Schizophrenic Disorders
advertisement
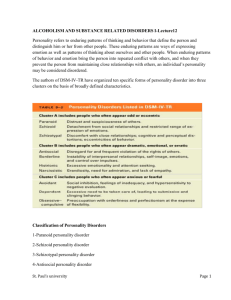
Schizophrenic Disorders Chapter 13 Onset and Course of the Disorder • Onset-typically occurs during adolescence or early adulthood. • Period of risk-for the development of the disorder is thought to be between the ages of 15 and 35. • The course of schizophrenia can follow many different patterns, but the problems of most patients can be divided into three phases. Three Phases of Schizophrenic Onset • Promodol-precedes the phase of active schizophrenia. • Active Phase: appearance of the positive symptoms. • Residual Phase • Positive symptoms; such as hallucinations, delusions, and disorganized speech have improved. • Symptoms similar to the promodal phase: negative symptoms become more pronounced Symptoms • Positive symptoms- psychotic symptoms or the presence of aberrant behavior. • Negative symptoms- defined as responses that are missing from the persons behavior . • Disorganization - include verbal communication problems and bizarre behavior. Positive Symptoms • Hallucinations-sensory experiences that are not caused by actual external stimuli. • Delusional Beliefs-beliefs held with the utmost conviction, even when presented with contrary evidence. – Preoccupation with the delusions to the point that the patient finds it difficult to NOT talk about the delusion. – Common delusions include the belief that thoughts are being inserted into the patient’s head, and that other people are reading the patient’s thoughts. Negative Symptoms • Blunted Affect -restriction of patients nonverbal display of emotional responses. • Anhedonia -inability to experience pleasure • Social Withdrawal -early symptom that something is wrong, appears to be both a symptom of the disorder and a strategy that is actively employed by some patients to deal with their other symptoms. • Avolition-lack of will do anything. Become apathetic and cease to work toward personal goals or to function independently. s. • Alogia-speech disturbance that refers to impoverished thinking. – Poverty of speech-don’t have anything to say – Thought blocking-patient’s train of speech is interrupted before a thought or idea has been completed. Disorganized • Disorganized Speech-tendency of the schizophrenic to say things that don’t make sense, including irrelevant responses to questions, expressing disconnected ideas, and using words in peculiar ways. – Loose association (derailment)-shifting topics too abruptly – Tangentiality-replying to a question with an irrelevant response. – Perseveration-persistently repeating the same word or phrase over and over again. • Bizarre Behavior – Catatonia-most often refers to immobility and marked muscular rigidity. • Can also refer to excitement and overactivitysuch as purposeless pacing, repetitious movements. – Stupurous state-reduced responsiveness where the person seems unaware of their surroundings, though completely conscious and believed able to hear and understand everything going on around them. – Inappropriate affect-`lack of adaptability in emotional expression. Diagnostic Criteria-DSM-IV • Characteristic Symptoms: Two or more of the following present for a significant portion of time during a one month period: – – – – – Delusions Hallucinations Disorganized speech Grossly disorganized or catatonic behavior Negative symptoms, such as flat affect, alogia or avolition • Social/Occupational Dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care is markedly below the level achieved prior to the onset. • Duration-Continuous signs of disturbance persist for at least 6 months Subcategories: Five Subtypes • Catatonic-characterized by symptoms of motor immobility or excessive and purposeless activity • Disorganized-characterized by disorganized speech, behavior and flat or inappropriate affect. • Paranoid- delusions of persecution or grandiosityfrequent auditory hallucinations • Undifferentiated Type- display psychotic symptoms but do not meet the criteria for a specific subtype • Residual Type- no longer meet the criteria for active phase, but still exhibit negative symptoms and some forms of hallucinations, delusions, or disorganized speechsaid to be in a partial remission. Related Psychotic Disorders • Schizoaffective Disorder -defined by an episode in which the symptoms of schizophrenia partially overlap with a major depressive episode or a manic episode. • Delusional Disorder –Do not meet the full symptomatic criteria for schizophrenia, but are preoccupied for at least one month with delusions that are not bizarre. • Brief Psychotic Disorder- people who exhibit psychotic symptoms, such as delusions, hallucinations, disorganized speech for at least 1 day but less than one month. The episode often follows a stressful event. Course and Outcome • Severe progressive disorder that most often begins in adolescence. • Recent evidence indicates there can be marked improvement in the patient, but the prediction of which is difficult. • Patient is thought to be improved in relation to symptom severity and occupational functioning relative to initial assessment. • Best predictor of future social adjustment appears to be previous social adjustment. Epidemiology • Lifetime risk factors for the general population are 1%. • Gender Differences • Cross Cultural Etiology • Biological Factors -strongest evidence for etiology. • Social Factors - The disorder appears to be expressed in its full blown form only when vulnerable individuals experience some type of environmental event, which might include anything from nutritional variables to stressful life events. • Psychological Factors -research indicated that family interactions and communication problems are not primarily responsible for the initial appearance of symptoms, however they may contribute to the onset of the disorder in people with a genetic predisposition, and they also influence the course of the disorder after the symptoms have appeared. Biological Factors • • • • • Genetics Pregnancy and Birth Complications Viral Infections Neuropathology Neurochemistry Genetics • Twin Studies-MZ =48%, DZ =17 • Linkage studies-designed to identify the location of a specific gene that is responsible for the disorderunable to identify a specific gene, but has implicated regions on a small number of chromosomes that may contribute to the etiology. Pregnancy and Birth Complications • People with schizophrenia are more likely than the general population to have been exposed to various problems during their mother’s pregnancy and to have suffered birth injuries. • Birth complications • Severe malnutrition during the early months of pregnancy leads to an increased risk of schizophrenia among the offspring. Viral Infections • People who develop schizophrenia are somewhat more likely than other people to have been born during the winter months, making their mothers more likely to develop viral infections during their pregnancies which are more prevalent during the winter. • Exposure to infection presumably interferes with brain development in the fetus. Neuropathology – Decrease in total volume of brain tissue among schizophrenic patients. – Mildly to Moderately enlarged ventricles at the expense of other brain regions. – Decreases size of the hippocampus, parahippocampus, amygdale, and the thalamus, all of which are parts of the limbic system, and play a crucial role in the regulation of emotion as well as the integration of cognition and emotion. – Reversal in asymmetry with regard to size in the planum temporale….usually larger in the left hemisphere than the right in men, in schizophrenics it is reversed. – PET scans An fMRi indicate dysfunction in several neural circuits as this type of imaging is conducted while the patient is conducting specific tasks. Results indicate dysfunction in various neural circuits including regions of the prefrontal cortex, and temporal lobes. – Conclusions from imaging studies indicate that the neural network connecting the limbic areas with the frontal cortex may be fundamentally disordered in schizophrenia, but the dysfunction seems to be associated with an over-all severity of the disorder rather than etiology of a subgroup of patients. Neurochemistry • Dopamine Hypothesis • Multiple Neurotransmitters Dopamine Hypothesis • Original tenet of this hypothesis was that the disorder was caused by excess levels of Dopaminergic activities, which could be supported by the excessive number of D2 receptors found in the brains of schizophrenic patients on autopsy • Increased D2 receptors could lead to elevated sensitivity to DA. • Antipsychotic drugs improve the symptoms of many schizophrenic patients. • Mechanism of action in the antipsychotic drugs is blockage of the DA post-synaptic receptors leading to an increase in release at the pre-synaptic neuron. • The neuro-chemical model focusing solely on DA failed to explain several aspects of the disorder. – Treatment with antipsychotic drugs produces an increase in D2 receptors. – Some patients do not respond positively to typical antipsychotic drugs. Multiple Neurotransmitters • Evidence exists that other Neurotransmitters may be involved that involve complex interactions with DA pathways. • Serotonin-Relief of symptoms via the atypical antipsychotic drugs, which produce a strong blockade of serotonin drugs and a very weak blockade of the D2 receptor. • Glutamate (excitatory) and GABA (inhibitory) involvement due to their interaction with DA pathways that connect the temporal lobe structures with the prefrontal and limbic cortexes. Social Factors • Social Causation Hypothesis • Social Selection Hypothesis Psychological Factors • Expressed Emotion-in either form of hostility and too little support or over protectiveness, significantly contributes to patient relapse following hospital discharge. • Expressed Emotion is a reciprocal process • Some patients relapse in spite of an understanding family environment. Criteria for Vulnerability Markers – Must distinguish between those who already have schizophrenia and those who do not – Markers should be stable characteristic over time – Proposed measure should identify more people among the biological relatives of schizophrenic patients than among people in the general population. – Should be able to predict the future development of schizophrenia among those who have not yet experienced a psychotic episode. – Reliable vulnerability markers have not yet been identified, but are being actively pursued. Possible Vulnerability Markers • Attention and Cognition Deficits in a Continuous Performance Task in schizophrenic patients and unaffected first degree relatives. • Eye Tracking Dysfunction Treatment Multi-faceted approach includes medication, family therapy, and skills training. However, medication is the primary treatment for the disorder. Medication Psychosocial Treatment Medication – Typical Antipsychotic Drugs- strong affinity for DA receptor sites. Positive symptoms such hallucinations, respond better to the typical Antipsychotic drugs than the negative symptoms such as alogia or blunted affect. • High rate of non-responders-25% • Several motor side effects (extra-pyramidal side effects )—include muscular rigidity, tremors, restless agitation, strange involuntary movements and inability to initiate motor movements. • Tardive Dyskinesia-syndrome of abnormal involuntary movements of the mouth and face, such as tongue protrusion and lip smacking, as well as spastic movements of the limbs and trunk. This condition frequently occurs with long term use of typical antipsychotics. Can be irreversible in some patients. • Best known-thorazine – Atypical Antipsychotic Drugs-strong affinity for serotonin with weak affinity for DA. • Are effective for both positive and negative symptoms. • Much less likely to produce motor side effects. • Main side effects are severe weight gain and obesity which has been known to lead to diabetes. • Best known-risperdal, Zyprexa Maintenance Medication – Relapse rate during the first year after hospital discharge is 65-70% if patients discontinue medication. – Continued medication at a reduced rate after they recover from psychotic episodes can reduce this rate to 40% Psychosocial Treatment • • • • Family oriented aftercare Social Skills Training Assertive Community Treatment Institutional Programs