Sex ed and hiv: nuts and bolts
advertisement

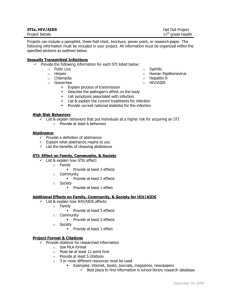
SEX ED AND HIV FRAMEWORK: THE NUTS AND BOLTS 11/17/15 Lisa Jo Gagliardi, MPA lisajo@eupschools.org Agenda 9:30am: Data-Driven decisions about teaching reproductive health and choosing curriculum 10:00am: Curriculum Selection and Best Practices 12:00pm: Lunch 12:30pm: The Law-What you need to know to teach Reproductive Health 2:00pm: Parent Involvement Resources/best practices 2:30pm: Content Update on Sex Offenses 3:15 pm: Content updates in HIV/AIDS and other STIs 4:00pm: Adjourn • Name • School/grades • Why did you come to this training? What are you hoping to learn? WORKING AGREEMENTS NO KILLER COMMENTS-REPRODUCTIVE HEALTH CAN BE A SENSITIVE SUBJECT. NO JUDGING-WE WILL BE DOING A LOT OF DISCUSSION /GROUP WORK TODAY AND WANT PEOPLE TO FEEL SAFE. NO RABBIT HOLES-WE WILL TRY TO REFRAIN FROM GOING DOWN RABBIT HOLES THAT TAKE US AWAY FROM OUR LEARNING OBJECTIVES. USE “I” MESSAGES-WHEN SPEAKING ABOUT YOURSELF AND YOUR OWN THOUGHTS AND FEELINGS. WHAT ARE SOME THINGS YOU THINK WE SHOULD MAKE AS GROUND RULES FOR TODAY? GOAL Provide teachers/other constituents with the basics of curriculum selection, instruction and the law, as well as updates for teaching sexuality and HIV and STD education Objectives • Understand the standards of best practice teaching in HIV and sexuality education. • Increase your comfort level for teaching HIV and Sex Ed. • Understand current trends in youth behaviors and how HIV and sex education can impact those trends. • Understand Michigan School Code requirements. • Identify ways of reaching parents on HIV and sex education. • Identify and utilize local, state, and national HIV and sexuality education resources. Please note: This training is meant to keep educators up to date, comfortable and equipped to teach reproductive health and HIV/AIDS. It is required every 5 years for HIV This is not an endorsement for a teaching certificate, and has no baring on whether you are “highly qualified” to teach reproductive health… that is a teaching certification/endorsement issue. HIV/AIDS: Teacher (no specific endorsement needed), or a health professional. Both must go through training with the Regional School Health Coordinator once every 5 years. Sex Education (including Puberty): Qualified to teach health (§380.1507). All subjects for elementary classroom teachers. Secondary level, must have either the MA (health), MX (health, physical education, recreation and dance), or KH (family and consumer science) endorsement. A HS Health Teacher cannot teach 5th grade puberty (unless K-12 MA, MX or KH endorsement) PE is NOT a Health Ed. endorsement. Ongoing professional development for teachers is strongly recommended. The Office of Professional Preparation Services at MDE accepts applications from districts for full-year permits that allow certified teachers to teach without the required endorsements, while pursuing coursework toward earning the endorsement. HEALTH STANDARDS and Reviewing GLCEs and MMC www.eupschools.org ->Programs -> Health Ed. Looking at Data. What we think vs. what is known TRUE FALSE About 52% of Michigan high school students have had sex in their lifetime True False- 38.1% according to 2013 Michigan YRBS False About 25% of Michigan high school students have had sexual intercourse in the past 3 months True TRUE- 26% according to 2013 Michigan YRBS False 55% of Michigan high school students that have had sex in the past 3 months, did so under the influence of drugs or alcohol True FALSE- 21% according to 2013 Michigan YRBS False Of high school students who had sexual intercourse in the past 3 months, 25% used a condom True FALSE- 61% according to 2013 Michigan YRBS False 8% of Michigan high school students, who have had sexual intercourse, have had 4 or more partners in their lifetime True TRUE- according to 2013 Michigan YRBS False Michigan high school boys are more sexually active than girls True FALSE- there is no statistically significant data to support this False ABSTINENCE-BASED V. ABSTINENCE ONLY Abstinence -ONLY Abstinence-Based (aka Abstinence+) Only can talk about abstaining from sexual intercourse. Abstinence is taught as the only 100% safe choice. Risk reduction is taught. The degree of risk reduction taught is up to the Sex Ed. Advisory and guided by the curriculum chosen (i.e. condoms, birth control, oral protection, etc…) Is your school Abstinence-Only or AbstinenceBased? What are the pros and cons to each? LET’S TALK CURRICULUM See the “Curriculum Evaluation Tool” hand-out Processing the Curriculum Evaluation Tool ■Please get into a group of 4 Processing the Curriculum Evaluation Tool ■Let’s read the first page silently Processing the Curriculum Evaluation Tool ■Now, in groups of 4, count off 14 ■Each person grab 3 sticky notes. Processing the Curriculum Evaluation Tool ■You are assigned to your section… #1 take section 1, #2 take section 2, etc… Processing the Curriculum Evaluation Tool Read your assigned section silently. On your sticky notes: 1. Write a word that stands out 2. Write a phrase that stands out 3. Write a sentence that stands out. Processing the Curriculum Evaluation Tool ■Now dialogue with your quartet about why you chose the: 1. Word 2. Phrase 3. Sentence Be prepared to share out from your group 10 Characteristics of Effective Curricula -1focus on reducing one or more sexual behaviors that lead to unintended pregnancy or HIV/STD infection. 10 Characteristics of Effective Curricula -2based upon theoretical approaches demonstrated to be effective in influencing other health-related risky behaviors 10 Characteristics of Effective Curricula -3give a clear message, and continually reinforce that message. 10 Characteristics of Effective Curricula -4- provide basic, accurate information about the risks of unprotected intercourse and methods of avoiding unprotected intercourse. 10 Characteristics of Effective Curricula -5Includes activities that address social pressures on sexual behaviors. 10 Characteristics of Effective Curricula -6Provides modeling and opportunities to practice communication, negotiation, and refusal skills. 10 Characteristics of Effective Curricula -7Employs a variety of teaching methods, designed to involve participants and personalize the information. 10 Characteristics of Effective Curricula -8Incorporates behavioral goals, teaching methods, and materials that are appropriate to the students' age, sexual experience, and culture. 10 Characteristics of Effective Curricula -9Lasts a sufficient length of time to adequately complete important activities. 10 Characteristics of Effective Curricula -10Has teachers or peer educators who believe in the program and are provided appropriate training to deliver the curriculum INSTRUCTION BEST PRACTICES What is Skills-based Instruction - explains the skill - models the skill - guides practice - personalizes the use of the skills. Why is Skill-Based Learning Important? Adapted Health Belief Model The most important predictors of current and future health status Behaviors Facts to make responsible decisions Abilities to act in healthy way Skills Understanding severity Risks and benefits Self-Efficacy Environmental Support Peers, school, home, community support and reinforcement for healthy behaviors. Belief that one can use the skills to change life Typical Practice Behavior change unlikely Skills Self-Efficacy Environmental Support SKILLS -Showing that they can Analyze Influences -Exhibiting the ability to Access Information -Practicing Interpersonal Communication skills -Demonstrating Decision-making skills -Demonstrating goal-setting skills to enhance health. -Practicing health-enhancing behaviors and avoid or reduce health risks. -Advocating for personal, family and community health. Does your puberty/sex ed or HIV curriculum use skillbased instruction currently? Why do you think is it important to teach skills-based? THE LAW FOR HIV AND SEX ED Also reviewing Sex Ed. Advisory Board requirements and 2 year reports Where to find the laws Key to Compiled Laws Regarding HIV/STD and Sex Education MCL No. Public Act Last Action 380.1169 School Code Amended 6/04 380.1506 School Code Amended 11/77 380.1507 School Code Amended 6/04 School Code School Code Added 7/96 Amended 6/04 388.1766 State Aid Act Amended 7/96 388.1766a State Aid Act Added 6/04 380.1507a 380.1507b Focus Dangerous communicable diseases; human immunodeficiency virus infection and acquired immunodeficiency virus infection; teacher training; teaching materials; curricula; teaching of abstinence from sex. Program of instruction in reproductive health; supervision; request to excuse pupil from attendance; “reproductive health” defined. Instruction in sex education; instructors, facilities, and equipment; stressing abstinence from sex; elective class; notice to parent or guardian; request to excuse pupil from attendance; qualifications of teacher; sex education advisory board; public hearing; distribution of family planning drug or device prohibited; “family planning,” “class,” and “course” defined. Notice of excuse from class; enrollment. Sex education and instruction; curriculum requirements. Dispensing or distributing family planning or drug or device, dispensing prescriptions for family planning drug, or making referrals for abortion; forfeiture. Instruction in reproductive health or other sex education; complaint process. Mandated HIV and allowable Sex Ed. This means that you must teach HIV/AIDS at each building level (elementary, middle and High School) This part of the law also says that Sex Ed is optional and allowable Sex Ed. Advisory Board Every district that chooses to implement sex education must have a sex education advisory board. School board sets terms of service, number of members, and a membership selection process ■ must include: parents, pupils, educators, local clergy, and community health professionals--At least half of the members must be parents. A majority of those parent members must not be employed by a school district. ■ Members must be given two weeks written or electronic notice of meetings Sex Ed. Advisory Board-ROLE Establishing program goals and objectives Reviewing and recommending materials and methods to the board, taking into consideration the district’s needs, demographics, and trends including, but not limited to: teenage pregnancy rates, STI rates, and incidents of sexual violence and harassment. Evaluating, measuring, and reporting the attainment of program goals and objectives and Sex Ed. Advisory Board-MEMBERS Sex Ed. Supervisor; usually a Superintendent, Principal or School Health Professional. 2 co-chairs for the advisory. One must be a parent, and one is a school person. ½ Advisory must be “pure parents”. The board of a school district shall include pupils of the school district, educators, local clergy, and community health professionals on the sex education advisory board. Sex Ed. Advisory Board-Definition of Sex Education It’s useful to develop or adopt a definition of sex education that aligns with existing definitional language in the law. Sex Ed. Advisory Board-Curricula Approval Curricula that are used as a part of HIV/STI or sex education instruction must go through the formal approval process, including two public hearings and school board approval. Curricula Approval Factors Curricula, materials, and methods must be approved in advance regardless of the: class in which it is taught (e.g., health class, schoolwide assembly, English class); person providing the instruction (teacher, school nurse, guest speaker) time of day the instruction is offered (during the school day versus after school); or place the instruction takes place (within the building versus off the school premises). Prohibited Content and Actions Ensure pupils are not taught in a way that condones the violation of laws of this state including, but not limited to: those relating to sodomy, indecent exposure, gross indecency, and criminal sexual conduct in the first, second, third, and fourth degrees. Clinical abortion cannot be considered a method of family planning, nor can abortion be taught as a method of reproductive health. A person cannot dispense or otherwise distribute a family planning drug or device in a public school or on public school property. Model Curricula-Michigan Model for Health 7-8 grade HIV/AIDS/STI: Qualifies as HIV/AIDS curriculum. 9-12 Healthy and Responsible Relationships (covers sex. Ed and HIV/AIDS and STI). Elementary Teachers attending today’s HIV/AIDS/STIs training will be considered trained for elementary All of the above are FREE to you thanks to our State grant, and we can train you in them. Other curricula that is good Puberty: the Wonder Years: good for grades 4-6th. (can train, cannot pay for curriculum) F.L.A.S.H.: Free online curricula for pubertyH.S. Sex Ed. Has a Special Education curricula too. (It is Free. Not equipped to train in it) Healthy Sexuality, from RMC Health: good for grades 6-8. ($200. Not equipped to train in it. Need to add in Michigan Law pieces.) Other curricula There are many other good curricula out there. Be sure to use the Curriculum Evaluation Tool when reviewing a new curriculum. Parental Rights and Exclusion from Instruction Parents have The Right to know the content of the instruction. The right to review materials in advance. The right to observe instruction. The right to excuse their child without penalty Parent Complaint Process person can file a complaint with the superintendent or chief administrator of the district or ISD in which the pupil is enrolled.. If the parent is not satisfied with the investigation or findings made by the superintendent, the parent can appeal the findings to the ISD in which the district is located. If the parent is not satisfied with the investigation or findings they can appeal the findings to the MDE. PENALTIES! If an investigation conducted by MDE reveals that one or more violations of the Revised School Code or State School Aid Act, the district or ISD shall forfeit an amount equal to 1% of its total state school aid allocation. A district in which a school official, member of a board, or other person dispenses or otherwise distributes a family planning drug or device, dispenses prescriptions for any family planning drug, or makes referrals for abortions shall forfeit 5% of its total state aid appropriation. Sex Ed. must include A-K of the law (Law 380.1507b) See A-K curriculum Checklist for next activity. You will be assigned a Letter. You will present your letter of the law with a visual presentation. Use the chart paper and markers supplied. You have 15 minutes. Example A). Discuss the benefits of abstaining from sex until marriage and the benefits of ceasing sex if a pupil is sexually active. NO. I do not want to have sex STOP HIV/AIDS & STI Looking at Data. What we think vs. what is known. True False CHLAMYDIA ACCOUNTS FOR MOST SEXUALLY TRANSMITTED INFECTIONS IN THE OUR REGION. True TRUE-according to MDHHS False HIV/AIDS SHOULD BE TAUGHT AT EVERY BUILDING LEVEL (ELEMENTARY, MIDDLE AND HIGH SCHOOL) True TRUE-Per Michigan School Code False HIV/AIDS CURRICULUM MUST BE APPROVED BY THE SCHOOL BOARD, BUT DOES NOT HAVE TO GO THROUGH THE SEX EDUCATION ADVISORY COMMITTEE True TRUE-Sex education must go through the advisory False HIV-AIDS abstinence only has to go through the School Board MICHIGANDERS, AGES 15-24 YEARS, ACCOUNT FOR 75% OF ALL CHLAMYDIA CASES True True- according to MDHHS False IN MICHIGAN, 64% OF ALL GONORRHEA CASES ARE FOUND IN 24-29 YEAR OLDS True FALSE- It is actually 15-24 year olds, according to MDHHS False What Is AIDS? A = Acquired: Something that you get from someone who is infected I = Immune: Refers to body’s defense system D = Deficiency: A lack of S = Syndrome: A collection of diseases or malignancies What is HIV? H = Human Something that you get from someone who is infected I = Immunodeficiency Refers to the breakdown in the body’s defense system V = Virus a sub-microscopic infectious agent Window Period Defined as the point of infection to the development of enough antibodies to be detectable on a test… Timeframe for testing HIV antibody positive: Most people will develop detectable antibodies within 2-8 weeks (the average is 25 days). 97% by 3 months Stages of HIV Infection Acute HIV Infection Asymptomatic Chronic Symptomatic Advanced HIV Disease (AIDS) Acute HIV Infection A person newly infected with HIV may experience some initial temporary symptoms including: Fever Fatigue Red rash Headache Sore throat Muscle pain Swollen lymph nodes Vomiting Upset stomach Asymptomatic HIV Disease Period of no symptoms Longest stage of HIV infection. Most people will experience no symptoms for 5-10 years (or longer) 95% of persons infected will progress to experiencing symptoms at some point Chronic Symptomatic Stage Signs/symptoms include: Fatigue Swollen lymph nodes Fever/night sweats Weight loss Diarrhea Neurological symptoms Respiratory problems Unusual skin conditions Severe headaches Chronic generalized pain Thrush Chronic Symptomatic Stage Signs in Women: Persistent vaginal yeast infections Pelvic inflammatory disease (PID) Cervical abnormalities Invasive cervical cancer is an AIDS defining illness Menstrual irregularities Advanced HIV Disease (AIDS) CDC AIDS Case Definition: To be diagnosed with AIDS, a person must have: Evidence of HIV infection and at least one of the following: A CD4+ count below 200 (normal CD4+: 800-1200) OR Has been diagnosed with one or more of the 26 AIDS defining conditions 26 AIDS Defining Conditions A few of the most common: • KS: Kaposi’s Sarcoma • PCP: Pneumocystis carinii pneumonia • Toxo: Toxoplasmosis • Thrush: esophageal candidasis • TB: Tuberculosis • CMV: Cytomegalovirus • HIV encephalopathy: AIDS-related dementia Point of Infection Stages of HIV Disease Immune Strength Antibody Levels Viral Load Acute Asymptomatic Chronic Symptomatic Advanced HIV Infection HIV Disease HIV Disease HIV Disease (AIDS) What are the 5 bodily fluids that can transmit HIV? Body Fluids Known to Transmit HIV Blood Semen Vaginal/cervical fluids Breast milk Any body fluids containing blood [Cerebrospinal fluid, fluid surrounding a fetus, fluid surrounding joints] Formula for Assessing Risk Risk is related to: • Which body fluid • Route of entry into the body • Dose of infected fluid • How long fluid is out of body • Number of exposures • Condition of host • Condition of recipient No Casual Spread Can’t be spread through: Hugging Touching Using a public toilet Utensils OTHER Behaviors that can Transmit HIV Behaviors related to Birth (Perinatal Transmission) From mother to baby, transmission can occur: • During the birthing process • Through breast feeding Types of Testing Anonymous Client tested with number Confidential Client tested with name & other identifiers Blood Oral fluid ■ Most common HIV test is the antibody screening test- looks for the antibodies that your body makes against HIV. Can be in a lab or as a rapid test at the testing site. Performed on blood or oral fluid (not saliva). Because the level of antibody in oral fluid is lower than it is in blood, blood tests tend to find infection sooner after exposure. Most blood-based lab tests find infection sooner after exposure than rapid HIV tests. ■ Some tests detect both antibodies and antigen (part of the virus itself). These tests can find recent infection earlier than tests that detect only antibodies. These antigen/antibody combination tests can find HIV as soon as 3 weeks after exposure to the virus, but they are only available for testing blood, not oral fluid. Not all testing sites offer this test by default. ■ The rapid test is an immunoassay used for screening, and it produces quick results, in 30 minutes or less. Rapid tests use blood or oral fluid to look for antibodies to HIV. If an immunoassay (lab test or rapid test) is conducted during the window period (i.e., the period after exposure but before the test can find antibodies), the test may not find antibodies and may give a false-negative result. ■ Follow-up diagnostic testing is performed if the first immunoassay result is positive. Modes of Testing OraSure (collection of oral mucosal transudate-OMT) Dried Blood Spot (Clinic collection finger stick) Clearview (15 min rapid testing) Traditional Blood Draw Global Impact Estimated 35 million people living with HIV and AIDS in 2013 3.2 million were <15 years old) 2.1 million new infections occurred in 2013 HIV is the world’s LEADING INFECTIOUS KILLER Michigan Data on HIV/AIDS ■ Estimated 19,800 people living with HIV in Michigan as of January 2013. ■ Below is the 5 year trend from 2008-2012 Michigan Data on HIV/AIDS ■ The number and rate of new HIV diagnoses in Michigan remained stable between 2008 and 2012, with an average of 809 new cases per year and an average rate of 8.2. ■ The highest rates of new HIV diagnoses occurred among: – 20 - 24 and 25-29 year olds – Black males and females – Men who have sex with men (MSM)* – Southeast Michigan residents ■ INCREASES in rates occurred among: – 20 - 24 year olds (4th consecutive trend report) ■ Almost three quarters of Michigan’s new cases among 13 - 24 year olds were residents of SE Michigan at diagnosis. What other skills or concepts, besides preventing this specific infection/disease, might we want to teach when teaching HIV/AIDS? What other skills can we teach kids when they are learning about HIV? PREVIEWING A VIDEO Understanding HIV & AIDS Accessing Videos and other resources on our website! www.eupschools.org ->Programs -> Health Education STIs Sexually Transmitted Infections CDC has great fact sheets on STIs (STDs) here: http://www.cdc.gov/std/healthcomm/fact_sheets.htm Michigan STI Surveillance http://www.mdch.state.mi.us/pha/osr/Index.asp?Id=12 Why STI not STD??? ■ STI stands for sexually transmitted infection. – The medical community has begun transitioning from “STD” to “STI” to clarify that not all sexually transmitted infections turn into a disease. – For instance, the vast majority of women who contract the VIRUS HPV (human papilloma virus) will not develop the resulting disease cervical cancer. – Nevertheless, currently you will still see STI and STD used interchangeably. Types Of STI’s ■ Bacterial Infections: Infections caused by bacteria that can be cured. – Chlamydia, Gonorrhea, Syphilis ■ Viral Infections: Infections caused by a virus that can be treated. – HBV, HCV, HPV, HIV ■ Parasitic Infections: Infections caused by tiny organisms that can be cured. – Trichimoniasis Chlamydia Symptoms ■ Females – NONE – Low abdominal pain – Bleeding between periods or after intercourse – Painful intercourse – Creamy discharge ■ Males – NONE – Clear, creamy, or milky discharge – Burning or irritation with urination ■ Newborns – pneumonia – ophthalmia Chlamydia Fast Facts ■ Most common reportable disease in the US ■ Highest age specific rates by gender Females: 15 - 19 year old Males: 20 - 24 year old ■ “Silent” Disease: 75% of women have no symptoms 50% of men have no symptoms ■ Complications – Infertility from PID in women – Infertility from Epididymitis in men ■ Increases transmission/acquiring of HIV Chlamydia Statistics 1,422,976 chlamydial infections were reported to CDC for all 50 states and the District of Columbia ~CDC 2010 48,505 in Michigan as of 2013 ~MDHHS Leading STI our region for 15-24 year olds Gonorrhea Symptoms ■ Females – NONE – Creamy, yellowishgreen discharge – Burning or irritation when urinating – Low abdominal pain – Painful intercourse ■ Males – NONE – Creamy or yellowish-green discharge – Pain, burning or tingling sensation when urinating – Painful or swollen testicles ■ Newborns – Ophthalmia Gonorrhea Fast Facts ■ Highest age specific rates by gender – Females:15-19 year old – Males: 20-24 year old – 75% cases in 15-29 years old ■ 50% of women have no symptoms ■ Complications – Infertility from PID in women – Infertility from Epididymitis in men ■ Increases transmission/acquiring of HIV Gonorrhea Statistics ■ In Michigan, 67% of all Gonorrhea cases are from 15-24 year olds ■ In 2012, 334,826 cases were reported – CDC ■ In 2014, 9,666 cases in Michigan. – MDHHS Syphilis Symptoms Primary: 10-90 day incubation period Painless sore Secondary: 6 weeks-6 months incubation period Rash all over; sores, especially on palms of hands and feet Tertiary: > 1 year (latent) Damage to heart, central nervous system; paralysis; death Syphilis ■ Highest age specific rates by gender – Females: 20-29 year old – Males: 20-29 year old ■ Untreated early syphilis during pregnancy – Resulted in perinatal death in up to 40% of cases – If acquired during four years pre-pregnancy may lead to infection of the fetus in over 80% of cases ■ Increased transmission/acquiring of HIV Syphilis Statistics In Michigan, the largest percentage of cases are in 30-44 year old category In 2012, there were 14,503 cases reported in the U.S. ~ CDC 1,116 in Michigan ~MDHHS Herpes Symptoms ■ Transmission – vaginal, oral, anal sex ■ 2-20 day incubation period. ■ Flu-like feelings. ■ Painful sores or blisters on the sex organs or mouth lasting 1-3 weeks, but may recur periodically. ■ Itching, tingling or burning before blisters appear. Genital Herpes Statistics ■ 45 million people in the United States ages 12 and older infected ■ 1 in 6 sexually active adolescents and adults infected ■ 1 in 5 sexually active women infected ■ Most people who have genital herpes don't know it because they never have any symptoms Human Papiloma Virus (HPV) Statistics ■ Most common STI ■ 20 million people are currently infected with HPV ■ 6 million Americans get a new genital HPV infection each year ■ More than 100 different strains or types of HPV ■ Over 40 types are sexual HPV ■ 50% sexually active people will acquire genital HPV at some point in their lives. ■ “High-risk” types of HPV may cause abnormal Pap tests ■ “Low-risk" types of HPV may cause mild Pap test abnormalities or genital warts HPV and Cancer ■ HPV can cause cervical and other cancers including cancer of the vulva, vagina, penis, or anus. It can also cause cancer in the back of the throat, including the base of the tongue and tonsils (called oropharyngeal cancer). ■ Cancer often takes years, even decades, to develop after a person gets HPV. The types of HPV that can cause genital warts are not the same as the types of HPV that can cause cancers. ■ There is no way to know which people who have HPV will develop cancer or other health problems. People with weak immune systems (including individuals with HIV/AIDS) may be less able to fight off HPV and more likely to develop health problems from it. The World of HPV ■ HPV (the virus): About 79 million Americans are currently infected with HPV. About 14 million people become newly infected each year. HPV is so common that most sexually-active men and women will get at least one type of HPV at some point in their lives. ■ Health problems related to certain types of HPV include genital warts and cervical cancer. ■ Genital warts: About 360,000 people in the United States get genital warts each year. ■ Cervical cancer: More than 11,000 women in the United States get cervical cancer each year. ■ In most cases, most kinds of HPV go away on its own and does not cause any health problems. But when HPV does not go away, it can cause health problems like genital warts and cancer. ■ Genital warts usually appear as a small bump or group of bumps in the genital area. They can be small or large, raised or flat, or shaped like a cauliflower. A healthcare provider can usually diagnose warts by looking at the genital area. Genital Warts (HPV) ■ Types 16, 18, 31, 33, and 35 – Related to cervical cancer ■ Type 16 accounts for more than 50% ■ Types 16, 18, 31 and 45 account for 80% – Cause Pap smear abnormalities ■ Types 6 and 11 – Cause genital warts – Cause recurrent respiratory papillomatosis in infants (STD Surveillance 2010) MDE TOT October 12, 2009 Genital Warts (HPV) ■ Transmission: – Direct skin to skin contact during vaginal, anal or possible oral sex ■ Symptoms: – May be asymptomatic – Small, bumpy, cauliflower growths on the sex organs, throat or anus – Itching or burning around the sex organs ■ 4-6 weeks to 9 month incubation period What To Do if Exposed to an STI ■ Seek health care provider for exam, testing, and treatment ■ Stop having sex until you and your partner are treated and have finished all medication ■ Notify partner ■ Get tested for HIV Risk Reduction from STIs ■ Abstinence from sex & needles is only PREVENTION. ■ Have sex with only one partner who only has sex with you. ■ Avoid using alcohol and other drugs. ■ Talk to your partner about past sex partners. ■ Correct, consistent use of condoms, dental dams, and female condoms. Treatment ■ Get tested, tell partner if you think you may have or were exposed to an STI ■ Entire dose of medication must be taken to completely treat the STI ■ Avoid sex for duration of treatment and 5 to 7 days after or as directed ■ Do not take anyone else’s prescription medication QUESTIONS/COMMENTS? LISA JO GAGLIARDI REGIONAL SCHOOL HEALTH COORDINATOR lisajo@eupschools.org (906) 632-3373 ext. 132