Chronic Condition Documentation
advertisement
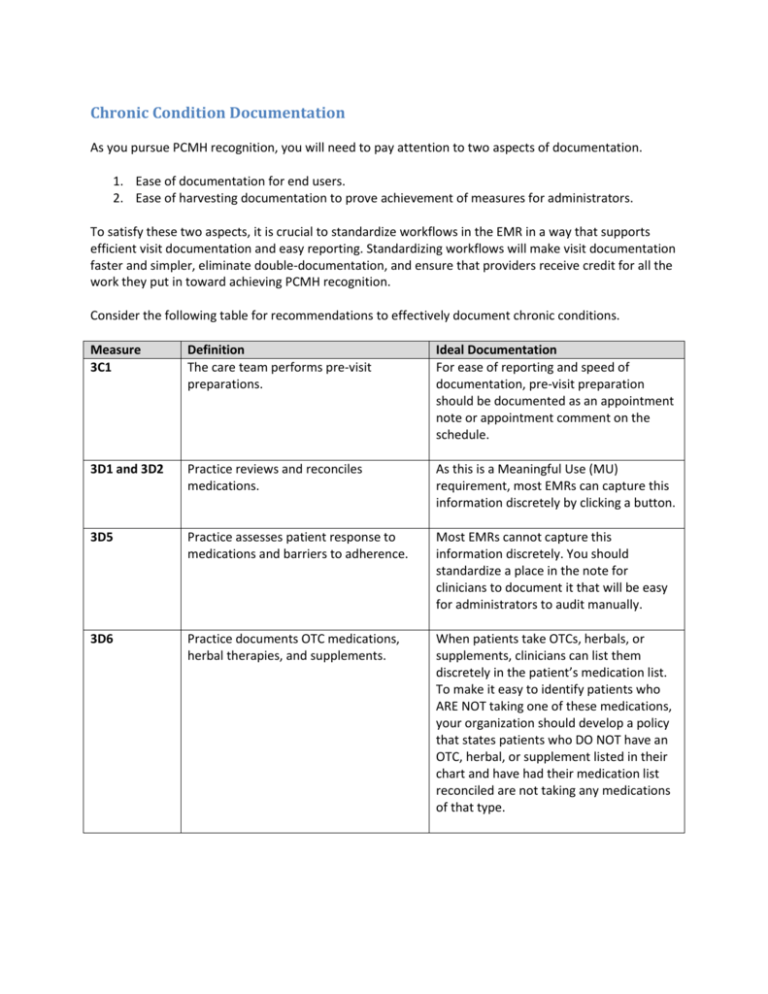
Chronic Condition Documentation As you pursue PCMH recognition, you will need to pay attention to two aspects of documentation. 1. Ease of documentation for end users. 2. Ease of harvesting documentation to prove achievement of measures for administrators. To satisfy these two aspects, it is crucial to standardize workflows in the EMR in a way that supports efficient visit documentation and easy reporting. Standardizing workflows will make visit documentation faster and simpler, eliminate double-documentation, and ensure that providers receive credit for all the work they put in toward achieving PCMH recognition. Consider the following table for recommendations to effectively document chronic conditions. Measure 3C1 Definition The care team performs pre-visit preparations. Ideal Documentation For ease of reporting and speed of documentation, pre-visit preparation should be documented as an appointment note or appointment comment on the schedule. 3D1 and 3D2 Practice reviews and reconciles medications. As this is a Meaningful Use (MU) requirement, most EMRs can capture this information discretely by clicking a button. 3D5 Practice assesses patient response to medications and barriers to adherence. Most EMRs cannot capture this information discretely. You should standardize a place in the note for clinicians to document it that will be easy for administrators to audit manually. 3D6 Practice documents OTC medications, herbal therapies, and supplements. When patients take OTCs, herbals, or supplements, clinicians can list them discretely in the patient’s medication list. To make it easy to identify patients who ARE NOT taking one of these medications, your organization should develop a policy that states patients who DO NOT have an OTC, herbal, or supplement listed in their chart and have had their medication list reconciled are not taking any medications of that type. 4A3 Practice develops and documents selfmanagement plans and goals. Some EMRs can capture self-management goals discretely. For EMRs that cannot, clinicians should document selfmanagement goals in a standardized location in the note or in the patient instructions section of the visit, as determined by the organization. 3C2 The care team collaborates with the patient/family to develop and individual care plan, including treatment goals. Some EMRs can capture treatment goals discretely. For EMRs that cannot, clinicians should document treatment goals in a standardized location in the note or in the patient instructions section of the visit, as determined by the organization. 3C4 The care team assesses and addresses barriers when patient has not met treatment goals. Clinicians should document barriers to treatment goals in a standardized location in the note or in the patient instructions section of the visit, as determined by the organization. 3C6 The care team identifies patients/families who might benefit from additional care management support. In order to meet this standard, clinicians should document whether or not patients would benefit from additional care management support in a standardized location in the note as determined by the organization. 3C3 and 3C5 The care team gives the patient/family a written plan of care and clinical summary. The plan of care should be included as part of the clinical summary/AVS printed by your EMR. Because printing clinical summaries/AVS is a MU requirement, your EMR should already have a report that identifies patients who have received one. 4A1 Practice provides education resources or refers patients to educational resources to assist in self-management. For reliability of documentation, it is best in most EMRs to have clinicians document in their note that they provided education resources to patients. 4A2 Practice uses EHR to identify patientspecific education resources. End-user reporting tools in EMRs are the best way to identify groups of patients that could benefit from educational resources. Practices should run reports to find patients and show screenshots that show their method for providing the information to patients. 4A5 Practice provides self-management tools. Some EMRs allow end-users to send selfmanagement tools, such as flowsheets, to patients. For EMRs that do not support this, clinicians will need to document that they provided self-management tools to patients in a standardized location in the note. 4A6 Practice counsels patients to adopt healthy behaviors. Many EMRs allow discrete capturing of counseling, either via clicking a button or placing an order for patient instructions. For EMRs that do not, clinicians should document counseling provided as part of a note.