Digestive System Organs The Mouth The mouth, a mucosa-lined cavity, is also called the oral cavity, or buccal cavity (buk′al). - Its boundaries are the lips (labia) anteriorly, cheeks laterally, palate superiorly, and tongue inferiorly . - Its anterior opening is the oral orifice. Posteriorly, the oral cavity is continuous with the oropharynx. - It is lined with stratified squamous epithelium which can withstand considerable friction. - The space bounded externally by the lips and cheeks and internally by the gums and teeth is called the vestibule . - The area that lies within the teeth and gums is the oral cavity proper. • The palate, forming the roof of the mouth, has two distinct parts: the hard palate anteriorly and the soft palate posteriorly. • The hard palate is formed by the palatine bones and the palatine processes of the maxillae, and it forms a rigid surface against which the tongue forces food during chewing. • The soft palate is a mobile fold formed mostly of skeletal muscle. Projecting downward from its free edge is the fingerlike uvula (u′vu-lah). The soft palate rises reflexively to close off the nasopharynx when we swallow. The Tongue The tongue occupies the floor of the mouth and fills most of the oral cavity when the mouth is closed. • A fold of mucosa, called the lingual frenulum, secures the tongue to the floor of the mouth and limits posterior movements of the tongue. • Children born with an extremely short lingual frenulum are often referred to as “tongue-tied” because of speech distortions that result when tongue movement is restricted. This congenital condition, called ankyloglossia (“fused tongue”), is corrected surgically by snipping the frenulum. • The Pharynx From the mouth, food passes posteriorly into the oropharynx and then the laryngopharynx ,both common passageways for food, fluids, and air. (The nasopharynx has no digestive role.) The mucosa contains a friction-resistant stratified squamous epithelium well supplied with mucus-producing glands. • The Esophagus A muscular tube about 25 cm (10 inches) long, is collapsed when not involved in food propulsion. The presence of the stratified squamous epithelium indicates the esophagus is to accommodate high friction. The esophagus takes a fairly straight course through the mediastinum of the thorax and pierces the diaphragm at the esophageal hiatus to enter the abdomen. It joins the stomach at the cardiac orifice. The cardiac orifice is surrounded by the gastro-esophageal or cardiac sphincter acts as a valve. The muscular diaphragm, which surrounds this sphincter, helps keep it closed when food is not being swallowed. • Histology of the Alimentary Canal From the esophagus to the anal canal, the walls of the alimentary canal have the same four basic layers : 1-The mucosa, or mucous membrane—the innermost layer—is a moist epithelial membrane that lines the alimentary canal lumen from mouth to anus. Its major functions are (1) secretion of mucus, digestive enzymes, and hormones, (2) absorption of the end products of digestion into the blood, and (3) protection against infectious disease. 2- The Submucosa just external to the mucosa, is a moderately dense connective tissue containing blood and lymphatic vessels, lymphoid follicles, and nerve fibers. 3-The Muscularis Externa This layer is responsible for segmentation and peristalsis. It typically has an inner circular layer and an outer longitudinal layer of smooth muscle cells .In several places along the tract, the circular layer thickens, forming sphincters that act as valves to prevent backflow and control food passage from one organ to the next. 4-The Serosa The outermost layer which is the visceral peritoneum. It is formed of a single layer of squamous epithelial cells. In the esophagus, which is located in the thoracic instead of the abdominopelvic cavity, the serosa is replaced by an adventitia (ad″ven-tish′e-ah). • HOMEOSTATIC IMBALANCE Heartburn, the first symptom of gastroesophageal reflux disease (GERD), is the burning, radiating substernal pain that occurs when the acidic gastric juice regurgitates into the esophagus. Heartburn is most likely to happen in conditions that force abdominal contents superiorly, such as extreme obesity, pregnancy, and running, which causes stomach contents to splash upward with each step (runner’s reflux). It is also common in those with a hiatal hernia, in which the superior part of the stomach protrudes slightly above the diaphragm. If the episodes are frequent and prolonged, esophagitis (inflammation of the esophagus) and esophageal ulcers may result. • The Stomach Below the esophagus, the GI tract expands to form the stomach ,a temporary “storage tank” where chemical breakdown of proteins begins and food is converted to a creamy paste called chyme (kīm; “juice”). The stomach lies in the upper left quadrant of the peritoneal cavity, nearly hidden by the liver and diaphragm. Specifically, it lies in the left hypochondriac, epigastric, and umbilical regions of the abdomen. Though relatively fixed at both ends, the stomach is quite movable in between. • The adult stomach varies from 15 to 25 cm (6 to 10 inches) long, but its diameter and volume depend on how much food it contains. An empty stomach has a volume of about 50 ml and a cross-sectional diameter only slightly larger than the large intestine, but when it is really distended it can hold about 4 L (1 gallon) of food and may extend nearly all the way to the pelvis! When empty, the stomach collapses inward, throwing its mucosa (and submucosa) into large, longitudinal folds called rugae . • The small cardiac region, or cardia (“near the heart”), surrounds the cardiac orifice through which food enters the stomach from the esophagus. The fundus is its dome-shaped part, that bulges superolaterally to the cardia. The body, the midportion of the stomach, is continuous inferiorly with the funnel-shaped pyloric region. The pylorus is continuous with the duodenum through the pyloric sphincter, which controls stomach emptying (pylorus = gatekeeper). • The convex lateral surface of the stomach is its greater curvature, and its concave medial surface is the lesser curvature. Extending from these curvatures are two mesenteries, called omenta (o-men′tah), that help tether the stomach to other digestive organs and the body wall • The lesser omentum runs from the liver to the lesser curvature of the stomach, where it becomes continuous with the visceral peritoneum covering the stomach. • The greater omentum from the greater curvature of the stomach to cover the coils of the small intestine. The greater omentum is riddled with fat deposits. It also contains large collections of lymph nodes. • The immune cells and macrophages in these nodes “police” the peritoneal cavity and intraperitoneal organs. • Microscopic Anatomy of the stomach The stomach wall contains the four layers typical of most of the alimentary canal .Besides the usual circular and longitudinal layers of smooth muscle, there is a layer that runs obliquely . The lining epithelium of the stomach mucosa is a simple columnar epithelium composed entirely of goblet cells, which produce a protective coat of alkaline mucus .This otherwise smooth lining is dotted with millions of deep gastric pits which lead into the gastric glands that produce the stomach secretion called gastric juice. The cells forming the walls of the gastric pits are primarily goblet cells. The glands in these pits contain a variety of secretory cells, including the four types described here: 1. Mucous neck cells, found in the upper, or “neck,” regions of the glands, produce mucus . 2. Parietal cells, secrete hydrochloric acid (HCl) and intrinsic factor. -HCl makes the stomach contents extremely acidic (pH 1.5–3.5), a condition necessary for activation and optimal activity of pepsin. The acidity also helps in food digestion by denaturing proteins and breaking down cell walls of plant foods, and can kill many of the bacteria ingested with foods. - Intrinsic factor is a glycoprotein required for vitamin B12 absorption in the small intestine. 3. Chief cells produce pepsinogen (pep-sin′o-jen), the inactive form of the protein-digesting enzyme pepsin. 4. Enteroendocrine cells (en″ter-o-en′do-krin; “gut endocrine”) release a variety of chemical messengers. Some of these, for example histamine and serotonin, act locally. Others, such as somatostatin, act both locally and as hormones . Gastrin, a hormone, plays essential roles in regulating stomach secretion and motility. • The Small Intestine The small intestine is the body’s major digestive organ. Within its twisted passageways, digestion is completed and virtually all absorption occurs. Gross Anatomy The small intestine is a convoluted tube extending from the pyloric sphincter in the epigastric region to the ileocecal valve in the right iliac region where it joins the large intestine .It is the longest part of the alimentary tube, but is only about half the diameter of the large intestine, ranging from 2.5 to 4 cm (1– 1.6 inches). Although it is 6–7 m long in a cadaver, the small intestine is only about 2–4 m (7–13 ft) long during life because of muscle tone. • The small intestine has three subdivisions: -the duodenum, is relatively immovable “twelve finger widths long”, which curves around the head of the pancreas ,is about 25 cm (10 inches) long. Although it is the shortest intestinal subdivision, the duodenum has the most features of interest. The bile duct, delivering bile from the liver, and the main pancreatic duct, carrying pancreatic juice from the pancreas, unite in the wall of the duodenum in the hepatopancreatic ampulla . The ampulla opens into the duodenum and is controlled by a muscular valve called the hepatopancreatic sphincter, or sphincter of Oddi. • The jejunum ,about 2.5 m (8 ft) long, extends from the duodenum to the ileum. • The ileum ,approximately 3.6 m (12 ft) in length, joins the large intestine at the ileocecal valve. The jejunum and ileum hang in sausagelike coils in the central and lower part of the abdominal cavity, suspended from the posterior abdominal wall by the fan-shaped mesentery .These more distal parts of the small intestine are encircled and framed by the large intestine. The nutrient-rich venous blood from the small intestine drains into the hepatic portal vein, which carries it to the liver. • Modifications for Absorption : - Its length alone provides a huge surface area, and - its wall has three structural modifications that amplify its absorptive surface enormously (by a factor of more than 600 times). Most absorption occurs in the proximal part of the small intestine, so these specializations decrease in number toward its distal end. 1- The circular folds, or plicae circulares are deep, permanent folds of the mucosa and submucosa . Nearly 1 cm tall, these folds force chyme to spiral through the lumen, slowing its movement and allowing time for full nutrient absorption. 2-Villi are fingerlike projections of the mucosa .In the core of each villus is a dense capillary bed and a wide lymph capillary called a lacteal . The villi are large and leaflike in the duodenum (the intestinal site of most active absorption) and gradually narrow and shorten along the length of the small intestine. 3- Microvilli, tiny projections of the plasma membrane of the absorptive cells of the mucosa, give the mucosal surface an appearance called the brush border .The plasma membranes of the microvilli bear enzymes referred to as brush border enzymes, which complete the digestion of carbohydrates and proteins in the small intestine. The Large Intestine The large intestine frames the small intestine on three sides and extends from the ileocecal valve to the anus. Its diameter, at about 7 cm, is greater than that of the small intestine (hence, large intestine), but it is less than half as long (1.5 m versus 6 m). Its major function is to absorb most of the remaining water from indigestible food residues (delivered to it in a fluid state), store the residues temporarily, and then eliminate them from the body as semisolid feces (fe′sēz). • Gross Anatomy -The large intestine has two features not seen elsewhere : -the longitudinal muscle layer is reduced to three bands of smooth muscle called teniae coli . -Their tone causes the wall of the large intestine to pucker into pocketlike sacs called haustra . -The large intestine has the following subdivisions: cecum, appendix, colon, rectum, and anal canal. -The saclike cecum (se′kum; “blind pouch”), which lies below the ileocecal valve in the right iliac fossa, is the first part of the large intestine . -Attached to its posteromedial surface is the blind, wormlike vermiform appendix. The appendix contains masses of lymphoid tissue, and as part of MALT, it plays an important role in body immunity. Its twisted structure provides an ideal location for enteric bacteria to accumulate and multiply. • The colon has several distinct regions: -the ascending colon, it travels up the right side of the abdominal cavity to the level of the right kidney. -Here it makes a right-angle turn—the right colic, or hepatic, flexure— and travels across the abdominal cavity as the transverse colon. -Directly anterior to the spleen, it bends acutely at the left colic (splenic) flexure and descends down the left side of the posterior abdominal wall as the descending colon. -Inferiorly, it enters the pelvis, where it becomes the S-shaped sigmoid colon. • In the pelvis, at the level of the third sacral vertebra, the sigmoid colon joins the rectum, which runs just in front of the sacrum. The position of the rectum allows the prostate gland of males to be examined digitally (with a finger) through the anterior rectal wall. This is called a rectal exam. • The anal canal, the last segment of the large intestine, lies in the perineum, entirely external to the abdominopelvic cavity. About 3 cm long, it begins where the rectum penetrates the levator ani muscle of the pelvic floor and opens to the body exterior at the anus. The anal canal has two sphincters, an involuntary internal anal sphincter composed of smooth muscle and a voluntary external anal sphincter composed of skeletal muscle. The sphincters, which act rather like purse strings to open and close the anus, are ordinarily closed except during defecation. Accessory Digestive organs • The Teeth The teeth lie in sockets (alveoli) in the gum-covered margins of the mandible and maxilla. We masticate, or chew, by opening and closing our jaws and moving them from side to side while continually using our tongue to move the food between our teeth. Teeth are classified according to their shape and function as incisors, canines, premolars, and molars . Ordinarily by age 21, two sets of teeth: - The primary dentition consists of the deciduous teeth, also called milk or baby teeth. The first teeth to appear, at about age 6 months, are the lower central incisors. Additional pairs of teeth erupt at one- to twomonth intervals until about 24 months, when all 20 milk teeth have emerged. - As the deep-lying permanent teeth enlarge and develop, the roots of the milk teeth are resorbed from below, causing them to loosen and fall out between the ages of 6 and 12 years. Generally, all the teeth of the permanent dentition (but the third molars) have erupted by the end of adolescence. -The third molars, also called wisdom teeth, emerge between the ages of 17 and 25 years. There are usually 32 permanent teeth in a full set, but sometimes the wisdom teeth are completely absent. • Tooth Structure Each tooth has two major regions: the crown and the root .The enamel-covered crown is the exposed part of the tooth above the gingiva (jin′jĭ -vah), or gum, which surrounds the tooth like a tight collar. Enamel, an acellular, brittle material that directly bears the force of chewing, is the hardest substance in the body. • The crown and root are connected by a constricted tooth region called the neck. The outer surface of the root is covered by cementum, a calcified connective tissue, which attaches the tooth to the thin periodontal ligament (per″e-o-don′tal; “around the tooth”). This ligament anchors the tooth in the bony alveolus of the jaw. • Dentin, a bonelike material, underlies the enamel cap and forms the bulk of a tooth. It surrounds a central pulp cavity containing a number of soft tissue structures (connective tissue, blood vessels, and nerve fibers) collectively called pulp. Pulp supplies nutrients to the tooth tissues and provides for tooth sensation. • Where the pulp cavity extends into the root, it becomes the root canal. At the proximal end of each root canal is an apical foramen that allows blood vessels, nerves, and other structures to enter the pulp cavity. • In youth, the gingiva adheres to the enamel covering the crown. But as the gums begin to recede with age, as a result, the teeth appear to get longer in old age. • HOMEOSTATIC IMBALANCE When a tooth remains embedded in the jawbone, it is said to be impacted. Impacted teeth can cause a good deal of pressure and pain and must be removed surgically. Wisdom teeth are most commonly impacted . • The Salivary Glands A number of glands associated with the oral cavity secrete saliva which. (1) cleanses the mouth, (2) dissolves food chemicals so that they can be tasted, (3) moistens food and aids in compacting it into a bolus, and (4) contains enzymes that begin the chemical breakdown of starchy foods. Three pairs of salivary glands: 1-The large parotid gland lies anterior to the ear between the masseter muscle and the skin. The prominent parotid duct opens into the vestibule next to the second upper molar. Branches of the facial nerve run through the parotid gland on their way to the muscles of facial expression. For this reason, surgery on this gland can result in facial paralysis. • HOMEOSTATIC IMBALANCE Mumps, a common children’s disease, is an inflammation of the parotid glands caused by the mumps virus (myxovirus), which spreads from person to person in saliva. People with mumps complain of pain when they open their mouth or chew. Mumps in adult males carry a 25% risk that the testes may become infected as well, leading to sterility. 2- the submandibular gland lies along the medial aspect of the mandibular body. 3- The small sublingual gland lies anterior to the submandibular gland under the tongue and opens via 10–12 ducts into the floor of the mouth. To a greater or lesser degree, the salivary glands are composed of two types of secretory cells: mucous and serous. Serous cells produce a watery secretion containing enzymes and ions, whereas the mucous cells produce mucus. • Composition of Saliva Saliva is largely water—97 to 99.5%.. As a rule, saliva is slightly acidic (pH 6.75 to 7.00), but its pH may vary. Its solutes include electrolytes (Na+, K+, Cl–, PO4–, and HCO3–); the digestive enzyme salivary amylase; the proteins mucin (mu′sin), lysozyme, and IgA; and metabolic wastes (urea and uric acid). When dissolved in water, the glycoprotein mucin forms thick mucus that lubricates the oral cavity and hydrates foodstuffs. The Pancreas The pancreas is a soft, gland that extends across the abdomen from its tail (abutting the spleen) to its head, which is encircled by the C-shaped duodenum . Most of the pancreas is retroperitoneal and lies deep to the greater curvature of the stomach. • It produces enzymes that break down all categories of foodstuffs. This exocrine product, called pancreatic juice, drains from the pancreas via the centrally located main pancreatic duct. The pancreatic duct generally fuses with the bile duct just as it enters the duodenum (at the hepatopancreatic ampulla). A smaller accessory pancreatic duct empties directly into the duodenum just proximal to the main duct. • Pancreatic islets (islets of Langerhans) are mini-endocrine glands release insulin and glucagon, hormones that play an important role in carbohydrate metabolism, as well as several other hormones . • Composition of Pancreatic Juice Approximately 1200 to 1500 ml is produced daily. It consists mainly of water, and contains enzymes and electrolytes (primarily bicarbonate ions). The high pH (about pH 8)of pancreatic fluid helps neutralize acid chyme entering the duodenum and provides the optimal environment for activity of intestinal and pancreatic enzymes. Like pepsin of the stomach, pancreatic proteases (proteindigesting enzymes) are produced and released in inactive forms, which are activated in the duodenum, where they do their work. This prevents the pancreas from self-digestion. For example, within the duodenum, trypsinogen is activated to trypsin. Trypsin, in turn, activates two other pancreatic proteases (procarboxypeptidase and chymotrypsinogen) to their active forms, carboxypeptidase (kar-bok″se-pep′tĭ-dās) and chymotrypsin (ky″mo-trip′sin), respectively .Other pancreatic enzymes—amylase, lipases, and nucleases—are secreted in active form. The Liver and Gallbladder The liver and gallbladder are accessory organs associated with the small intestine. The liver, one of the body’s most important organs, has many metabolic and regulatory roles. However, its digestive function is to produce bile for export to the duodenum. Bile is a fat emulsifier; that is, it breaks up fats into tiny particles so that they are more accessible to digestive enzymes. The gallbladder is chiefly a storage organ for bile. • Gross Anatomy of the Liver The liver is the largest gland in the body, weighing about 1.4 kg (3 lb) in the average adult ,it occupies most of the right hypochondriac and epigastric regions, extending farther to the right of the body midline than to the left. Located under the diaphragm, the liver lies almost entirely within the rib cage, which provides some protection . Typically, the liver is said to have four primary lobes. The largest of these, the right lobe, is visible on all liver surfaces and separated from the smaller left lobe by a deep fissure .A mesentery, the falciform ligament, separates the right and left lobes anteriorly and suspends the liver from the diaphragm and anterior abdominal wall . • Bile leaves the liver through several bile ducts that ultimately fuse to form the large common hepatic duct, which travels downward toward the duodenum. Along its course, that duct fuses with the cystic duct draining the gallbladder to form the bile duct . • Composition of Bile Bile is a yellow-green, alkaline solution containing bile salts, bile pigments, cholesterol, triglycerides, phospholipids (lecithin and others), and a variety of electrolytes. Of these, only bile salts and phospholipids aid the digestive process. Bile salts are cholesterol derivatives. Their role is to emulsify fats .As a result, large fat globules entering the small intestine are physically separated into millions of small, more accessible fatty droplets that provide large surface areas for the fat-digesting enzymes to work on. • Bile salts also facilitate fat and cholesterol absorption .Although many substances secreted in bile leave the body in feces, bile salts are not among them. Instead, bile salts are conserved by means of a recycling mechanism called the enterohepatic circulation. In this process, bile salts are (1) reabsorbed into the blood by the ileum, (2) returned to the liver via the hepatic portal blood, and then (3) resecreted in newly formed bile. • The chief bile pigment is bilirubin (bil″ĭ-roo′bin), a waste product of the heme of hemoglobin formed during the breakdown of worn-out erythrocytes The globin and iron parts of hemoglobin are saved and recycled, but bilirubin is absorbed from the blood by the liver cells, excreted into bile, and metabolized in the small intestine by resident bacteria. One of its breakdown products, stercobilin (ster′ko-bi″lin), gives feces a brown color. In the absence of bile, feces are gray-white in color and have fatty streaks (because essentially no fats are digested or absorbed). • The liver produces 500 to 1000 ml of bile daily, and production is stepped up when the GI tract contains fatty chyme . • The gallbladder is a thin-walled green muscular sac about 10 cm (4 inches) long in a shallow fossa on the ventral surface of the liver .Its rounded fundus protrudes from the inferior margin of the liver. The gallbladder stores bile and concentrates it by absorbing some of its water and ions. (In some cases, bile released from the gallbladder is ten times as concentrated as that entering it.) When empty, or when storing only small amounts of bile, its mucosa is thrown into folds like the rugae of the stomach, allow the organ to expand as it fills. When its muscular wall contracts, bile is expelled into its duct, the cystic duct, and then flows into the bile duct. • HOMEOSTATIC IMBALANCE Bile is the major vehicle for cholesterol excretion, and bile salts keep the cholesterol dissolved within bile. Too much cholesterol or too few bile salts leads to cholesterol crystallization, forming gallstones, or biliary calculi which obstruct the flow of bile. Then, when the gallbladder or its duct contracts, the sharp crystals cause agonizing pain that radiates to the right thoracic region. When the gallbladder is removed, the bile duct enlarges to assume the bile-storing role. Bile duct blockage prevents both bile salts and bile pigments from entering the intestine. As a result, yellow bile pigments accumulate in blood and eventually are deposited in the skin, causing it to become yellow, or jaundiced. Jaundice caused by blocked ducts is called obstructive jaundice . Digestive Processes The processing of food by the digestive system involves six essential activities: 1. Ingestion is simply taking food into the digestive tract, usually via the mouth. 2. Propulsion, which moves food through the alimentary canal, includes : -swallowing, which is initiated voluntarily, and - peristalsis (per″ĭ -stal’sis), an involuntary process. the major means of propulsion, involves alternate waves of contraction and relaxation of muscles in the organ walls .Its main effect is to squeeze food along the tract, but some mixing occurs as well. In fact, peristaltic waves are so powerful that, once swallowed, food and fluids will reach your stomach even if you stand on your head. 3. Mechanical digestion Mechanical processes include chewing, mixing of food with saliva by the tongue, churning food in the stomach, and segmentation, or rhythmic local constrictions of the intestine Segmentation mixes food with digestive juices. 4. Chemical digestion is a series of steps in which complex food molecules are broken down to their chemical building blocks by enzymes secreted into the lumen of the alimentary canal. Chemical digestion of foodstuffs begins in the mouth and is essentially complete in the small intestine. 5. Absorption is the passage of digested end products (plus vitamins, minerals, and water) from the lumen of the GI tract through the mucosal cells by active or passive transport into the blood or lymph. The small intestine is the major absorptive site. 6. Defecation eliminates indigestible substances from the body via the anus in the form of feces. • Digestive Processes Occurring in the Mouth, Pharynx, and Esophagus -The mouth (1) ingests, (2) begins mechanical digestion by chewing, and (3) initiates propulsion by swallowing. Salivary amylase, the main enzyme in saliva, starts the chemical breakdown of polysaccharides (starch and glycogen) into smaller fragments of linked glucose molecules. (If you chew a piece of bread for a few minutes, it will begin to taste sweet as sugars are released.) Except for a few drugs that are absorbed through the oral mucosa (for example, nitroglycerine), essentially no absorption occurs in the mouth. The pharynx and esophagus single digestive function is food propulsion, accomplished by the role they play in swallowing. • Mastication (Chewing) As food enters the mouth, its mechanical breakdown begins with mastication, or chewing. The cheeks and closed lips hold food between the teeth, the tongue mixes food with saliva to soften it, and the teeth cut and grind solid foods into smaller morsels. Mastication is partly voluntary and partly reflexive. We voluntarily put food into our mouths and contract the muscles that close our jaws. • Deglutition (Swallowing) To send food on its way from the mouth, it is first compacted by the tongue into a bolus and then swallowed. Deglutition (deg″loo-tish′un), or swallowing, is a complicated process that involves coordinated activity of over 22 separate muscle groups. It has two major phases, the buccal and the pharyngeal-esophageal phases. -The buccal phase occurs in the mouth and is voluntary. In the buccal phase, we place the tip of the tongue against the hard palate, and then contract the tongue to force the bolus into the oropharynx . Once food enters the pharynx, respiration is momentarily inhibited and all routes except the desired one—into the digestive tract— are blocked off: -The tongue blocks off the mouth. -The soft palate rises to close off the nasopharynx. -The larynx rises so that the epiglottis covers its The upper esophageal sphincter relaxes. HOMEOSTATIC IMBALANCE Vomiting, or emesis, is caused by extreme stretching of the stomach or intestine or the presence of irritants such as bacterial toxins, excessive alcohol, spicy foods, and certain drugs in those organs. The diaphragm and abdominal wall muscles contract,, the cardiac sphincter relaxes, and the soft palate rises to close off the nasal passages. As a result, the stomach (and perhaps duodenal) contents are forced upward through the esophagus and pharynx and out the mouth. Before vomiting, an individual typically is pale, feels nauseated, and salivates. Excessive vomiting can cause dehydration and may lead to severe disturbances in the electrolyte and acid-base balance of the body. HOMEOSTATIC IMBALANCE Watery stools, or diarrhea, result from any condition that rushes food residue through the large intestine before that organ has had sufficient time to absorb the remaining water. Prolonged diarrhea may result in dehydration and electrolyte imbalance (acidosis and loss of potassium). Conversely, when food remains in the colon for extended periods, too much water is absorbed and the stool becomes hard and difficult to pass. This condition, called constipation, may result from lack of fiber in the diet, improper bowel habits ,lack of exercise, emotional upset, or laxative abuse. Defecation The rectum is usually empty, but when feces are forced into it by mass movements, stretching of the rectal wall initiates the defecation reflex .This is a spinal cord– mediated parasympathetic reflex that causes the sigmoid colon and the rectum to contract, the internal anal sphincter to relax. As feces are forced into the anal canal, messages reach the brain allowing us to decide whether the external (voluntary) anal sphincter should be opened or remain constricted to stop feces passage temporarily. If defecation is delayed, the reflex contractions end within a few seconds, and the rectal walls relax. With the next mass movement, the defecation reflex is initiated again—and so on, until one chooses to defecate or the urge to defecate becomes unavoidable. METABOLISM The term metabolism encompasses all of the reactions that take place in the body. Everything that happens within us is part of our metabolism. The reactions of metabolism may be divided into two major categories: anabolism and catabolism. Anabolism means synthesis or “formation” reactions, the bonding together of smaller molecules to form larger ones. Synthesis of hemoglobin by cells of the red bone marrow, synthesis of glycogen by liver cells, and synthesis of fat to be stored in adipose tissue are all examples of anabolism. Such reactions require energy, usually in the form of ATP. Catabolism means decomposition, the breaking of bonds of larger molecules to form smaller molecules. Cell respiration is a series of catabolic reactions that down food molecules to carbon dioxide and water. During catabolism, energy is often released and used to synthesize ATP .The ATP formed during catabolism is then used for energy-requiring anabolic reactions. Most of our anabolic and catabolic reactions are catalyzed by enzymes. Enzymes are proteins that enable reactions to take place rapidly at body temperature. The body has thousands of enzymes, and each is specific, that is, will catalyze only one type of reaction. • Carbohydrate Metabolism Because all food carbohydrates are eventually transformed to glucose, the story of carbohydrate metabolism is really a tale of glucose metabolism. Glucose enters the tissue cells by facilitated diffusion, a process that is greatly enhanced by insulin. Immediately upon entry into the cell, glucose is phosphorylated to glucose-6-phosphate by transfer of a phosphate group to its sixth carbon during a coupled reaction with ATP: Glucose + ATP→ glucose-6-PO4 + ADP • Most body cells lack the enzymes needed to reverse this reaction, so it effectively traps glucose inside the cells. Because glucose-6-phosphate is a different molecule from simple glucose, the reaction also keeps intracellular glucose levels low, maintaining a concentration gradient for glucose entry. The catabolic and anabolic pathways for carbohydrates all begin with glucose-6-phosphate. Glucose is the raw material for the synthesis of another important monosaccharide, the pentose Sugars that are part of nucleic acids. Deoxyribose is the five-carbon sugar found in DNA, and ribose is found in RNA. This function of glucose is very important, for without the pentose sugars our cells could neither produce new chromosomes for cell division nor carry out the process of protein synthesis. Any glucose in excess of immediate energy needs or the need for pentose sugars is converted to glycogen in the liver and skeletal muscles. Glycogen is then an energy source during states of hypoglycemia or during exercise. If still more glucose is present, it will be changed to fat and stored in adipose tissue(lipogenesis). • Gluconeogenesis is the formation of glucose from noncarbohydrate (fat or protein) molecules. It occurs in the liver when blood glucose levels begin to fall. CELL RESPIRATION ,the breakdown of food molecules to release their potential energy d synthesize ATP the summary reaction of cell respiration is: C6H12O6(glucose) + O2 → CO2 + H2O + ATP + Heat, the purpose of which is to produce ATP. Glucose contains potential energy, and when it is broken down to CO2 and H2O, this energy is released in the forms of ATP and heat. The oxygen that is required comes from breathing, and the CO2 formed is circulated to the lungs to be exhaled. The water formed is called metabolic water, and helps to meet our daily need for water. Energy in the form of heat gives us a body temperature, and the ATP formed is used for energyrequiring reactions. Cell respiration of glucose involves three major stages: glycolysis, the Krebs citric acid cycle, and the cytochrome (or electron) transport system. • Glycolysis A series of ten chemical steps by which glucose is converted to two pyruvic acid molecules. All steps except the first, during which glucose entering the cell is phosphorylated to glucose-6-phosphate, are fully reversible. The enzymes for the reactions of glycolysis are found in the cytoplasm of cells, and oxygen is not required (glycolysis is an anaerobic process). In glycolysis, a sixcarbon glucose molecule is broken down to two threecarbon molecules of pyruvic acid. As a result of these reactions, a net gain of two ATP molecules per glucose molecule is obtained. If no oxygen is present in the cell, as may happen in muscle cells during exercise, pyruvic acid is converted to lactic acid, which causes muscle fatigue. If oxygen is present, however, pyruvic acid continues into the next stage, the Krebs citric acid cycle (or, more simply, the Krebs cycle). • Krebs Citric Acid Cycle The enzymes for the Krebs cycle (or citric acid cycle) are located in the mitochondria of cells. This second stage of cell respiration is aerobic, meaning that oxygen is required. The Krebs cycle is fueled by pyruvic acid (and fatty acids). To enter the cycle, pyruvic acid is converted to acetyl CoA. The acetyl CoA is then oxidized and decarboxylated. Complete oxidation of two pyruvic acid molecules yields a net gain of 2 ATP . To enter the cycle, pyruvic acid is converted to acetyl CoA. The acetyl CoA is then oxidized and decarboxylated. Complete oxidation of two pyruvic acid molecules yields 6 CO2, 8 NADH + H+, 2 FADH2, and a net gain of 2 ATP. Much of the energy originally present in the bonds of pyruvic acid is now present in the reduced coenzymes. • In the electron transport chain, reduced coenzymes are oxidized by delivering hydrogen to a series of oxidation-reduction acceptors; and electrons are combined with oxygen to form water . • For each glucose molecule oxidized to carbon dioxide and water, there is a net gain of 38 ATP. Proteins Metabolism Animal products provide highquality complete protein containing all (10) essential amino acids. Most plant products lack one or more of the essential amino acids. Amino acids are the structural building blocks of the body and of important regulatory molecules. Protein synthesis can and will occur if all essential amino acids are present and sufficient carbohydrate (or fat) calories are available to produce ATP. Otherwise, amino acids will be burned for energy. Nitrogen balance occurs when protein synthesis equals protein loss. A dietary intake of 0.8 g of protein per kg of body weight is recommended for most healthy adults. Amino Acids The primary uses for amino acids are the synthesis of the non-essential amino acids by the liver and the synthesis of new proteins in all tissues. By way of review, we can mention some proteins with which you are already familiar: keratin and melanin in the epidermis; collagen in the dermis,tendons, and ligaments; myosin, actin, and myoglobin in muscle cells; hemoglobin in RBCs; antibodies produced by WBCs; prothrombin and fibrinogen for clotting; albumin to maintain blood volume; pepsin and amylase for digestion; growth hormone and insulin; and the thousands of enzymes needed to catalyze reactions within the body. -Only when the body’s needs for new proteins have been met are amino acids used for energy production. - Excess amino acids; they will be deaminated and converted to simple carbohydrates and contribute to glycogen storage or they may be changed to fat and stored in adipose tissue. -Amine groups removed during deamination (as ammonia) are combined with carbon dioxide by the liver to form urea. Urea is excreted in urine. -Protein synthesis requires the presence of all ten essential amino acids. If any are lacking, amino acids are used as energy fuels. Lipids Metabolism Most dietary lipids are triglycerides. The primary sources of saturated fats are animal products while unsaturated fats are present in plant products, nuts, and fish. -The major sources of cholesterol are egg yolk, meats, and milk products . Linoleic and linolenic acids are essential fatty acids. -Triglycerides provide reserve energy, cushion body organs, and insulate the body. -Phospholipids are used to synthesize plasma membranes and myelin. -Cholesterol is used in plasma membranes and is the structural basis of vitamin D, steroid hormones, and bile salts. -Fat intake should represent 35% or less of caloric intake. The liver makes a basal amount of cholesterol (85%) even when dietary cholesterol intake is excessive. Fatty Acids and Glycerol The end products of fat digestion that are not needed immediately for energy production but may be stored as fat (triglycerides) in adipose tissue. Most adipose tissue is found subcutaneously and is potential energy for times when food intake decreases. Fatty acids and glycerol are also used for the synthesis of phospholipids, which are essential components of all cell membranes. Myelin, for example, is a phospholipid of the membranes of Schwann cells, which form the myelin sheath of peripheral neurons. The liver can synthesize most of the fatty acids needed by the body. Two exceptions are linoleic acid and linolenic acid, which are essential fatty acids and must be obtained from the diet. Linoleic acid is part of lecithin, which in turn is part of all cell membranes. When fatty acids are broken down in the process of beta-oxidation, the resulting acetyl groups may also be used for the synthesis of cholesterol. This takes place primarily in the liver, although all cells are capable of synthesizing cholesterol for their cell membranes. The liver uses cholesterol to synthesize bile salts for the emulsification of fats in digestion. The steroid hormones(Adrenal cortex and sex hormones) are also synthesized from cholesterol. • Cholesterol Metabolism and Regulation of Blood Cholesterol Levels Cholesterol, though an important dietary lipid, it is not used as an energy source. It serves instead as the structural basis of bile salts, steroid hormones, and vitamin D and as a major component of plasma membranes. About 15% of blood cholesterol comes from the diet. The other 85% is made from acetyl CoA by the liver. • Cholesterol is lost from the body when it is catabolized and secreted in bile salts, which are eventually excreted in feces. • Cholesterol Transport Because triglycerides and cholesterol are insoluble in water, they are transported to and from tissue cells bound to small lipid-protein complexes, formed by the liver, called lipoproteins. Lipoproteins vary considerably in their relative fatprotein composition, but they all contain triglycerides, phospholipids, and cholesterol in addition to protein . In general, the higher the percentage of lipid in the lipoprotein, the lower its density; and the greater the proportion of protein, the higher its density. On this basis, there are high-density lipoproteins (HDLs), low-density lipoproteins (LDLs), and very low density lipoproteins (VLDLs). • The Metabolic Role of the Liver 1-The liver is the body’s main metabolic organ and it plays a crucial role in processing (or storing) virtually every nutrient group. 2-It helps maintain blood energy sources, metabolizes hormones, and detoxifies drugs and other substances. 3-The liver synthesizes cholesterol, catabolizes cholesterol and secretes it in the form of bile salts, and makes lipoproteins. LDLs transport triglycerides and cholesterol from the liver to the tissues, whereas HDLs transport cholesterol from the tissues to the liver (for catabolism and elimination). Excessively high LDL levels are implicated in atherosclerosis, cardiovascular disease, and strokes. METABOLIC RATE Although the term metabolism is used to describe all of the chemical reactions that take place within the body, metabolic rate is usually expressed as an amount of heat production. This is because many body processes that utilize ATP also produce heat. These processes include the contraction of skeletal muscle, the pumping of the heart, and the normal breakdown of cellular components. Therefore, it is possible to quantify heat production as a measure of metabolic activity. During sleep, for example, energy expended by a 150-pound person is about 60 to 70 kcal per hour. Getting up and preparing breakfast increases energy expenditure to 80 to 90 kcal per hour. For mothers with several small children, this value may be significantly higher. Clearly, greater activity results in greater energy expenditure. The energy required for merely living (lying quietly in bed) is the basal metabolic rate (BMR). A number of factors affect the metabolic rate: 1- Age—metabolic rate is highest in young children and decreases with age. 2-Body configuration—more surface area proportional to weight (tall and thin) means a higher metabolic rate. 3. Sex hormones—men usually have a higher metabolic rate than do women; men have more muscle proportional to fat than do women. 4. Sympathetic stimulation—metabolic activity increases in stress situations. 5. Decreased food intake—metabolic rate decreases to conserve available energy sources. 6. Climate—people who live in cold climates usually have higher metabolic rates because of a greater need for heat production. 7. Exercise—Contraction of skeletal muscle increases energy expenditure and raises metabolic rate . To estimate your own basal metabolic rate (BMR), calculate kilocalories (kcal) used per hour as follows: For women: use the factor of 0.9 kcal / kg/hour. For men: use the factor of 1.0 kcal / kg /hour Then multiply kcal/hour by 24 hours to determine kcal per day. Example: A 120-pound woman: 1. Change pounds to kilograms: 120 lb at 2.2 lb/kg = 55 kg 2. Multiply kg weight by the BMR factor: 55 kg x 0.9 kcal/kg/hr = 49.5 kcal/hr 3. Multiply kcal/hr by 24: 49.5 kcal/hr x 24 = 1188 kcal/day (An approximate BMR, about 1200 kcal/day) Example: A 160-pound man: 1. 160 lb at 2.2 lb/kg = 73 kg 2. 73 kg x 1.0 kcal/kg/hr = 73 kcal/hr 3. 73 kcal/hr x 24 = 1752 kcal/day To approximate the amount of energy actually expended(Total Metabolic Rate,TMR) during an average day (24 hours), the following percentages may be used: -Sedentary activity: add 40% to 50% of the BMR to the BMR -Light activity: add 50% to 65% of the BMR to the BMR -Moderate activity: add 65% to 75% of the BMR to the BMR -Strenuous activity: add 75% to 100% of the BMR to the BMR Using our example of the 120-pound woman with a BMR of 1200 kcal/day: Sedentary: 1680 to 1800 kcal/day Light: 1800 to 1980 kcal/day Moderate: 1980 to 2100 kcal/day Strenuous: 2100 to 2400 kcal/day Proteins and Fats—as energy sources 1. Excess amino acids are deaminated in the liver and converted to pyruvic acid or acetyl groups to enter the Krebs cycle. Amino acids may also be converted to glucose to supply the brain . 2. Glycerol is converted to pyruvic acid to enter the Krebs cycle. 3. Fatty acids, in the process of beta-oxidation in the liver, are split into acetyl groups to enter the Krebs cycle; ketones are formed for transport to other cells. Energy Available from Food 1. Energy is measured in kilocalories (Calories)kcal. 2. There are 4 kcal per gram of carbohydrate, 4 kcal per gram of protein, 9 kcal per gram of fat. With reference to food,kilocalories may be called calories. Synthesis Uses of Foods 1. Glucose—used to synthesize the pentose sugars for DNA and RNA; used to synthesize glycogen to store energy in liver and muscles. 2. Amino acids—used to synthesize new proteins and the non-essential amino acids; essential amino acids must be obtained in the diet. 3. Fatty acids and glycerol—used to synthesize phospholipids for cell membranes, triglycerides for fat storage in adipose tissue, and cholesterol and other steroids; essential fatty acids must be obtained in the diet. 4. Any food eaten in excess will be changed to fat and stored. Body Temperature - Normal range is 36° to 38°C with an average of 37°C. - Temperature regulation in infants and the elderly is not as precise as it is at other ages. Heat Production Heat is one of the energy products of cell respiration. Many factors affect the total heat actually produced: 1. Thyroxine from the thyroid gland—the most important regulator of daily heat production. As metabolic rate decreases, more thyroxine is secreted to increase the rate of cell respiration. 2. Stress—sympathetic impulses and epinephrine and norepinephrine increase the metabolic activity of many organs, increasing the production of ATP and heat. 3. Active organs continuously produce heat. Skeletal muscle tone produces 25% of the total body heat at rest. The liver provides up to 20% of the resting body heat. 4. Food intake increases the activity of the digestive organs and increases heat production. 5. Changes in body temperature affect metabolic rate. A fever increases the metabolic rate, and more heat is produced. Heat Loss 1. Most heat is lost through the skin. 2. Blood flow through the dermis determines the amount of heat that is lost by radiation, conduction, and convection. 3. Vasodilation in the dermis increases blood flow and heat loss; radiation and conduction are effective only if the environment is cooler than the body. 4. Vasoconstriction in the dermis decreases blood flow and conserves heat in the core of the body. 5. Sweating is a very effective heat loss mechanism; excess body heat evaporates sweat on the skin surface; sweating is most effective when the atmospheric humidity is low. Sweating also has a disadvantage in that water is lost and must be replaced to prevent serious dehydration. 6. Heat is lost from the respiratory tract by the evaporation of water from the warm respiratory mucosa; water vapor is part of exhaled air. 7. A very small amount of heat is lost as urine and feces are excreted at body temperature. Regulation of Heat Loss 1. The hypothalamus is the thermostat of the body and regulates body temperature by balancing heat production and heat loss.It receives information from its own neurons and from the temperature receptors in the dermis. Fever—is controlled hyperthermia. Most often, it results from infection somewhere in the body, but it may be caused by cancer or allergic reactions. 1. Pyrogens are substances that cause a fever: bacteria, foreign proteins, or chemicals released during inflammation (endogenous pyrogens). 2. Pyrogens raise the setting of the hypothalamic thermostat; the person feels cold and begins to shiver to produce heat. 3. When the pyrogen has been eliminated, the hypothalamic setting returns to normal; the person feels warm, and sweating begins to lose heat to lower the body temperature. -A low fever may be beneficial because it increases the activity of WBCs and inhibits the activity of some pathogens. -A high fever may be detrimental because enzymes are denatured at high temperatures. This is most critical in the brain, where cells that die cannot be replaced. Heat-Promoting Mechanisms When the external temperature is low or blood temperature falls for any reason, the heat-promoting center is activated and triggers one or more of the following mechanisms : 1-Constriction of cutaneous blood vessels. As a result, blood is restricted to deep body areas and largely bypasses the skin. Because the skin is separated from deeper organs by a layer of insulating subcutaneous (fatty) tissue, heat loss from the shell is dramatically reduced. HOMEOSTATIC IMBALANCE Restricting blood flow to the skin is not a problem for a brief period, but if it is extended (as during prolonged exposure to very cold weather), skin cells deprived of oxygen and nutrients begin to die. This extremely serious condition is called frostbite. 2. Shivering. is involuntary shuddering contractions. Shivering is very effective in increasing body temperature because muscle activity produces large amounts of heat. 3. Increase in metabolic rate. Cold stimulates the release of epinephrine and norepinephrine by the adrenal medulla in reponse to sympathetic nerve stimuli, which elevates the metabolic rate and enhances heat production. 4. Enhanced thyroxine release. Because thyroid hormone increases metabolic rate, body heat production increases. Beside these involuntary adjustments, we humans make a number of behavioral modifications to prevent overcooling of our body core: -Putting on more or warmer clothing to restrict heat loss (a hat, gloves, and “insulated” outer garments) -Drinking hot fluids -Changing posture to reduce exposed body surface area (clasping the arms across the chest). -Increasing physical activity to generate more heat (jumping up and down, clapping the hands) • Heat-Loss Mechanisms Heat-loss mechanisms protect the body from excessively high temperatures. Most heat loss occurs through the skin via radiation, conduction, convection, and evaporation. Heat-loss mechanisms include one or both of the following : 1. Dilation of cutaneous blood vessels. As the blood vessels swell with warm blood, heat is lost from the shell by radiation, conduction, and convection. 2. Enhanced sweating. The sweat glands are strongly activated. Evaporation of perspiration is an efficient means of ridding the body of heat as long as the air is dry. However, when the relative humidity is high, evaporation occurs much more slowly. In such cases, the heat-liberating mechanisms cannot work well, and we feel miserable and irritable. Behavioral or voluntary measures commonly taken to reduce body heat include : • Reducing activity (“laying low”) • Seeking a cooler environment (a shady spot) or using a device to increase convection (a fan) or cooling (an air conditioner) • Wearing light-colored, loose clothing that reflects radiant energy. (This is actually cooler than being nude because bare skin absorbs most of the radiant energy striking it.) • HOMEOSTATIC IMBALANCE Under conditions of overexposure to a hot and humid environment, normal heat-loss processes become ineffective. The hyperthermia (elevated body temperature) that ensues depresses the hypothalamus. Increasing temperatures increase the metabolic rate, which increases heat production. The skin becomes hot and dry and, as the temperature continues to spiral upward, multiple organ damage becomes a distinct possibility, including brain damage. This condition, called heat stroke, can be fatal unless corrective measures are initiated immediately (immersing the body in cool water and administering fluids). • Hypothermia (hi″po-ther′me-ah) is low body temperature resulting from prolonged uncontrolled exposure to cold. Vital signs (respiratory rate, blood pressure, and heart rate) decrease as cellular enzymes become sluggish. Drowsiness sets in and, oddly, the person becomes comfortable even though previously he or she felt extremely cold. Shivering stops at a core temperature of 30–32°C (87–90°F) when the body has exhausted its heatgenerating capabilities. Uncorrected, the situation progresses to coma and finally death (by cardiac arrest), when body temperatures approach 21°C (70°F). Developmental Aspects of the Digestive System 1. The glandular accessory organs (salivary glands, liver, pancreas, and gallbladder) form from outpocketings of the foregut endoderm. The mucosa of the alimentary canal develops from the endoderm, which folds to form a tube. The remaining three tunics of the alimentary canal wall are formed by mesoderm. 2. Important congenital abnormalities of the digestive tract include cleft palate/lip, tracheoesophageal fistula, and cystic fibrosis. All interfere with normal nutrition. • 3. Various inflammations affect the digestive system throughout life. Appendicitis is common in adolescents, gastroenteritis and food poisoning can occur at any time (given the proper irritating factors), ulcers and gallbladder problems increase in middle age. 4. The efficiency of all digestive system processes declines in the elderly, and periodontal disease is common. Diverticulosis, fecal incontinence, and GI tract cancers such as stomach and colon cancer appear with increasing frequency in an aging population.