Coordinating care in medical practices p Ann S. O’Malley, MD, MPH
advertisement

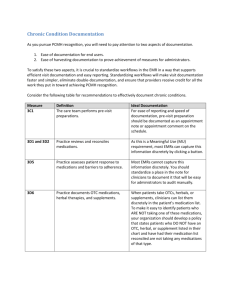
Coordinating care in medical practices p Ann S. O’Malley, MD, MPH Interventions to improve coordination Academy Health June 29, 2010 How are we using the term “Coordination of Care?” I Integration i off care across allll off a person’s: ’ Conditions & health needs Providers & settings Family & caregivers Community services, e.g. home health 2 Study 1: How are practices trying to coordinate care? Background: Calls to improve coordination, but little guidance Goal: Identify practices practices’ challenges, challenges strategies & facilitators “Bottom up approach” R Respondents: d t 62 clinicians li i i ffrom 36 PC & S Spec practices ti & TL 1. Notices on ACP, AAFP listservs 2 Referrals from thought leaders (TL) 2. We asked about coordination strategies: Within the primary care practice Between PC & other specialists/services Between outpatient & inpatient settings (Transitions) With community based services (few examples) 3 Study y 1: Challenges g to Coordination Lack of payment for coordination=“No Time” • Opportunityy costs for resources spent = lost revenue • “Culture of non-communication & non-ownership” Insufficient staff to help with coordination tasks Disruptions in continuity of care with PCP • Patient self-referrals and spec-spec cross-referrals • Changes g in plan provider networks, insurance Health plan provider networks • Inconsistent with PCP-spec. p trusted working g relationships p • Administrative burden 4 Study 1: How Practices Promote Coordination of Care for Patients Commitment C to continuity with PCP/Team C / Enlist patient/family in coordination Trusted us ed working o g relationships e a o s ps be between ee PC C & Spec Increase efficiency to make time for coordination Standardize particular coordination processes One size may not fit all Leadership, culture, and aligned $$ incentives 5 Study y 2: Current EMRs & Coordination Goal: Examine whether & how ambulatory care practices use commercial EMRs to support coordination tasks Respondents: • 60 providers id ffrom 26 practices ti iin 12 CTS (Community (C it Tracking Site) markets & national thought leaders • Practices with commercial EMR for > 2 years • Smaller-Medium size practices emphasized 6 Study y 2: Key y Findings g EMRs facilitate coordination within a practice via ed ate data access, instant sta t messaging essag g immediate EMRs less able to support coordination between practices & settings due to inadequate data standards poor interoperability, standards, interoperability low penetration Office work-flow changes necessary to maximize EMRs’ potential to support coordination (à la AHRQ) 7 Study y 2: Key y Findings g ((continued)) “Work-arounds” common (See JGIM article)** e.g. problem lists, performance reporting, referral tracking Redundant, unorganized printouts challenge end- user trying t i to t identify id tif critical iti l info i f for f coordination di ti EMRs do not capture dynamic coordination process FFS encourages EMR documentation for billing Need standardized data that can be “pushed back” to medical home from other providers to pop pop. EMR 8 What do findings imply for HITECH’s support of coordination of care? Need systematic y structures, tools & processes p for info. creation, transfer, receipt & recognition by the sending g & receiving g clinicians. Measures off “M M “Meaningful i f l HIT U Use”” could ld include i l d items that support, track and confirm completion of coordination di ti tasks. t k 9 Can findings help inform PPACA implementation around coordination? Strategies described have potential to improve coordination if aligned with payment incentives/supports PPACA: Better align payment with coordination goals: PC Payment boosts Public and private sector demonstrations & grants - Med Homes-Support for coordination as described - ACOs-Align incentives to create mechanisms for PC/specialists/hospitals/community services to coordinate - State level grants for teams/coordination Increase PC workforce-Can’t coordinate care without providers 10 Thanks to Funders: CMWF & HCFO Collaborators: Joy Grossman, Hoangmai H. Pham, Genna Cohen, Cohen Nicole Kemper, Kemper Matthew Davis R Respondents: d t Clinicians Cli i i and d thought th ht leaders l d 11 Additional information www.hschange.org EMR Coordination Study in JGIM can be found at: http://www.hschange.org/CONTENT/1104/OMalley.pdf Editorial: http://www.hschange.org/CONTENT/1104/Bates.pdf Coordination Research Brief can be found at: http://www.hschange.org/CONTENT/1058/1058.pdf aomalley@hschange.org 12 End of Academy y Health Presentation Extra slides follow with more details Links to full articles listed: slide 12 13 Study y 1: Strategies g Within PC practice p Emphasis E h i on continuity ti it with ith specific ifi clinician li i i Care coordinators (Med Asst to RN-SW) RN SW) PC Teams, Pods Role definition and training of all team members Restricting panel size Practices contract services they cannot provide Systems for phone triage & direct physician access Specialized programs for high risk patients 14 Study y 1: Facilitators Within PC Practice Involve I l patient/family ti t/f il iin coordination di ti • Medications, Self-management, ID self- & cross-referrals Care C Plans Pl Standardization of particular processes ex. How lab results reported to patients Planned care visits w pre pre-visit visit prep & post-visit post visit f/u Huddles (à la IHI, Health Partners, Bodenheimer, C. Sinsky, Wagner) Complexity C l i screener prior i to initial i i i l visit i i (Pediatric) (P di i ) HIT 15 Study 1: Strategies & Facilitators between PCP & Specialists Strategies: Limiting referral network to “trusted” relationships Shared Sh d Care C Pl Plans-patient ti t heavily h il involved i l d Referral Tracking Systems PCP-Specialist Service Agreements E E-referrals referrals (see Hal Yee’s Yee s work) (see Antonelli’s work) Facilitators: Well constructed referral/consultation notes Real-time communication between providers Enlist patient in information transfer Shared EMR 16 Study y 1: Strategies g & Facilitators-Transitions Link & Share Care Plan with ED* PCP-Hospitalist communication Care Transitions Program (à la Coleman et al; Naylor et al) Facilitated by: S Shared a ed financial a c a incentives ce es & staff sa 17