Medical Nutrition Therapy for Chronic Obstructive
advertisement
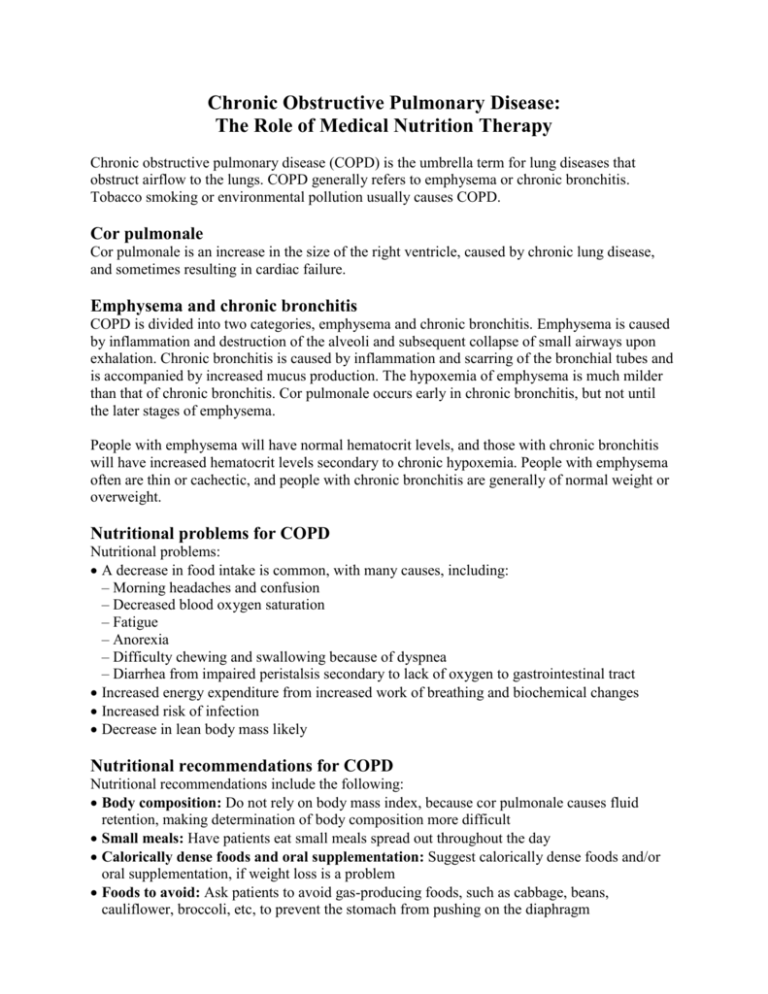
Chronic Obstructive Pulmonary Disease: The Role of Medical Nutrition Therapy Chronic obstructive pulmonary disease (COPD) is the umbrella term for lung diseases that obstruct airflow to the lungs. COPD generally refers to emphysema or chronic bronchitis. Tobacco smoking or environmental pollution usually causes COPD. Cor pulmonale Cor pulmonale is an increase in the size of the right ventricle, caused by chronic lung disease, and sometimes resulting in cardiac failure. Emphysema and chronic bronchitis COPD is divided into two categories, emphysema and chronic bronchitis. Emphysema is caused by inflammation and destruction of the alveoli and subsequent collapse of small airways upon exhalation. Chronic bronchitis is caused by inflammation and scarring of the bronchial tubes and is accompanied by increased mucus production. The hypoxemia of emphysema is much milder than that of chronic bronchitis. Cor pulmonale occurs early in chronic bronchitis, but not until the later stages of emphysema. People with emphysema will have normal hematocrit levels, and those with chronic bronchitis will have increased hematocrit levels secondary to chronic hypoxemia. People with emphysema often are thin or cachectic, and people with chronic bronchitis are generally of normal weight or overweight. Nutritional problems for COPD Nutritional problems: A decrease in food intake is common, with many causes, including: – Morning headaches and confusion – Decreased blood oxygen saturation – Fatigue – Anorexia – Difficulty chewing and swallowing because of dyspnea – Diarrhea from impaired peristalsis secondary to lack of oxygen to gastrointestinal tract Increased energy expenditure from increased work of breathing and biochemical changes Increased risk of infection Decrease in lean body mass likely Nutritional recommendations for COPD Nutritional recommendations include the following: Body composition: Do not rely on body mass index, because cor pulmonale causes fluid retention, making determination of body composition more difficult Small meals: Have patients eat small meals spread out throughout the day Calorically dense foods and oral supplementation: Suggest calorically dense foods and/or oral supplementation, if weight loss is a problem Foods to avoid: Ask patients to avoid gas-producing foods, such as cabbage, beans, cauliflower, broccoli, etc, to prevent the stomach from pushing on the diaphragm Carbonated beverages: Tell patients to avoid drinking carbonated beverages with meals to prevent early satiety Medications: Explain that many drugs, including bronchodilators, expectorants, and corticosteroids, may have food-drug implications Indirect calorimetry: Know that indirect calorimetry is recommended, whenever possible (energy needs are highly variable). Realize that patients will require 1.2-1.7 grams protein/kilogram dry weight/day Protein, fat, and carbohydrates: Understand that protein should account for 15% to 20% of total calories, fat 30% to 45% of total calories, and carbohydrate 40% to 55% of total calories for optimal respiratory quotient Vitamin C for smokers: Suggest vitamin C supplementation for patients who smoke Vitamin D, calcium, and phosphorus: Recommend supplementation of vitamin D, calcium, and phosphorus, because many patients with COPD exhibit a decrease in bone density Fluid restriction: Restrict fluids for patients who have cor pulmonale (usually necessary). Sodium: Consider fluid restriction, if fluid retention is evident Mealtime: Remind patients that they should eat slowly, chew well, and rest before mealtime. Encourage socialization during mealtime, if family/friends are available. Explain that patients should use oxygen during mealtime Social service programs: Make referrals to social service programs if patients are having trouble shopping or preparing their own food Alcohol: Strongly suggest that patients with COPD avoid alcohol, because it slows respiration References and recommended readings Academy of Nutrition and Dietetics. Nutrition Care Manual® [by subscription]. Nutrition Care Manual Web site. www.nutritioncaremanual.org. Accessed March 29, 2014. Chronic obstructive pulmonary disease (COPD). Merck Manuals Web site. http://www.merck.com/mmpe/sec05/ch049/ch049a.html#sec05-ch049-ch049a-479. Updated November 2013. Accessed March 29, 2014. Mayo Clinic staff. COPD. Mayo Clinic Web site. http://www.mayoclinic.com/print/copd/DS00916/DSECTION=all&METHOD=print. Accessed March 29, 2014. Mueller DH. Medical nutrition therapy for pulmonary disease. In: Mahan LK, Escott-Stump S, Raymond J. Krause’s Food and the Nutrition Care Process. 13th ed. St Louis, MO: Elsevier Saunders; 2012:782-798, 945-948. Wouters EF. Nutrition and metabolism in COPD. Chest. 2000;117(5 suppl 1):274S-280S. Review Date 3/14 G-0618