Chapter 23 - FacultyWeb
advertisement

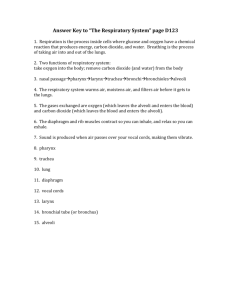
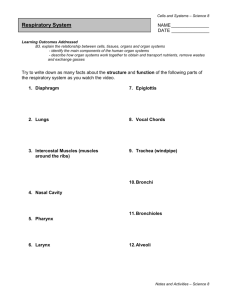
Which structure is not part of the lower respiratory system? 1. 2. 3. 4. Larynx Pharynx Trachea Bronchi Which structure is the final part of the conduction portion of the respiratory tract? 1. 2. 3. 4. Alveolar sacs Tertiary bronchi Respiratory bronchioles Terminal bronchioles What role do the nasal conchae play in the respiratory system? 1. 2. 3. 4. Trapping airborne particles in mucus Warming and humidifying incoming air Bringing olfactory stimulation to olfactory receptors All of the above are correct The epithelium of the pharynx changes from ____ in the nasopharynx to ____ in the oropharynx. Why? 1. 2. 3. 4. Pseudostratified ciliated columnar to stratified squamous/oropharynx is subject to abrasion Simple cuboidal to pseudostratified ciliated columnar/gas exchange occurs in the nasal cavity Stratified squamous to pseudostratified ciliated columnar/nasopharynx contains goblet cells None of the above. Why are the cartilages that reinforce the trachea C-shaped? 1. 2. 3. 4. To prevent tracheal crushing To conform to thoracic cavity shape To allow room for esophageal expansion To allow normal cardiac functioning What happens to the alveoli if surfactant is not produced? Why? 1. The alveoli contract/elastic recoil of lungs 2. The alveoli collapse/increase in surface tension 3. The alveoli expand/intrapleural pressure decreases 4. The alveoli burst/increase in intrapulmonary pressure What path does air take in flowing from the glottis to the respiratory membrane? 1. Larynx, trachea, bronchi, alveolar duct, alveolar sac, respiratory membrane 2. Larynx, trachea, alveolar duct, bronchioles, respiratory membrane 3. Trachea, bronchi, larynx, bronchioles, alveolar duct, alveolar sac 4. Larynx, trachea, bronchioles, alveolar duct, bronchi, alveolar sac, respiratory membrane Which arteries supply blood to the conducting portions of the respiratory tract? 1. 2. 3. 4. External carotid arteries Bronchial arteries Thyrocervical trunk All of the above What is the primary function of pleura. What does it secrete? 1. 2. 3. 4. Reduces surface tension/surfactant Reduces friction between visceral and parietal pleura/pleural fluid Prevents lungs from drying out/mucus Prevents friction between heart and lungs/serous fluid What does Boyle’s Law state concerning the relationship between pressure and volume? 1. 2. 3. 4. If you decrease the volume of a gas, its pressure will decrease. If you increase the volume of a gas, its pressure will decrease. P = 1/V 2 and 3 are correct. The primary function of pulmonary ventilation is _____. 1. Maintaining adequate alveolar ventilation 2. Diffusion of gases across the respiratory membrane 3. Transport of O2 and CO2 between capillaries and tissues 4. Absorption of O2 and release of CO2 in tissues Which factor influencing compliance increases compliance? 1. Inadequate secretion of surfactant 2. Restricted movement of thoracic cage 3. Loss of connective tissue resulting from alveolar damage 4. The percent of oxygen in inhaled air Why is it important to exhale while lifting weights? 1. To relax the diaphragm 2. To equalize pressures inside and outside the thoracic cavity 3. To enhance action of the accessory respiratory muscles 4. To prevent intrapulmonary pressure from increasing Mark breaks a rib that punctures his left lung. What will happen to his left lung as a result? What happens to his right lung? 1. Fluids leak into the alveoli/decrease in respiratory function 2. Atelectasis/nothing 3. Increase in compliance/decrease in surface area for gas exchange 4. Bronchodilation/atelectasis Which respiratory muscles become actively involved only during a forced inspiration? 1. Diaphragm and external intercostal muscles 2. Internal intercostal muscles as well as external and internal oblique muscles 3. Pectoralis minor, scalenes, and serratus anterior 4. 1 and 3 are correct Why is VA more important than the respiratory minute volume? 1. 2. 3. 4. VA determines the rate of O2 delivery to alveoli. VA determines the volume of dead space. VA determines the amount of air moved each minute. VA determines functional reserve capacity. If you have maximally exhaled all the air you can (ERV), what is the amount you can now maximally inhale? 1. 2. 3. 4. Inspiratory reserve volume Vital capacity Inspiratory capacity Residual volume How is inspiratory capacity calculated? 1. It is the amount of air one can inhale beyond TV. 2. TV + IRV 3. ERV + TV + IRV 4. FRC + TV + IRV In pneumonia, fluid accumulates in the alveoli of the lungs and bronchioles constrict. What effect does pneumonia have on vital capacity? 1. Increase in vital capacity 2. Decrease in vital capacity 3. Increase in breathing rate, with no effect on vital capacity 4. Decrease in tidal volume, with no effect on vital capacity Which Gas Law states, “At a given temperature, the amount of a particular gas in solution is directly proportional to the partial pressure of that gas”? 1. 2. 3. 4. Boyle’s Law Dalton’s Law The Bohr effect Henry’s Law Which of the following is false concerning the efficiency of gas exchange. 1. Total surface area for gas exchange is large. 2. Gases are lipid soluble. 3. The difference in partial pressure across the respiratory membrane is minimal. 4. Blood flow and airflow are coordinated. What do increased temperatures in active skeletal muscles and increased concentrations of BPG have in common? What is the result? 1. Both allow the Hb molecule to release O2 more readily/improved tissue oxygenation 2. Both cause the Hb molecule to bind O2 more tightly/determines how long a blood bank can store blood 3. Both allow Hb to have a higher affinity for O2/ improved O2 transfer across the placenta 4. 1 and 3 are correct What is the functional relationship between hemoglobin and pH? 1. 2. 3. 4. As pH drops, the Hb molecule changes shape. As pH drops, O2 saturation declines. As pH increases, Hb releases O2 more readily. 1 and 2 are correct. Which of the following is not a method of carbon dioxide transport in blood? 1. 2. 3. 4. As molecules of carbonic acid In plasma Binding to iron in Hb All of the above are methods of carbon dioxide transport What effect does a decrease in pneumotaxic output have on breathing? Why? 1. 2. 3. 4. Shorter breaths and increased respiration rate/ stimulation of the VRG Decreased respiratory rate and increased depth of respiration/the apneustic centers are stimulated Neurons of the VRG activate accessory muscles of inhalation/little pulmonary ventilation is occurring None of the above is correct Beyond transport of respiratory gases, how do the respiratory and cardiovascular systems interact? 1. Regulation of BP by activation of angiotensin II 2. Bicarbonate ions contributing to the buffering capacity of blood 3. Maintenance of normal fluid and ion balance 4. 1 and 2 are correct