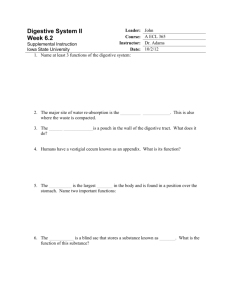
2. Secretion.
advertisement

Lec.1 Medical Physiology Z.H.Kamil PHYSIOLOGY OF THE GASTROINTESTINAL TRACT (GIT) The alimentary tract provides the body with a continual supply of water, electrolytes, and nutrients. To achieve this requires (1) movement of food through the alimentary tract; (2) secretion of digestive juices and digestion of the food; (3) absorption of water, various electrolytes, and digestive products; (4) circulation of blood through the gastrointestinal organs to carry away the absorbed substances; and (5) control of all these functions by local, nervous, and hormonal systems. Functions of GIT Overall, the digestive system performs six basic processes: 1. Ingestion. This process involves taking foods and liquids into the mouth (eating). 2. Secretion. Each day, cells within the walls of the GI tract and accessory digestive organs secrete a total of about 7 liters of water, acid, buffers, and enzymes into the lumen (interior space) of the tract. 3. Mixing and propulsion. Alternating contractions and relaxations of smooth muscle in the walls of the GI tract mix food and secretions and propel them toward the anus. This capability of the GI tract to mix and move material along its length is called motility. 4. Digestion. Mechanical and chemical processes break down ingested food into small molecules. In mechanical digestion the teeth cut and grind food before it is swallowed, and then smooth muscles of the stomach and small intestine churn the food. As a result, food molecules become dissolved and thoroughly mixed with digestive enzymes. In chemical digestion the large carbohydrate, lipid, protein, and nucleic acid molecules in food are split into smaller molecules by hydrolysis. Digestive enzymes produced by the salivary glands, tongue, stomach, pancreas, and small intestine catalyze these catabolic reactions. A few substances in food can be absorbed without chemical digestion. These include vitamins, ions, cholesterol, and water. 5. Absorption. The entrance of ingested and secreted fluids, ions, and the products of digestion into the epithelial cells lining the lumen of the GI tract is called absorption. The absorbed substances pass into blood or lymph and circulate to cells throughout the body. 6. Defecation. Wastes, indigestible substances, bacteria, cells sloughed from the lining of the GI tract, and digested materials that were not absorbed in their journey through the digestive tract leave the body through the anus in a process called defecation. The eliminated material is termed feces. Divisions of The Digestive System The gastrointestinal system consists of the gastrointestinal tract and the accessory exocrine glands. The gastrointestinal tract includes the mouth, the esophagus, the stomach, the small intestine, and the large intestine. The major accessory glands are the salivary glands, the liver, the gallbladder, and the pancreas. Figure 1 shows the entire alimentary tract. Each part is adapted to its specific functions: some to simple passage of food, such as the esophagus; others to temporary storage of food, such as the stomach; and others to digestion and absorption, such as the small intestine. Types of Digestion The food we eat is broken down in two complementary processes: mechanical digestion and chemical digestion. Mechanical digestion is the physical breaking up of food into smaller pieces. Chewing is an example of this. As food is broken up, more of its surface area is exposed for the action of digestive enzymes. The work of the digestive enzymes is the chemical digestion of broken-up food particles, in which complex chemical molecules are changed into much simpler chemicals that the body can utilize. Such enzymes are specific with respect to the fat, protein, or carbohydrate food molecules each can digest. For example, protein-digesting enzymes work only on proteins, not on carbohydrates or fats. Each enzyme is produced by a particular digestive organ and functions at a specific site. However, the enzyme’s site of action may or may not be its site of production. Figure 1: Divisions of GIT Neural Control of Gastrointestinal Function— Enteric Nervous System The gastrointestinal tract has a nervous system all its own called the enteric nervous system. It lies entirely in the wall of the gut, beginning in the esophagus and extending all the way to the anus. The number of neurons in this enteric system is about 100 million, almost exactly equal to the number in the entire spinal cord. This highly developed enteric nervous system is especially important in controlling gastrointestinal movements and secretion. In general, stimulation of the sympathetic nervous system inhibits activity of the gastrointestinal tract, causing many effects opposite to those of the parasympathetic system. It exerts its effects in two ways: (1) to a slight extent by direct effect of secreted norepinephrine to inhibit intestinal tract smooth muscle (except the mucosal muscle, which it excites) and (2) to a major extent by an inhibitory effect of norepinephrine on the neurons of the entire enteric nervous system. Strong stimulation of the sympathetic system can inhibit motor movements of the gut so greatly that this literally can block movement of food through the gastrointestinal tract. -Hormonal Control of Gastrointestinal Motility Although the motility effects are usually less important than the secretory effects of the hormones, some of the more important of them are the following: Gastrin is secreted by the “G” cells of the antrum of the stomach in response to stimuli associated with ingestion of a meal, such as distention of the stomach, the products of proteins, and gastrin releasing peptide. The primary actions of gastrin are (1) stimulation of gastric acid secretion. (2) stimulation of growth of the gastric mucosa. Cholecystokinin is secreted by “I” cells in the mucosa of the duodenum and jejunum mainly in response to digestive products of fat, fatty acids, and monoglycerides in the intestinal contents. This hormone strongly contracts the gallbladder, expelling bile into the small intestine where the bile in turn plays important roles in emulsifying fatty substances, allowing them to be digested and absorbed. Cholecystokinin also inhibits stomach contraction moderately. Therefore, at the same time that this hormone causes emptying of the gallbladder, it also slows the emptying of food from the stomach to give adequate time for digestion of the fats in the upper intestinal tract. Secretin was the first gastrointestinal hormone discovered and is secreted by the “S” cells in the mucosa of the duodenum in response to acidic gastric juice emptying into the duodenum from the pylorus of the stomach. Secretin has a mild effect on motility of the gastrointestinal tract and acts to promote pancreatic secretion of bicarbonate which in turn helps to neutralize the acid in the small intestine. Gastric inhibitory peptide is secreted by the mucosa of the upper small intestine, mainly in response to fatty acids and amino acids but to a lesser extent in response to carbohydrate. It has a mild effect in decreasing motor activity of the stomach and therefore slows emptying of gastric contents into the duodenum when the upper small intestine is already overloaded with food products. Motilin is secreted by the upper duodenum during fasting, and the only known function of this hormone is to increase gastrointestinal motility. Motilin secretion is inhibited after ingestion by mechanisms that are not fully understood. Movements in the Gastrointestinal Tract Two types of movements occur in the gastrointestinal tract: (1) propulsive movements, which cause food to move forward along the tract at an appropriate rate to accommodate digestion and absorption. The basic propulsive movement of the gastrointestinal tract is peristalsis, which is a reflex response that is initiated when the gut wall is stretched by the contents of the lumen, and it occurs in all parts of the gastrointestinal tract from the esophagus to the rectum. The stretch initiates a circular contraction behind the stimulus and an area of relaxation in front of it (Figure 2). The wave of contraction then moves in an oral-to-caudal direction, propelling the contents of the lumen forward at rates that vary from 2 to 25 cm/s. Peristaltic activity can be increased or decreased by the autonomic input to the gut, but its occurrence is independent of the extrinsic innervations. Indeed, progression of the contents is not blocked by removal and resuture of a segment of intestine in its original position and is blocked only if the segment is reversed before it is sewn back into place. Peristalsis is an excellent example of the integrated activity of the enteric nervous system. (2) mixing movements, which keep the intestinal contents thoroughly mixed at all times. When the meal is present, the enteric nervous system promotes a motility pattern that is related to peristalsis, but is designed to retard the movement of the intestinal contents along the length of the intestinal tract to provide time for digestion and absorption (Figure 2). This motility pattern is known as segmentation, and it provides for ample mixing of the intestinal contents (known as chyme) with the digestive juices. A segment of bowel contracts at both ends, and then a second contraction occurs in the center of the segment to force the chyme both backward and forward. Unlike peristalsis, therefore, retrograde movement of the chyme occurs routinely in the setting of segmentation. This mixing pattern persists for as long as nutrients remain in the lumen to be absorbed. It presumably reflects programmed activity of the bowel dictated by the enteric nervous system, and can occur independent of central input, although the latter can modulate it. Figure 2: Peristalsis and Segmentation