Ch 17 Functions of the Blood
advertisement

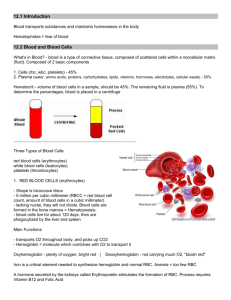
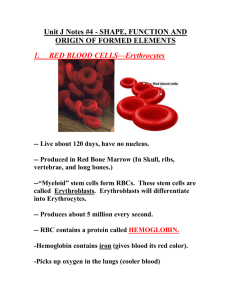
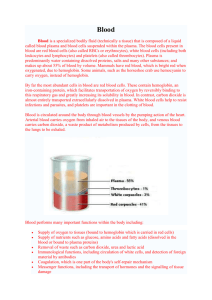
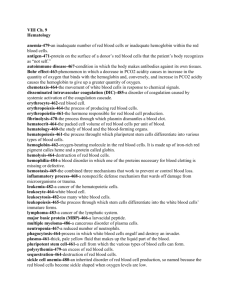
Ch 17 Functions of the Blood Chapter Summary • Blood transports molecules and heat from one area of the body to another, defends against foreign agents, and assists in the maintenance of extracellular fluid pH and osmolarity. • Blood is a connective tissue containing erythrocytes, leukocytes, thrombocytes, and plasma. • Average adult blood volume is 5 L. • Plasma is the intercellular fluid of the blood. Plasma is approximately 93% water and 7% solutes (inorganic and organic). • Plasma proteins are divided into the following fractions: albumin, globulins, and fibrinogen. Plasma proteins serve as amino acid reserves, carriers, and buffers and also participate in blood coagulation and the regulation of fluid distribution within the body. The immune globulins play important roles in the body’s defense. • Hematopoiesis is the generation of blood cells from pluripotential hemopoietic stem cells (PHSCs). • PHSCs develop into committed progenitor cells called colonyforming units (CFUs), which generate colonies of specific blood cell types. • The erythrocyte is a biconcave, anucleated cell that numbers approximately 5 million cells/μL of whole blood. • Erythrocytes contain hemoglobin, which transports oxygen. One gram of hemoglobin can transport 1.34 mL of O2. The amount of hemoglobin in blood is approximately 15 g/dL; therefore, the oxygen-carrying capacity of blood is approximately 20 mL of O2 per deciliter. • Erythropoiesis is the formation of erythrocytes. Normally, approximately 230 billion red blood cells are produced each day. Substances required for erythropoiesis include vitamin B12, folic acid, iron, and protein. Erythropoiesis is controlled by a renal hormone called erythropoietin. • Approximately 230 billion red blood cells are destroyed each day. When an erythrocyte is destroyed, most parts of the hemoglobin are conserved. The remainder is excreted as bilirubin in bile. • Anemia is an abnormal reduction in the oxygen-carrying capacity of the blood. Anemias are characterized by changes in one or more of the following red blood cell indices: MCV, MCH, and MCHC. • Polycythemia is a relative or absolute increase in the number of circulating red blood cells above normal. Two main types are polycythemia vera and secondary polycythemia. • The ABO blood group contains blood types based on the presence or absence of antigens A and B on the red blood cell membrane. • Major agglutination occurs when donor red blood cells containing a strong antigen possessed by the recipient are infused into the recipient’s body. • Minor agglutination occurs when donor plasma containing antibodies against the recipient’s red cell antigens is infused into the recipient’s body. • The Rh blood group contains blood types based on the presence or absence of antigen D. If antigen D is present on the red blood cell membrane, the blood type is Rh-positive. If antigen D is absent, the blood type is Rh-negative. The plasma of an Rh-negative person may or may not contain anti-D. • Leukocytes are blood cells that do not contain hemoglobin. Two principal categories are granulocytes and granulocytes. On the average, whole blood contains approximately 7000 to 10,000 leukocytes/μL. Their principal function is body defense. • T-lymphocytes convey cell-mediated immunity, and B-lymphocytes convey antibody-mediated immunity. • Leukopoiesis, the formation of leukocytes, occurs primarily in the bone marrow, although some leukocytes mature outside the marrow in lymphoid organs. • Thrombocytes, or platelets, are produced from megakaryocytes. One megakaryocyte gives rise to approximately 6000 platelets. • Platelets play several roles in hemostasis. • Local vasoconstriction helps minimize blood loss when a blood vessel is opened. • Platelets clump together, forming a plug at the site of vascular damage. Platelets also release procoagulants. • Coagulation of blood, or formation of a blood clot, at the site of vascular injury helps seal the opened vessel. Coagulation involves the formation of fibrin thread, which is the foundation of the clot. • Fibrin formation occurs in three states: stage I—formation of prothrombin-converting factor, stage II—conversion of prothrombin to thrombin, and stage III—conversion of fibrinogen to fibrin. • After formation of a clot, clot retraction helps draw wound surfaces together. • Clots gradually are dissolved by enzymes that break down fibrin. • Abnormalities of hemostasis can result from platelet defects, coagulation defects, and/or excessive production of anticoagulants. Principal abnormalities include thrombocytopenia and hemophilia.