Peer Review System - ampi
advertisement
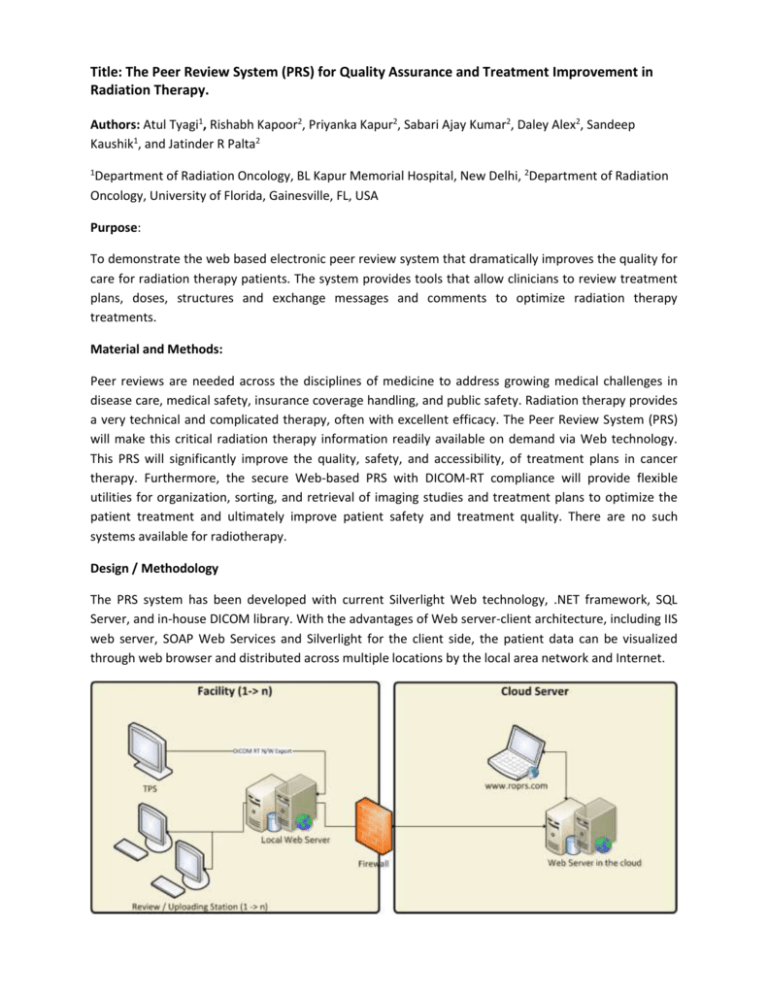
Title: The Peer Review System (PRS) for Quality Assurance and Treatment Improvement in Radiation Therapy. Authors: Atul Tyagi1, Rishabh Kapoor2, Priyanka Kapur2, Sabari Ajay Kumar2, Daley Alex2, Sandeep Kaushik1, and Jatinder R Palta2 1 Department of Radiation Oncology, BL Kapur Memorial Hospital, New Delhi, 2Department of Radiation Oncology, University of Florida, Gainesville, FL, USA Purpose: To demonstrate the web based electronic peer review system that dramatically improves the quality for care for radiation therapy patients. The system provides tools that allow clinicians to review treatment plans, doses, structures and exchange messages and comments to optimize radiation therapy treatments. Material and Methods: Peer reviews are needed across the disciplines of medicine to address growing medical challenges in disease care, medical safety, insurance coverage handling, and public safety. Radiation therapy provides a very technical and complicated therapy, often with excellent efficacy. The Peer Review System (PRS) will make this critical radiation therapy information readily available on demand via Web technology. This PRS will significantly improve the quality, safety, and accessibility, of treatment plans in cancer therapy. Furthermore, the secure Web-based PRS with DICOM-RT compliance will provide flexible utilities for organization, sorting, and retrieval of imaging studies and treatment plans to optimize the patient treatment and ultimately improve patient safety and treatment quality. There are no such systems available for radiotherapy. Design / Methodology The PRS system has been developed with current Silverlight Web technology, .NET framework, SQL Server, and in-house DICOM library. With the advantages of Web server-client architecture, including IIS web server, SOAP Web Services and Silverlight for the client side, the patient data can be visualized through web browser and distributed across multiple locations by the local area network and Internet. Figure 1. PRS Architecture Figure 1 show the architecture of the system which has a local web server (DICOM RT Archive) to store the treatment planning data from the TPS. This storage is done via standard network DICOM send / receive interface. The architecture has the review / uploading stations to select the case and de-identify the data element to remove patient’s identity. It also provides a secure encryption model via which the data is securely transmitted to the web server in the cloud from the local web servers of multiple institutions. Before the data is submitted the remote peer reviewer are identified and tagged with the patient’s record. As soon as the submission is completed then the remote reviewers are notified via Email / SMS about their pending case for review. The remote reviewers have to login to the web portal (www.roprs.com) and load up the case on their browser. The web portal contains tools to annotate and provide textual comments for the submitter for the purpose of reviewing this case. Once the case has been successfully reviewed the comments are transmitted back to the local web server of the submitter and displayed with the case on the review stations. Results: To validate the PRS system, we tested the system for 100 patients with Philips Pinnacle v 9.0 and Varian Eclipse v 8.9 treatment planning system (TPS). We transmitted the DICOM RT data from the TPS to the cloud based services via the PRS local DICOM RT Archive. Various CT simulation based parameters such as orientation of CT, properties of RT structures etc. were compared between the TPS and PRS system. Data integrity of other parameters such as patient demographics (patient name, ID, attending physician etc.) and dose volume related parameters were also evaluated. Such rigorous testing allowed us to optimize the functionalities and clinical implementation of the PRS. Conclusions We believe that the PRS will improve the quality and safety of a broad spectrum of radiation therapy patients treated in underserved areas while discouraging the overutilization of expensive radiation treatment modalities. Acknowledgement: This research and development project is supported by the James and Ester King Biomedical Research Program grant # RC1-09KW-09-26829