03. COPD
advertisement

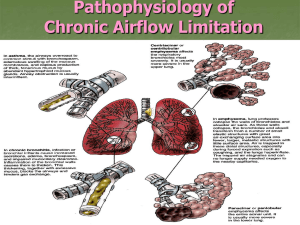
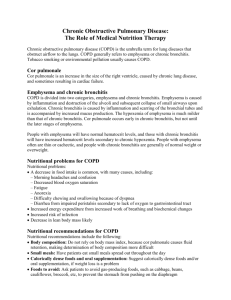
Chronic obstructive bronchitis and emphysema chronic obstructive airway disease (COAD, COLD) ( chronic obstructive pulmonary disease ) COPD COPD emphysema „pink puffer” bronchitis „blue bloater” 1. COPD, a common preventable and treatable disease, is characterized by persistent airflow limitation. 2. The airway obstruction is usually progessive and associated with an enhanced chronic ionflammatory response in the airways and the parenchyma to noxius particles and gases. 3. Exacerbations and comorbidities contribute to the overall severity in an individual patient. GOLD 2011 Percent Change in Age-Adjusted Death Rates, U.S., 1965-1998 Proportion of 1965 Rate 3.0 3.0 2.5 2.5 Coronary Heart Disease Stroke Other CVD COPD All Other Causes –59% –64% –35% +163% –7% 2.0 2.0 1.5 1.5 1.0 1.0 0.5 0.5 0.0 0 1965 - 1998 1965 - 1998 1965 - 1998 1965 - 1998 1965 - 1998 „Global burden of disease” (Science 1996; 274:740-743.) Epidemiology 4-7% of adult population, 9-10 % for those over 40 Prevalence expected to rise 3x in 10 years. By 2020, it becomes the 3rd most frequent cause of death COPD morbidity in Hungary OKTPI, 2015 Prevalence 180 983 Incidence 15 362 CIBA Guest Symposium: Terminology, definitions and classifications of chronic pulmonary emphysema and related conditions (1959) 1./ Obstructive emphysema: abnormal permanent enlargement of the airspaces distal to the terminal bronchioles, accompanied by destruction of the alveolar walls and without obvious fibrosis. 2./ Chronic bronchitis: the presence of chronic productive cough for 3 months in each of 2 successive years in a patient in whom other causes (heart failure, tbc, bronchiectasis, tumor, lung abscess) of chronic cough have been excluded. Differential diagnosis of airway obstruction Chronic bronchitis Emphysema COPD Airflow obstruction Asthma Adapted from Snider 1995 Etiology: host factors Etiology: acquired risk Effect of smoking on annual decline in lung function Fletcher C, Peto R: BMJ 1977:i: 1645 ? CD8+ lymphocyta Alveolar macrophage neutrophil chemotactic factors cytokines ( IL-8 ) mediators ( LTB4 ) neutrophil alfa1-antitrypsin SLPI protease inhibitors - alveolar destruction ( emphysema) proteázok proteases neurophil elastase cathepsines matrix metalloproteinases increased mucus productio ( chronic bronchitis ) Pathology 1. chronic bronchitis – increased mucus production, chronic cough 2. obstructiv bronchiolitis – small airway obstruction with inflammation and fibrosis of bronchioles 3. Emphysema – alveolar destruction, hiperinflation, loss of elastic recoil, gázcserezavar, bronchiális obstrukció Small airways in COPD Barnes, NEJM,2004 Loss of alveolar attachments in smokers Normal Smoker Saetta et al. ARRD 1985 Airway muscle thickness Increase in COPD Non-smoker COPD Saetta. 1998 Causes of Airflow Limitation • Irreversible – Fibrosis and narrowing of the airways – Loss of elastic recoil due to alveolar destruction – Destruction of alveolar support that maintains patency of small airways Causes of Airflow Limitation • Reversible – Accumulation of inflammatory cells, mucus, and plasma exudate in bronchi – Smooth muscle contraction in peripheral and central airways – Dynamic hyperinflation during exercise Driving pressure (parenchyma) Resistance (small airways) Airflow = limitation Pathology and gas exchange in COPD Stockley, Rennard, Rabe, Celli, 2007 Differencial diagnostics • • • • Asthma CHF Bronchiectasis Bronchiolitis obliterans (young, non-smoker, RA, smoke exposition, HRCT:hypodens area) • Diffuse panbronchiolitis (non-smoker malei, sinusitis, HRCT:centrilobular foci and hyperinflation) Inflammation and lung function In asthma and COPD Overlap ~ 10 - 40% Barnes, 2009 asthma COPD neutrophils mild AHR* no(poor) bronchodilation no corticosteroid effect eosinophils AHR* 10 – 40 % good bronchodilator effect good corticosteroid effect “ Wheezy bronchitis ” reversibility threshold: 12 –15% (>200ml) FEV1increase *AHR= airway hyperreactivity Characteristics of phenotypes bronchitis Dynamic lung volumes decreased emphysema decreased ( FEV1 , FEV1/FVC) Static lung volumes TLC RV Diffusion capacity Blood gas exercise Cor pulmonale normal or mild increase moderate increase increased increasd normal or mild decrease decreased hypoxaemia, hypercapnia hypoxaemia: no change, improves or deteriorates frequently hypoxaemia in end-stage hypoxaemia deteriorates seldom Diagnosis: postbronchodilator (4 puff salbutamol) FEV1/FVC<70% Classification FEV1 (ref %) symptoms cough, sputum mild moderate severe very severe 80 % morning sputum, minimal breathing dyscomfort 50 - 80 % dyspnea on moderate exertion with or without wheezing, discolored sputum, acute worsening with infection, with significant erosion of QoL 30 – 50 % < 30% n cough, wheezing, breathlessness on minimal exertion signs of RHF, significantly impaired QoL Pharm.spir. Beta-2 agonist Parasympatholytics Xantin derivate Systemic consequences/comorbidities in COPD COPD COPD Exacerbation Expiratory flow limitation Air trapping Hyperinflation Dyspnea Reduced exercise tolerance Quality of life Inactivity Deconditioning Systemic consequences e.g. Muscle atropgy/wasting, atherosclerosis, depression, osteoporosis, anaemia, diabetes Airway inflammation and systemic consequences in COPD (theory) Tüdő Muscle wasting/atrophy TNFa Inzulin resistance, II. type diabetes IL-6 ? Local inflammation Cardiovascular events CRP Liver Osteoporosis GOLD Workshop Report Four components of COPD Management 1. Asses and monitor disease 2. Reduce risk factors 3. Manage stabil COPD Education PharmacologicGyógyszeres Non-pharmacologic 4. Manage exacerbations Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEFV1 Anthonisen N.R. és mtsai. JAMA 1994: 272, 1497-1505. Smoking cessation is the only intervention which may retard the steep loss in lung function in COPD 1/3 of patients are able to do this (nicotin replacement, bupropion, vareniclin) Smoking: early and late quit Doll, BMJ 2004 34 439 Brittish male physicians, 1951-2001 Treatment of COPD ipratropium bromid, (SAMA) MDI, 4 x 3-6 ( 60-120 µg ) puff + β2 agonist (SABA) MDI 4 x 2-4 puff ( 200-400 µg ) + LAMA (tiotropium) DPI, 1x1 LABA (salmeterol, formoterol) 2x1 or (indacaterol, olodaterol) 1x1 ICS/LABA + retard theophyllin tabl. 300-900 mg ( Se- level 8-12 µg/ml ) antibiotics(5-10 days) + corticosteroid exacerbation (32 mg methylprednisolon, 10-14 days) fluticason/salmet erol or budesonid/formot erol Treatment of COPD Surgical treatment ? (GOLD 2006) longterm oxigen treatment (chronic respiratoryy failure) inhalative corticosteroids ( 3 exacerbation in the previous 3 years) One or more long acting bronchodilators, rehabilitation Short acting anticholinergic and/or 2-agonist as needed Avoidance of risk factors, influenza FEV1 80% without 50% FEV1 < 80% or vaccination 30% FEV1 < 50% with symptoms FEV1 < 30% or chronic respiratory or right heart failure airway obstruction (FEV1/FVC < 70%) I. mild II. moderate III. severe IV. very severe Longterm oxygen in COPD NOTT: Ann Intern Med, 1980 BMC: Lancet, 1981 the only treatment which prolongs life in hypoxic COPD Indication: resting • PaO2 < 55 mmHg or SAT < 88% • 55 Hgmm < PaO2 < 60 mmHg, and pulmonary hypertension, polyglobulia or heart failure Target: PaO2 ≈ 60 mmHg or SAT ≈ 90 % Pa CO2 increase < 15-20 mmHg Dose: > 15 h/day, 1-2 L/min through nasal prong Respiratory insufficiency in COPD acute exacerbation pink puffer partial (hypoxaemic/transfer failure) blue bloater global (pump-, ventilatory failure) Main symptomps in acute exacerbation of COPD increased dyspnea wheezing, chest tightness, increased cough and sputum purulence +/- reduced exercise tolerance, fever , change in chest x-ray, leukocytosis +/- malice, disturbed sleep, daytime sleepiness, depression, confusion (CO2 retention) Antibacterial treatment of AECOPD pathogens 1./ acute tracheobronchitis atipical agent 2./ Chronic bronchitis without comorbidity treatment ? H. influenzae M. catarrhalis res. S. pneumoniae ? ( FEV1 > 50% ) 3./ Chronic bronchitis with comorbidity ( FEV1 < 50% ) „ res. Pneumococcus ! 4./ Chronic bronchial infection „ Gram-neg enterobact. macrolide ? aminopenicillin/cv cefalo. II, III makrolide II. „ respiratory kinolon respiratory kinolon Ps. eruginosa = ciprofloxacin Non-invasive mechanical ventilation in respiratory insufficiency