Chapter 43
advertisement

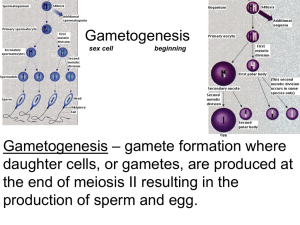
Exercise 45 Physiology of Reproduction 1 Meiosis Gametes Haploid complement (n) Gametogenesis Process of gamete formation with the reduction by half of the chromosome number Homologous chromosome Carries genes for the same traits 2 Meiosis 3 Meiosis I Prophase • 23 tetrads • Homologues chromosomes synapse • Chiasmata or crossover Meiosis Metaphase Anaphase • Homologues separates • Dyads stays together Telophase • 2 cells with diploid number of chromosomes 4 Meiosis 5 Meiosis II Prophase • No chromosome replication • Cells are diploid Metaphase Meiosis Anaphase • Breaks of the centromeres will result each cell having one chromatid • 4 daughter cells • Crossover and the way in which the homologues align on the spindle equator during the first maturation division introduces a great variability in the resulting gametes 6 Spermatogenesis It is the male gamete formation Starts at puberty and continues throughout life 7 Spermatogenesis 8 Spermatogenesis Steps of sperm formation: Spermatogonia (2n) Stem cell Found in the seminiferous tubules It undergoes mitosis and forms one primary spermatocyte and one spermatogonium Phase regulated by FSH 9 Spermatogenesis Primary spermatocyte (2n) It undergoes to a growth phase It undergoes to meiosis I after the growth phase and forms the secondary spermatocyte Secondary spermatocyte (n) It undergoes meiosis II and produces 4 spermatids 10 Spermatogenesis 11 Spermatids (n) Nonfunctional gametes No motile They undergo spermiogenesis and form the sperm Spermatogenesis 12 Sperm Motile Smaller than the spermatid Head of the sperm • Contain the genetic material • Acrosome Spermiogenesis 13 Spermatogenesis Midpiece • Centriole that gives rise to the filaments that forms the tail • Mitochondria present Tail • flagellum 14 Spermatogenesis 15 Sertoli cells Support cells responsible for sperm nourishment Oogenesis and ovarian cycle It is the female gamete formation Steps of the oogenesis: Before birth Oogonia • Primitive stem cell • it undergoes mitosis many times • It grows in size and becomes a primary oocyte 16 Oogenesis and ovarian cycle Primordial follicles • Capsule formed by a single layer of squamouslike cells that surround the primary oocyte At birth Oogonias no longer exists All cells are oocytes encapsulated by a primordial follicle No more oocytes will be produced 17 Oogenesis and ovarian cycle From birth to puberty Primary oocytes are quiescent From puberty and on Increase of FSH levels cause: Follicle One or more primordial follicles to undergo maturation (every 28 days) 18 Follicle 19 Oogenesis and ovarian cycle Formation of primary follicle • From the maturation of the primordial follicle • Follicle cells • The epithelium changes from squamous to simple cuboidal • Many layers of cuboidal cells • Granulosa • It secrets estrogen 20• It contains the primary oocyte Oogenesis and ovarian cycle Secondary follicle • Follicle with several layers of granulosa cells • Presence of antrum Tertiary follicle (Graafian) • Presence of granulosa cells • Corona radiata 21 Oogenesis and ovarian cycle • It is a mature follicle that continues secreting increasing amounts of estrogen • It contains the secondary oocyte • It expels the secondary oocyte accompanied by the corona radiata at the middle of the 28-day cycle 22 Oogenesis and ovarian cycle Corpus luteum • It comes from the rupture Graafian follicle • It produces mainly progesterone • If pregnancy does not occur it will degenerate and will be replaced by scar tissue 23 Oogenesis and ovarian cycle Corpus albicans • Scar tissue resulted from the disintegration of the corpus luteum Oocyte Primary oocyte Meiosis I is completed forming one secondary oocyte and one first polar body 24 Follicle 25 Oogenesis 26 Oogenesis and ovarian cycle 27 Secondary oocyte Large cell (contains most of the cytoplasm of the primary oocyte) Haploid Arrested in metaphase of meiosis II It is expelled by the Graafian follicle (ovulation) It is captured by the uterine tube Oogenesis and ovarian cycle If penetrated by the sperm, it will complete meiosis II and will produce a large ovum and one small secondary polar body Ovum Chromosomes of the ovum and sperm will combine to form a diploid cell 28 Oogenesis and ovarian cycle 29 First polar body Small cell (almost no cytoplasm) Produced by the division of the primary oocyte It will disintegrate Secondary polar body Produced by the division of the secondary oocyte It will also disintegrate Oogenesis and ovarian cycle Hormonal cycle Beginning of the menstrual cycle FSH is the dominant hormone Low levels of LH Low levels of estrogen and progesterone 30 Oogenesis and ovarian cycle 31 Before ovulation Estrogen levels increase Progesterone level remain low Ovulation Caused mainly by a peak of LH After ovulation Estrogen levels decrease Progesterone levels increase FSH and LH levels decrease Menstrual cycle Controlled by ovarian hormones Menstrual phase Lasts 1-5 days Sloughing off of the functional layer of the endometrium with bleeding 32 Oogenesis and ovarian cycle 33 Proliferative phase From day 6-14 Estrogen is the main hormone Ovarian follicle grows Endometrium thickens with proliferation of its glands and blood vessels Ovulation occur at day 14 Oogenesis and ovarian cycle 34 Secretory phase From day 15-28 Progesterone produced by the corpus luteum is the main hormone Endometrium thickens even more with further proliferation and coiling of the glands Uterus is getting ready for the embryo implantation Oogenesis and ovarian cycle 35 If no implantation occurs the corpus luteum will deteriorate causing lack of ovarian hormones that will cause deterioration of the functional layer of the endometrium Menstrual cycle 36