Chronic Obstructive Lung Disease Emphysema Risk Factors
advertisement
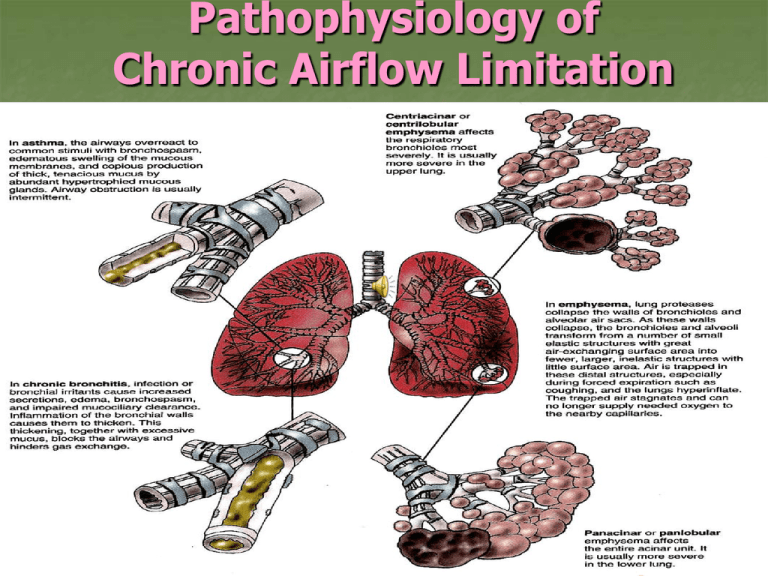
Pathophysiology of Chronic Airflow Limitation Chronic Obstructive Lung Disease Emphysema Abnormal permanent enlargement of the airspaces distal to the terminal bronchioles, accompanied by destruction of their walls and without obvious fibrosis Risk Factors: Cigarette Smoking Irritation - > 4,000 chemicals inhaled Hyperplasia – reduces airway diameter Abnormal dilatation of distal airspaces Destruction of alveolar walls Chronic Obstructive Lung Disease Emphysema Risk Factors (cont’d): Recurring respiratory tract infections Heredity – alpha 1 –Antitrypsin (ATT) deficiency H. flu, Strep pneumoniae, Moraxella catarrhalis Accounts for <1% of COPD in US AAT is a serum protein produced by the liver and normally found in the lungs IV or nebulized AAT (Prolastin) slows COPD progression Aging – Changes in lung structure Gradual loss of elastic recoil – thin alveolar wall – thoracic cage changes from osteoporosis & calcification COPD Pulmonary Blebs & Bullae Pathophysiology of Chronic Bronchitis and Emphysema Interferences with Ventilation Collaborative Care Goals Improve ventilation Promote removal of secretions Prevent complications & progression of symptoms Promote patient comfort & participation in care Improve quality of life as much as possible Interferences with Ventilation Collaborative Treatment Patients are treated primarily as outpatients Hospitalizations Acute exacerbations Complications Respiratory failure, pneumonia, congestive heart failure Interferences with Ventilation Collaborative Management Smoking cessation Treatment of respiratory infections Bronchodilator therapy Beta2-adrenergic agonists Anticholinergic agents Long-acting theophylline Corticosteroids PEFR monitoring (peak expiratory flow rate) Chest physiotherapy / Breathing exercises & retraining Hydration 3L/day (unless contraindicated) Rest - Progressive plan of exercise Patient & family education Influenza / Pneumovax immunization Low flow oxygen rate (if indicated) Pulmonary rehabilitation program