CHAPTER 6-2 “Bones Tissue”
advertisement

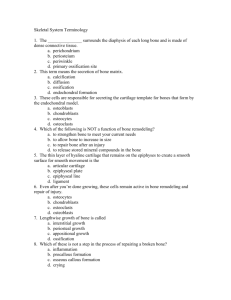
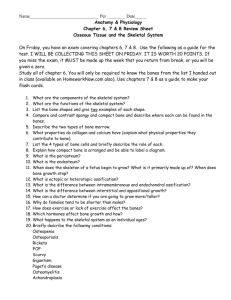
CHAPTER 6-2 Bone Development, Growth and Remodeling Objectives 1. 2. 3. 4. 5. 6. 7. 8. Functions of the skeletal system Classification of bones based on shape General features of bone Bone cells and matrix of bone Compact and spongy bone Bone marrows Bone development Overview of bone growth and remodeling Bone development Ossification or osteogenesis - is the process of forming new bone Two methods of ossification: 1. Endochondral ossification 2. Intramembranous ossification Classification based on formation 1. Endochondral ossification = The process by which bone is formed from hyaline cartilage. 2. Intramembranous ossification = Bone formed by replacing a fibrous membrane and not from cartilage. (ex. Clavicle and skull bones). Endochondral ossification The process by which bone is formed from hyaline cartilage Most bones in the body are formed by this method (including the vertebrae, pelvic bones and limb bones). Consists of 3 sites of ossification. 1. The primary ossification center 2. The metaphysis 3. The secondary ossification center Endochondral ossification During the first 8 weeks of fetal development, hyaline cartilage forms a model of future bone formation. The center (diaphysis) of the cartilage is “primary ossification site” which contains numerous chondrocytes in lacunae. Surrounding the cartilage model is an outer layer chondrocytes called the “perichondrium” which differentiate into “osteoblast cells” and begin to lay down a bony collar around the site. Once the collar is formed the perichondrium becomes periosteum. Endochondral ossification Buds of connective tissue grow from the periosteum into the caritlage and transform the primary ossification site into the primary marrow space. This space is lined with spongy bone. The metaphysis forms between the marrow space and the cartilaginous epiphyseal end. -It is considered as a transitional zone where cartilage is formed into bone at each end of the diaphysis. The metaphysis is just beneath the epiphyseal plate where bone growth continues until after adulthood. The secondary ossification center Begins at the time of birth. Forms in the epiphysis and develops similarly to the primary ossification center. The bone formed in the secondary ossification site persists as spongy bone and growth occurs beneath the outer covering of hyaline cartilage which persists as articular cartilage within the joint cavity on each end of the epiphysis. Endochondral ossification Endochondral ossification Intramembranous ossification Bone formed by replacing a fibrous membrane and not from cartilage. Ex. Skull and clavicle Basic Overview of Process – During the first 8 wks of embryonic development, fibrous connective tissue membranes form in the areas of future flat bones. – Beginning around 8 wks, an “ossification center” forms in the membrane. This center is composed of osteoblasts. – The osteoblasts begin to secrete hydroxyapatite. – The internal spongy bone forms. – The external compact bone forms. Intramembranous ossification Intramembranous ossification Bone Growth Once the cartilage models of embryonic development are replaced by bone, they must continue to grow through infancy, childhood and adolescence. – Increased length: bones continue to lengthen because hyaline cartilage remaining in the epiphyseal plates continues to grow. As adulthood approaches, this cartilage becomes less active and is eventually replaced by bone. Epiphyseal plate growth zones 1. 2. 3. 4. 5. Consists of five distinct zones: Zone of resting cartilage Zone of cartilage proliferation Zone of cell hypertrophic cartilage Zone of calcified cartilage Zone of ossification Epiphyseal plate growth zones Bone growth Appositional growth - Increased Width: bones continue to widen as osteoblasts form more layers of bone around the outside and osteoclasts break down some of the bony matrix inside. Why would bone need to be broken down inside as it grows outside? Appositional growth Control of Bone Growth Bones increase in length and width because of the influence of minerals, vitamins, and hormones in the body. Calcium and phosphate are necessary for calcification Vitamins A, C and D promote bone growth. The specific hormones which affect growth are growth hormone (GH), thyroid hormone (T3 and T4), and the sex steroids (estrogen and testosterone). Chemicals important in bone homeostasis Bone remodeling Even though the bones in an adult do not continue to grow as described above, they are constantly being remodeled. This means that bone is always being broken down by osteoclasts and reformed by osteoblasts (really no different from remodeling ones home). Each week we turn over about 5% of our bone mass. Control of Remodeling Two major factors influence remodeling. Calcium levels - our bodies need a homeostatic level of calcium in the blood for all cells to function properly. Mechanical stress - the varied activities of life put different stresses on each bone as we age, which requires slight adjustments to compensate for these stresses. Bone blood supply Bone is very vascular and well nourished by blood. Bone fractures Bone fractures Types of bone fractures Simple fractures do not break the skin. Compound fractures puncture the skin and are at great risk of infection. Bone fracture repair There are four primary stages for bone repair after a fracture. Bone fractures