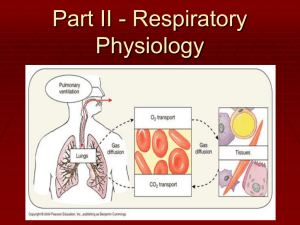
Pulmonary ventilation
advertisement

Part II - Respiratory Physiology 4 distinct events Pulmonary ventilation: air is moved in and out of the lungs External respiration: gas exchange between blood and alveoli Respiratory gas transport: CV system transports oxygen and carbon dioxide between lungs & tissues (discussed in Blood chapter) Internal respiration: gas exchange between blood & tissue cells Definition: Cellular respiration: actual use of oxygen & production of carbon dioxide in the cells (this is why we have to breathe!!) Pulmonary Ventilation External Respiration Resp. Gas Transport Internal Respiration Cellular Respiration Mechanics of Breathing Pulmonary Ventilation: Event #1 Pulmonary ventilation: - Moving air into and out of the lungs Depends on pressure changes Breathing Inspiration = moving air into the lungs Expiration = moving air out of lungs Pressure Relationships Intrapulmonary pressure Pressure within the alveoli (lungs) Changes with phases of breathing Always equalizes itself with atmospheric pressure Intrapleural pressure Pressure within intrapleural space (between the pleural membranes ) Always 4 mmHg less than intrapulmonary pressure Atalectasis Any conditions that causes intrapulmonary pressure to equal intrapleural pressure will cause the lungs to collapse This means they lose the ability to move air since there is NO more pressure difference Atelectasis term for lung collapse Pneumothorax Air in the intrapleural space due to trauma – causes lung collapse Pulmonary ventilation Question: Why does breathing happen? ONLY acceptable answer: The RULE: Volume changes lead to pressure changes which lead to the flow of gases to equalize the pressure Diaphragm Structure Boyle’s Law = Pressure & Volume have an INVERSE relationship . Pressure differences cause gas to flow from high to low When the diaphragm contracts, the muscle fibers shorten – so muscle comes down Inspiration Main inspiratory muscles Diaphragm & external intercostals Thoracic dimensions change to increase volume of thoracic cavity by 0.5 liters Intrapulmonary pressure drops 1-3 mmHg and air rushes info normal quiet inspiration A deep forced (active) inspiration requires activation of accessory muscles – see diagram in notes Expiration A passive process dependent on natural lung elasticity lungs recoil when inspiration stops – so alveoli compress –which leads to a volume decreases -causing intrapulmonary pressure to rise - gas outflows to equalize the pressure with atmospheric pressure Forced (active) expiration requires contraction of abdominals, etc – see diagram What doctors listen for Bronchial sounds: produced by air rushing through trachea & bronchi Vesicular sounds: produced by air filling alveoli Respiratory Sounds Wheezing : whistling sound Rales: rasping sound Hear the sounds Basic Lung Sounds – Bronchial Auscultating The Lungs - Reference Guide Physical factors influencing Pulmonary ventilation can be influenced by 4 physical factors Respiratory passage resistance Lung compliance Lung elasticity Alveolar surface tension forces Respiratory passage resistance Resistance due to increased friction as air moves through passages Smooth muscle bronchoconstriction Disorders such as asthma – when bronchi constrict Local accumulations of mucus, infectious material, and tumors – also block air passage Asthma Lung compliance The ease with which lungs can readily expand Affected by the elasticity of the lungs and the thoracic cage which can be diminished by 2 main factors: Fibrosis of the lung tissue Ossification and/or muscle paralysis impairs flexibility of the thoracic cage Lung fibrosis Lung Elasticity Essential for normal expiration Emphysema: tissue becomes less elastic and more fibrous loss of elasticity & increase in fibrous tissue causes enormous effort to exhale – at end stages, alveolar walls break down and surface area is lost for gas exchange Alveolar Surface Tension forces Surface tension is caused by the tendency of polar molecules such as water to stick to each other with hydrogen bonds this can cause the walls of the alveoli to stick together like plastic wrap every time you exhale. Large amounts of energy /effort will be required to simply re-expand the lungs and allow you to inhale (IRDS) Alveolar Surface Tension Forces Surfactant – interferes with cohesion of water molecules so less energy needed to expand lungs – this is one of the things that keeps our lungs partially expanded at all times. (the other thing is the pressure difference previously discussed) Secreted by Type II cells in lungs Alveoli & Surface Tension IRDS – Infant Respiratory Distress Syndrome AKA: Hyaline Membrane Disease Caused by lack of surfactant due to prematurity 28 weeks of gestation is considered Nonrespiratory Air Maneuvers Reaction or reflex response • Cough • Sneeze –travels up to 40 miles per hour • Hiccup – phrenic nerve irritation causes diaphragm to spasm • Yawn – saturates alveoli with fresh air Need for increased oxygen Control of Breathing Neural Medulla oblongata sets rate of breathing Pons fine-tunes rate and transition Hering-Breuer Reflexes Stimulation is sent Inflation reflex- prevents overexpansion via receptors around bronchioles Deflation reflex – inhibits expiratory centers and stimulates inspiratory centers. Receptors in alveolar walls Usually during forced activity Control of Breathing Chemical Factors Central chemoceptors monitor pH levels in cerebrospinal fluid. High levels of CO2 increase hydrogen level in blood – therefore pH decreases. Peripheral chemoreceptors located in aorta and carotid arteries monitor blood oxygen level. Mechanoreceptors located in muscles and joints detect muscle contraction and force increased ventilation. Lung Volume Static Lung Volume Instructed to perform following breathing maneuvers Tidal volume – amount inhaled during normal breathing Vital capacity – breath in maximum, followed by maximum expiration Lung Volume Residual volume – volume of air that never leaves the lungs Important for continual gas exchange Lung Volume Dynamic Lung Volume End of Quiz #2 Material