Schizophrenia
advertisement

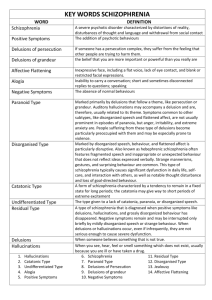
Schizophrenia Elisa A. Mancuso RNC, MS, FNS Professor 2 million people (1.5 % of Population) Costs $ 35 billion Onset late adolescence or early adulthood – Men 15-25 women 20-35 & > 50 Psychotic disorders with disturbances in: – Thought processes – Perceptions – Expression of feelings Indicators Psychotic Symptoms – Preoccupied with own thoughts and feelings Deterioration in functioning – Role, ADLs, Interpersonal relationships 6 month duration of symptoms Bleuler’s 4 As – Autism – Affect – Associative Looseness – Ambivilance Etiology Genetic – Abnormal marker gene on chromosome # 5 – Heredity determines one’s predisposition Both parents schizophrenic = 20-50 % ↑↑ risk Identical twins = 50-75 % ↑↑ risk for sibling Biochemical – – – – – – – Altered Neuroanatomy ▲s in cortex ↑↑ DA activity (2x DA receptors) = Psychosis ↓ AcH = ↑ Confusion, ↓ NE = Anhedonia ↓ 5-HT = ↓ Aggressive tendencies ↓Glutamate = learning & memory ↓Glucose metabolism & ↓ GABA Psychological Poor early mother-child relationship – “Trust vs Mistrust” ↓ Ego boundaries Dysfuntional family system Double-bind communication – Say one thing but mean the opposite Environment – ↓ Socioeconomic = ↑ stress & ↓ ↓ resources – Stressful life events precipitate onset! Schizophrenia Stages Stage I Schizoid Personality Isolate themselves, “loners” Indifferent, cold, aloof ↓ Range of emotional expression Don’t enjoy close relationships Stage II Prodromal “Pre-Schizophrenic” Socially withdrawn- Blunted affect Eccentric behavior & Bizarre ideas Unusual perceptual experiences ↓ Role performance ↓ADLs Schizophrenia Stages Stage III Schizophrenia (Active) Prominent psychotic symptoms >6 months Delusions False, fixed belief Grandiose, Persecutory, Paranoia, Religiosity Hallucinations False sensory perception Ideas of Reference Disorganized Behavior Impaired work, social relations & self care Disorganized Speech Associative Looseness Clanging Echolalia Word Salad Poverty of Speech Neologisms Schizophrenia Stages Stage III Secondary Symptoms – Anxiety Substance Abuse (ETOH, coke) – Depression > 25% – ↑↑ Suicide (10%) = Leading cause of death – Compulsive H2O drinking 4-10 L/day H2O intoxication ↓ Na = Lightheaded N&V Confusion Coma Lethargy Muscle cramps Schizophrenia Stages Stage IV Residual – Periods of remissions & exacerbations – Similar to Prodromal phase – Social withdrawal – Flat affect – Impaired Role Performance Schizophrenia Types Disorganized (Hebephrenic) – Onset before age 25 – Chronic flat, inappropriate affect – Silliness, giggling, masturbating in public – Bizarre behavior Facial grimacing & mannerisms – Impaired social interaction – ↓ Contact with reality – Incoherent speech & concrete thinking Schizophrenia Types Catatonic Least common Sudden onset & good prognosis Catatonic Excitement Extreme psychomotor agitation Purposeless movements – Echopraxia – ↑ risk of injury to self/others Continuous incoherent shouting - Echolalia Catatonic Stupor Extreme psychomotor retardation Mute & Waxy Flexibility (Bizarre posturing) Schizophrenia Types Paranoid – Preoccupied - 1 or more delusions Persecution or Grandeur – Related auditory hallucinations – Argumentative – Hostile – Aggressive – Tense – Suspicious – Hypervigilent Schizophrenia Types Undifferentiated Chronic – Disorganized-bizarre behavior – Usually docile and not aggressive – Does not meet criteria of other subtypes – Delusions & Hallucinations are prominent Schizophrenia Types Residual (Pseudo-neurotic) – Follows an acute episode – Absence of prominent symptoms No delusions or hallucinations – Social isolation – Poor Grooming – Eccentric behavior – Emotional Blunting Schizophrenia Types Schizoaffective Disorder – 2 week period of predominant psychotic episode (↑ incidence in women) Delusions Hallucinations Disorganized behavior ↑ Sexuality Racing thoughts – Mood Disorder (affective) behaviors Mania – Euphoria – Grandiosity & Hyperactivity Depression – – Psychomotor retardation & suicidal ideation – ↓↓ Occupational & social functioning Characteristics Positive – Excess or distorted inappropriate behaviors – Disorganized thinking – Not seen in mentally healthy adults! Negative – Loss or decrease of appropriate function – Diminished emotional expression Anhedonia Apathy Poverty of thoughts Charcteristics Positive Delusions Hallucinations Catatonic Excitement Echopraxia Echolalia Neologisms Associative Looseness Religiosity Paranoia Negative Concrete thinking Symbolism Catatonic Stupor Social withdrawal Poverty of speech Flat affect Anhedonia Depersonalization Assessment Mental Status Exam (Provides baseline data) – Appearance & General Health Dress Eye Contact Grooming Motor Behavior Facial Expression Posture – Speech Pace Tone & Modulation Spontaneity Clarity Volume Interruptions – Level of Consciousness General Responsiveness Sensorium – Emotional State Mood Affect Intensity Appropriateness – Cognitive Function Thought Process Concentration Content Abstract Thinking Perceptions Insight/Judgment Nursing Interventions Primary Goal = Patient Safety Establish trust & listen closely – Accepting attitude & Keep promises Calm approach & non-threatening environment – Prevent violence & ↓ Anxiety Clarify & reinforce reality – Orient to here & now Address physical needs ↑ Self esteem Psychotic Symptom Interventions Delusions Accept experience, identify content & triggers Encourage reality oriented conversation Use distraction & refocus Role model coping techniques to ↓ anxiety Hallucinations Focus on the behavioral cue (laughing, talking, turning head) Have Pt describe what is happening Identify environmental & emotional triggers To prevent aggressive responses Avoid touching without 1st warning Psychotic Symptom Interventions Impaired Communication Role model clear communication Use simple, concrete statements Seek clarification & validate content Vebalize the implied Paranoia ↓ Environmental stimulation Maintain eye contact Provide plenty of personal space Always announce your presence ↓ Impulsivity “Time Outs” for rest Psychotic Symptom Interventions Ritualism Initiate conversation as ritual is performed Assess for behavioral cues indicating ↑ anxiety Negotiate a schedule for ritual & ADLs Social Withdrawal Convey nonverbal acceptance & worthiness Provide brief & frequent 1:1 contacts Initiate interaction & gradually expand social contacts ↑ Social skills training Rules & expectations Cognitive Therapy ↑ Decision making Regression RN approaches Pt. ↑ Self-Esteem and encourage independent behavior Antipsychotic (Neuroleptic) Meds Major Tranquilizers ↑↑ Protein Binding (91-99%) ↓ Efficacy in men (1/3 relapse + 1/3 disabled) Potency – High Fluphenazine (Prolixin) [Decanoate IM q3 weeks] Haloperidol (Haldol) [Decanoate IM q4 weeks] Trifluroperazine (Stelazine) – Low Chlorpromazine (Thorazine) * 1st drug 1950 Thioridazine (Mellaril) Antipsychotic (Neuroleptic) Meds Action – ↓ Agitation ↓ Psychotic Symptoms – ↓ + Behaviors (Delusions/Hallucinations) – Block DA receptors =↓ DA Improves fine motor movement & coordination Sensory integration & emotional behavior – Anticholinergic Effects (Autonomic NS) Dry Mouth Blurred vision Constipation Sedation Urinary Retention Photophobia Orthostatic Hypotension Nasal Congestion Antipsychotic (Neuroleptic) Meds ↑↑ Prolactin Levels – Sexual/Menstrual dysfunction – ↓ Libido – Galactorrhea – Gynecomastia – ↑ weight gain Cognition – ↓ Alertness ↓ Concentration – ↓ Seizure threshold = ↑ Risk of seizures Antipsychotic (Neuroleptic) Meds ExtraPyramidal Side Effects (EPS) – ↓↓ DA ↑↑ AcH Imbalance – ↑↑ Incidence with ↑↑ potency meds Prolixin, Haldol & Stelazine – Movement disorder Dystonia Pseudoparkinsonism Akathesia Tardive Dyskinesia ExtraPyramidal Side Effects (EPS) Dystonia – Quick onset 1st few hours or days – ↑ Adolescent males < age 25 – Acute spasms of tongue, face, neck & back – Hypertonia – Laryngospasm – Respiratory distress – Oculogyric Crisis- Rolling back of eyes – Torticolis- Head twisted to 1 side – Involuntary uncoordinated movements ExtraPyramidal Side Effects (EPS) Pseudoparkinsonism – Appears within 1-5 days – ↑ women & older Pts – Drooling, Pill-Rolling of thumb & finger – Mask-like face, Stooped Posture – Action Tremors – Shuffling gait with small steps – Muscle rigidity – Bradykinesia – Cogwheeling ExtraPyramidal Side Effects (EPS) Akathesia – Appears 50-60 days – Motor restlessness “Nervous Energy” Jitteriness Tapping feet constantly Pacing Rocking back & forth Frequent position changes ExtraPyramidal Side Effects (EPS) Tardive Dyskinesia – Slow & insideous process – Irreversible after several years of meds. – Involuntary movements of Limbs, trunk & face. – Bizarre facial movements “Fly catching” with tongue Lip smacking – Difficulty swallowing – Irregular respirations Neuroleptic Malignant Syndrome NMS Rare idiosyncratic reaction 1% young men ↑ Incidence with ↑↑ potency meds & ↓↓ DA Abrupt onset & rapid progression 10% mortality rate Signs – Severe muscle rigidity Hyperreflexia (+4) – Hyperthermia > 105 Diaphoresis – Altered LOC → Stupor → Coma – ↑↑ HR ↑↑ RR – CV Collapse & Respiratory failure = Fatal! NMS Therapy Immediately D/C med Wait 2 weeks before starting new meds (Lithium) NO Haldol or Thorazine Cooling blanket O2 MSO4 (Morphine sulfate) – ↓ pain & ↓ VS Tylenol – ↓ Temp and pain Dantrolene (Dantrium) muscle relaxant & ↓ Temp Bromocriptine (Parlodel) IV Fluids Atypical Medications Relieves (+) & (-) Behaviors ↓ EPS ↓ Prolactin Clozapine (Clozaril) – Binds to 5-HT2, Alpha1,2, H1, & DA recptors – SE- National registry to monitor SEs! Agranulocytosis –WBC < 3000 or ANC < 500 = D/C med! –Mandatory weekly CBC 1st 6 months Then q other week Drowsiness ↑Salivation ↑Dizziness ↑ HR ↑Weight ↑ Risk for IDDM Prolonged QT interval Atypical Medications Risperidone (Risperdal) – ↓↓ DA ↓ 5-HT ACh & NE – Readily absorbed – Active metabolite is clinically effective – SE Sedation/Insomnia Orthostatic Hypotension ↑↑ Appetite Tardive Dyskinesia Atypical Medications Olanzapine (Zyprexia) – Antagonizes DA & 5-HT receptors – Binds to Histamine Quetiapine (Seroquel) – √ renal function – √ EKG for prolonged QT wave Ziprasidone (Geodon) – DA & 5-HT receptor antagonists – ↓ Depression & Anxiety Medication Administration Schedule – Initially take meds in divided doses 2-4x/day – Non-compliant Pts: Haldol decanoate IM q 4 weeks Prolixin decanoate IM q 3 weeks Efficacy – Takes 1- 4 weeks for significant response – Once symptoms are controlled ▲ HS ↓↓ SE Dosage – Use lowest dosage to ↓ Tardive Dyskinesia Medication Administration Antiparkinson Meds – Give to counteract SE & toxic effects – Only given with documented S/S of EPS – Restore the balance of DA & Ach ↑↑DA ↓↓ACh Amantadine (Symmetrel) Bromocriptine (Parlodel) Benzotropine (Cogentin) Trihexyphenidyl (Artane) Biperiden (Akineton) Procyclidine (Kemadrin) Patient Teaching Medication – Generic & trade name, dose, action & SE – Assess SE “How is medication working?” Interventions & when to notify RN/MD – Carry card with Med ID – NO ETOH or illegal substances – Don’t stop taking drug abruptly – Don’t ▲ position rapidly Patient Outcome Evaluation Slow progress – Services are needed long-term (decades) Set small achievable, short-term goals Assess effective coping skills Obtain Pt & family input – Pt. safety Communication skills – Social Skills Self-Esteem – Medication compliance – Support system – Living in least restrictive setting