Schizophrenia Outline
advertisement

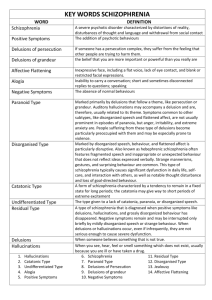
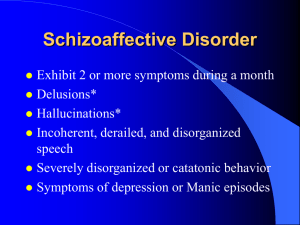
Schizophrenia 3/5/10 (Moceo) Defined as: o Schizophrenia - a syndrome or disease process of the brain causing distorted and bizarre thoughts, perceptions, emotions, movements, and behavior DSM IV Diagnostic Criteria o Delusions o Disorganized speech o Disorganized or catatonic behavior o Signs of disturbance for at least 6 months o Hallucinations o Negative symptoms o Social/occupational dysfunction o Signs/symptoms not associated with general medical disorder or substance abuse Symptoms of Schizophrenia o Positive (or hard) symptoms include: Remember that positive symptoms that normally wouldn’t be there… I’m positive you’re signs are of schizophrenia Delusions Hallucinations Grossly disorganized thinking, speech and behavior o Negative (or soft) symptoms include: Remember that negative symptoms are things that a normal person would normally have. N for normal, N for negative. A normal person has them and your test comes back negative for these Flat affect – they have a very blah kind of mood Avolition – unable to initiate goal directed activity. They neither have the desire or the ability to do these things… Apathy – may not care about anything at all. They are indifferent Alogia – speaking very little. May not have a whole lot of meaning when they do speak Social withdrawal Social discomfort Types of Schizophrenia o Paranoid type: persecutory or grandiose delusions and hallucinations; sometimes excessive religiosity; hostile and aggressive behavior o Disorganized type: grossly inappropriate or flat affect, incoherence, loose associations, extremely disorganized behavior o Catatonic: marked psychomotor disturbance, motionlessness, or excessive motor activity; extreme negativism; mutism; peculiarities of voluntary movement (echolalia - when they repeat a word you say over and over and over and over and over… haha, echopraxia - when they repeat everything you just said). May have waxy flexibility – they sit in the same position for hours and you go up and move their fingers into a peace sign or whatever and they keep the peace sign for hours and hours o Undifferentiated: mixed schizophrenic symptoms along with disturbances of thought, affect, and behavior o Residual: at least one previous psychotic episode but not one currently; social withdrawal, flat affect, loose associations o Remember, most schizophrenics will exhibit signs of all of these, so don’t get too focused on trying to separate them Clinical Course o Most patients experience a slow and gradual onset of symptoms o Younger age of onset associated with poorer outcomes Because it’s progressive! Each time you have an exacerbation you may not ever return to that level of functioning you were at before the exacerbation. Say they could tie their shoes, they have an episode, and then for the rest of their life they can’t. o In first years after diagnosis, patient may have relatively symptom-free periods between psychotic episodes or fairly continuous psychosis with some shift in severity of symptoms Really common to diagnose during college years (maybe stress, drugs, whatever) o Most patients with schizophrenia have difficulty functioning in the community and few lead fully independent lives o Early detection and aggressive treatment of the first psychotic episode improves outcomes Related Disorders o Schizophreniform disorder: symptoms of schizophrenia are experienced for less than the 6 months required for a diagnosis of schizophrenia Schizophreniform disorder is characterized by the same features as schizophrenia. The only exception is the duration of the symptoms, at least one month but less than six months. The diagnosis is changed to schizophrenia if the clinical picture lasts longer than six months. o Schizoaffective disorder: symptoms of psychosis and thought disorder along with all the features of a mood disorder (basically you have schizophrenia and bipolar stuff along with it, maybe mood disorder along with it) Schizoaffective disorder is manifested by schizophrenic behaviors and symptoms associated with either manic or depressive mood disorders. Depression is exhibited with psychomotor retardation and suicidal ideation. Mania is characterized by euphoria, grandiosity, and hyperactivity. The decisive factor, however, is the presence of characteristic schizophrenic symptoms, such as prominent delusions and hallucinations along with a dysfunctional mood. o Delusional disorder: one or more non-bizarre delusions with no impairment in psychosocial functioning Delusional disorder is characterized by the presence of systematized, nonbizarre delusions accompanied by affect appropriate to the delusion. The delusion my preoccupy and dominate the patient’s life. o Brief psychotic disorder: at least one psychotic symptom lasting 1 day to 1 month; may or may not have an identifiable stressor, such as childbirth o Shared psychotic disorder (folie `a deux): similar delusion shared by two people, one of whom has psychotic delusions Predisposing factors o Exact cause is still unknown o Most likely result of combination of factors: Biological Chemicals, virus or illness, degenerative changes in the brain. Rule out stroke, Huntingtons, alcohol abuse Psychological Environmental Toxins, living in crowded, poor, unsanitary conditions, abusive conditions Cultural Considerations o Ideas that are considered delusional in one culture may be commonly accepted by another culture o Auditory or visual hallucinations may be a normal part of religious experiences in some cultures o Ethnicity may be a factor in the way a person responds to psychotropic medications Asians usually need lower doses of these meds Treatment o Primary treatment involves antipsychotic (neuroleptic) medication o Conventional antipsychotics target the positive signs: Delusions Hallucinations Disturbed thinking Other psychotic symptoms have no observable effect on the negative signs Conventional (typical) antipsychotic review o o o o Haldol Loxitane Mellaril Moban Navane Prolixin Stelazine Thorazine With these you have a higher risk of extrapyramidal symptoms. Give them Cogentin, Artane, sometimes Benadryl or Semetral to combat these EPS Atypical antipsychotics diminish positive symptoms, and they lessen the negative signs: Avolition Social withdrawal Anhedonia – lack of pleasure May get a better response if conventionals are not working, these are the newer drugs Atypical antipsychotic review: Abilify Clozaril – remember agranulocytosis and need for CBC Geodon Invega Risperdal Seroquel Zyprexa Maintenance Therapy Antipsychotics available in depot injection forms for maintenance therapy: Prolixin decanoate (Fluphenazine decanoate) Haldol decanoate (Haloperidol decanoate) Risperdal Consta (Risperidone) The effects of the medications last from 2 to 4 weeks, eliminating the need for daily oral antipsychotic medication Side effects of Antipsychotic Medications Neurologic side effects: Extrapyramidal side effects (acute dystonic reactions, akathisia, and parkinsonism) Tardive dyskinesia Seizures Neuroleptic malignant syndrome Non-neurologic side effects: Weight gain Sedation Photosensitivity Anticholinergic symptoms Orthostatic hypotension Agranulocytosis (Clozaril) Psychosocial Treatment Group therapies Supportive, medication management, use of community supports o Sometimes those groups can get really old, they hear the same things over and over. Could also be because of lack of motivation or the fact that most of the time their Givea-Shit is broken… Social skills training o o Cognitive adaptation training Cognitive enhancement therapy (CET) Computerized training where they can make an avatar or whatever make decisions for them without having to be the actual person doing that in a real life setting. Family therapy But sometimes their families are already fed up with their bullshit and aren’t willing to participate Family education Application of the Nursing Process o Assessment Previous history with schizophrenia Previous suicidal ideation Current support system Patient’s perception of current situation Want to know this because maybe they don’t know why they are being admitted or don’t understand what they did wrong. Could help you find out what’s going on in their life, the stressors, the breaking points. If you don’t know what their perception is you won’t be able to treat them effectively General appearance, motor behavior, and speech Mood and affect: flat or blunted affect, anhedonia Thought processes and content: disordered Delusions Sensorium and intellectual processes: hallucinations, disorientation, concrete or literal thinking Judgment and insight: impaired judgment, limited insight Self-concept: may be distorted, with depersonalization, loss of ego boundaries resulting in bizarre behaviors Roles and relationships: often socially isolated, have difficulty fulfilling life roles Physiologic and self-care considerations: may have multiple self-care deficits (inattention to hygiene, nutrition, sleep needs, polydipsia occasionally seen in longer-term patients) o Data Analysis Common nursing diagnoses for positive symptoms include: Risk for suicide Risk for other-directed violence Disturbed thought processes Disturbed sensory perception Disturbed personal identity Impaired verbal communication Common nursing diagnoses for negative symptoms and functional abilities include: Self-care deficits Social isolation Deficient diversional activity Ineffective health maintenance Ineffective therapeutic regimen management o Outcome Identification Expected outcomes for the acute, psychotic phase; the patient will: Not injure self or others Establish contact with reality Interact with others Express thoughts and feelings in a safe and socially acceptable manner o o Participate in prescribed therapeutic interventions Expected outcomes for continued care; the patient will: Participate in the prescribed regimen Maintain adequate routines for sleeping, food and fluid intake Be independent in self-care activities Communicate effectively with others in the community to meet needs Will seek or accept assistance to meet needs when indicated Interventions Promote safety of patient and others Establish therapeutic relationship Use therapeutic communication Interventions for delusional thoughts If they come up to you and tell them “Rats are eating my brain,” what do you do? You already have the therapeutic relationship with them enough for them to come to you, you may want to tell the dr. Obviously their med isn’t working and you need to tell the dr. This may not break the trust they have in you because maybe they are telling you so that you will go and tell the dr. She said there wouldn’t be a question like this in the test, but I added it in incase anyone wanted it Interventions for hallucinations Protect the patient who has socially inappropriate behaviors Say if they are dancing naked in the hallway, try and maybe get them out of the way of other people, in a nice and calming way. They may not know what they are doing and might be embarrassed later on when they come out of the delusion or whatever Patient and family teaching Remain calm anxiety is contagious Be consistent increases trust Keep promises increases trust Be dependable and honest increases trust Accept the patient as a human being Don’t reinforce delusions or hallucinations Orient the patient as needed Give them short and simple information because schizophrenics can’t organize and think and make it from one point to another mentally. Don’t touch Avoid whispering and laughing Reinforce positive behaviors Supports appropriate behaviors Avoid competitive activities May threaten patient, decrease self-esteem Depends on the pt, some like it, some don’t Don’t embarrass the patient (never ever do this) Discourages communication and trust Encourage patient verbalization Helps patient feel comfortable, promotes self-esteem Evaluation Is there a sufficient after-care or crisis plan in place to deal with recurrence of symptoms or difficulties encountered in the community? Are the patient and family adequately knowledgeable about schizophrenia? Does the patient believe that he or she has a satisfactory quality of life? Elder Considerations o Psychotic symptoms that appear in later life are usually associated with depression or dementia, not schizophrenia o Elderly people with schizophrenia experience a variety of long-term outcomes This one woman tried to kill herself in the shower but failed and received a fracture from the fall Community Based Care o Assertive community treatment (ACT) o Behavioral home health o Community support programs o Case management Mental Health Promotion o Psychiatric rehabilitation has the goal of recovery for patient, more than just symptom control and medication management o Early identification and aggressive treatment of psychotic symptoms maximizes recovery and quality of life o Studies identifying at-risk individuals and implementing early interventions result in improved prodromal symptoms, prevention of social stagnation or decline, and prevention or delay of progression to psychosis Self-Awareness Issues o May be challenging if patient is suspicious or mistrustful, or nurse is frightened o Nurse may become frustrated if patient is noncompliant o Nurse must not take patient’s success or failure personally; the patient’s remarks and behavior or noncompliance are not personal toward the nurse but are part of the illness o Focus on the patient’s strengths and time out of the hospital, not just on symptoms and need for acute care o No nurse has all the answers