COPD: Prevention, Identification & Management
advertisement

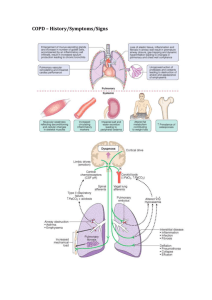
COPD: Prevention, Identification & Management Dr. Kenya V. Beard Ed.D. CNE GNP-BC NP-C ACNP-BC K Beard & Associates, LLC President Hunter College, Assistant Professor KBeard@hunter.cuny.edu Objectives Discuss the role of the nurse in caring for clients with COPD Compare and Contrast Emphysema and Chronic Bronchitis COPD 4th Leading cause of death in the Untied States COPD mortality rate has increased over the last 30 years Malnutrition- Found in up to 1/3rd of individuals with COPD Adversely affects exercise tolerance, surfactant production, protein synthesis, and it increases morbidity and mrotality. Role of Pulmonary System: Ventilation Gases must move into and out of the lungs Ventilatory rate measures how many times gas is inhaled and exhaled over one minute Minute volume aka minute ventilation represents the ventilatory rate x tidal volume (volume of air per breath) Why is CO2 elimination necessary? How does the health care professional determine whether ventilation is adequate? Pulmonary System Bring oxygen to alveoli, diffuse oxygen into and carbon dioxide out of blood Alveoli- Functional unit of the respiratory system Gas Exchange Airways Respiratory bronchioles Alveolar ducts Alveoli (primary gas-exchange unit) Alveolar Capillary Membrane Alveoli Facts Adult lungs contain about 300 million alveoli Alveoli type 1 cells for structure and type II cells for surfactant Surfactant is needed to prevent lung collapse helps alveoli expand during inhalation reduces surface tension at end-expiration Pulmonary capillaries surround the alveoli Alveolar macrophages ingest foreign matter Pulmonary Capillaries Pulmonary Artery (Receives blood from right ventricle) Pulmonary Vein (Blood sent to left atrium) Pulmonary Capillaries Wall has an endothelial layer & thin basement membrane Capillary basement membrane can fuse with alveolar membrane Alveolocapillary membrane Site for gas exchange Made up of alveolar and capillary basement membrane (& both endothelium and interstitial space) Very fragile (blood or plasma could leak into alveolar space) Gas exchange is impaired if any disorder thickens the membrane Chronic Obstructive Pulmonary Disease Disease state characterized by the presence of irreversible airflow limitation due to chronic bronchitis or emphysema (American Thoracic Society) A preventable and treatable disease that’s usually progressive and associated with a chronic inflammatory response. It is not fully reversible. (Global Initiative for Chronic Obstructive Lung Disease, 2011) What’s the biggest risk factor for COPD? 1. 2. 3. 4. Poor ventilation in the home Tobacco smoke Car exhaust fumes Occupational exposure Risk Factors Tobacco smoke (includes environmental tobacco smoke) Indoor air pollution (biomass fuel used in poorly vented dwellings) Occupational dusts and chemicals (irritants, fumes or vapors) Outdoor air pollution (contributes to burden but small effect in causing COPD) Consider COPD whenever a patient has Chronic mucous production History of exposure to risk factors A chronic cough Dyspnea CHAD should be Screened COPD Diagnosis Spirometry test Results must indicate Post-bronchodilator FEV1/FVC <0.70 (confirms that a persistent airflow limitation exists) Spirometry Forced vital capacity (FVC) – the amount of air that is exhaled from full inhalation to full exhalation (shows us the respiratory muscle strength and ventilatory reserve) Forced expiratory volume in the first second (FEV1) – the amount of air that is blown out as hard and fast as possible in the first second of the forced exhalation following full inhalation (is effort dependent) FEV1/FVC shows us airflow obstruction. Peak expiratory flow (PEF) – fastest airflow rate that’s achieved at any time during exhalation In order to establish a diagnosis of COPD the patient would 1. Need to have a chronic cough for at least 3 months 2. Need to have an arterial blood gas done 3. Need to have a spirometry test performed 4. Need to have an abnormal ventilatory rate Chronic Bronchitis The presence of chronic cough Hypersecretion of sputum production Exists for at least 3 months over 2 consecutive years Not always associated with airflow limitation Increased incidence in smokers Major health problem for adults Chronic Bronchitis: Step by Step Irritants increase mucus production (thick and tenacious) Increase in mucus glands and goblet cells Bacteria enjoy sticky coating (allows them to embed and reproduce rapidly) Streptococcus pneumoniae, Haemophilus influenzae Impaired ciliary function Bronchial walls thicken Permanent narrowing of airways Airways collapse in early expiration Gas trapping in distal parts of the lung Tidal volume decreases, hypoventilation and hypercapnia Chronic Bronchitis: Clinical Manifestations Decrease in exercise tolerance (exercise induced hypoxemia) Wheezing SOB May have a smoker’s cough Decreased FEV1 Increase occurrence of pulmonary infections Emphysema Permanent enlargement of gas exchange airways (respiratory bronchioles, alveolar ducts and alveoli = acinus) Alveolar wall destruction (Loss of elastic recoil) One of the many structural abnormalities that could exist in a patient with COPD Emphysema: Alpha Antitrypsin Alpha antitrypsin deficiency (enzyme that inhibits the action of proteolytic enzymes. In the lungs these proteolytic enzymes can destroy lung tissue if unchecked. Individuals with this deficiency who smoke have a greater risk for developing emphysema than those who don’t have the deficiency Emphysema: Step by Step Secondary emphysema usually initiated by cigarette smoke (toxins cause airway epithelial inflammation) Inflammatory cells infiltrate epithelium Cytokines released which increase protease activity (elastases, cathepsins and matrix metalloproteases) Elastin within the septa is broken down by proteases Septal destruction eliminates parts of the pulmonary capillary bed and reduces elastic recoil of airways VQ mismatching and hypoxemia results Air trapping results in chest hyperexpansion & increase work of breathing Emphysema: Clinical Manifestations Dyspnea on exertion Could progress to dyspnea at rest Little coughing and sputum produces Patients are usually thin Tachypnea with prolonged expiration (May note pursed lip breathing) Accessory muscles used AP diameter greater than transverse diameter Percussion note changes to hyperresonant What happens as a result of the loss in airway elastic recoil? 1. It becomes difficult for the patient to exhale and patients need more energy to exhale 2. Volume of air exhaled passively decreases so residual volume increases 3. Alveoli become hyperinflated and bullae (large air spaces in the lung parenchyma) develop 4. All of the above Respiratory Assessment History & Physical Exam Ask the patient if they smoke or if they’ve experienced any chest pain, shortness of breath (dypsnea), wheezing, cough, hemoptysis) If so get the DeTAILS (duration, type, associated factors, influencing factors, location and severity) Note the following Inspect: note chest shape (AP diameter >) Palpate: fremitus decreased with COPD Percuss: hyperresonance Auscultate: adventitious sounds (wheezing or ronchi) Nursing Diagnosis Impaired Gas Exchange r/t alveolar-capillary membrane changes, decreased size of airway, or hypersecretion of mucus, ventilatory muscle fatigue Ineffective Breathing Pattern r/t airway obstruction or decrease in energy Ineffective Airway Clearance r/t fatigue, ineffective cough or hypersecretion of mucus. Imbalanced Nutrition: Less than Body Requirements r/t anorexia or fatigue Activity Intolerance r/t fatigue, difficulty breathing, O2 imbalance Goal Relieve symptoms Improve exercise tolerance Prevent disease progression Prevent exacerbations Reduce mortality Determining Severity of COPD Symptoms- use questionnaires like the COPD Assessment Test Degree of airflow limitation- Use the GOLD Criteria for mild, moderate, severe, very severe (FEV1 > 80% predicted, 50-50, 50-30, less than 30) Risk of exacerbations- increases with increased airflow limitation & hx of previously treated events Comorbidities- osteoporosis, anxiety, skeletal muscle dysfunction, lung ca How is COPD Managed? Quit smoking and encourage tobacco-control policies Emphasize primary and secondary prevention Increase physical activity Bronchodilators (prn or regular basis) Inhaled corticosteroids (FEV1 < 60% predicted) Influenza vaccine recommended annually Pneumococcal vaccine recommended for pts over 65 Mucolytic Agents may be helpful Management Oxygen Therapy Indicated for severe hypoxemia in order to prevent Cor Pulmonale (PaO2 , 55 mmHg) or O2 sat <88 Must be administered carefully if pt has CO2 retention along with severe hypoxemia central chemoreceptors are no longer the primary breathing stimulus. Peripheral chemoreceptors are in charge and they are sensitive to PaO2 changes. If PaO2 exceeds 60mmHg the stimulus to breathe will decrease and the PaCO2 will increase- apnea results. What happens if an adequate oxygenation level can’t be achieved without causing respiratory depression? 1. 2. 3. 4. Patient goes on a ventilator Patient is referred to hospice Patient is given morphine sulfate Patient is given a respiratory stimulant Which of the following statements by a client with COPD suggests that teaching has been effective? 1. “I will get a pneumococcal vaccine every year” 2. “I will perform sedentary activities to prevent disease exacerbation” 3. “I will notify my health care provider if I notice that I’m more short of breath” 4. “I will try to take slow shallow breaths when performing breathing exercises” References Global Initiative for Chronic Obstructive Lung Disease. (2011). Global Strategies for diagnosis, management and prevention of COPD. Retrieved from http://www.goldcopd.org/uploads/users/files/GOLD_Pocket_ May2512.pdf McCance, K. L., Huether S. E., Brashers, V. LO. & Rote, N. S. (2010). Pathophysiology: The biologic basis for disease in adults and children. 6th ed. Missouri: Mosby Elsevier.