MENDEL-2 MS Supplement (Koren)
advertisement
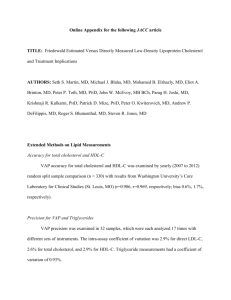
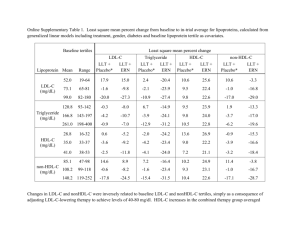
MENDEL-2 MS Supplement (Koren) J Am Coll Cardiol Appendix Anti-PCSK9 Monotherapy for Hypercholesterolemia – The MENDEL-2 Randomized, Controlled Phase 3 Clinical Trial of Evolocumab Michael J. Koren, MD*, Pernille Lundqvist, MD†, Michael Bolognese, MD‡, Joel M. Neutel, MD§, Maria Laura Monsalvo, MDǁ, Jingyuan Yang, PhDǁ, Jae B. Kim, MDǁ, Rob Scott, MDǁ, Scott M Wasserman, MDǁ, Harold Bays, MD¶ for the MENDEL-2 Investigators *Jacksonville Center for Clinical Research, Jacksonville, FL, USA; †Center for Clinical and Basic Research, Ballerup, Denmark; ‡Bethesda Health Research Center, Bethesda, MD, USA; §Orange County Research Center, Tustin, CA, USA; ǁAmgen Inc., Thousand Oaks, CA, USA, ¶L-MARC Research Center, Louisville, KY, USA Supplementary Methods. ..................................................................................................... Page S2 1 MENDEL-2 MS Supplement (Koren) J Am Coll Cardiol Supplementary Methods Key exclusion criteria Key exclusion criteria included heart failure; CHD history; recent deep vein thrombosis or pulmonary embolism; uncontrolled cardiac arrhythmia or hypertension; diabetes mellitus; thyroid, liver, gastrointestinal, endocrine, or renal dysfunction; malignancies within 5 years except for non-melanoma skin cancers or carcinoma in situ; or use of lipid-regulating drugs within 3 months. Study drug preparation Evolocumab and placebo SC were presented as a sterile, preservative-free solution in a single use, disposable, handheld (spring-based) prefilled auto-injector pen. Study drug administration occurred after all assessments and blood drawing procedures. Subcutaneous study drug was administered either as one injection of 1.0 mL of 140 mg/mL evolocumab or placebo biweekly or three administrations within 30 minutes of 1.0 mL of 140 mg/ mL (420 mg) evolocumab or placebo monthly. Day 1, week 2, week 8, and week 10 treatments occurred at study sites administered by site staff or patient self- injection. Patients selfadministered injections at week 4 and week 6 in non-clinical settings. All patients received oral ezetimibe or placebo. To enable blinding, ezetimibe or placebo were administered in over-encapsulated 10 mg tablets. Telephone assessments were made at week 14 for biweekly patients. Laboratory methods Research sites collected samples for lipid measurements after ≥9 hours of fasting. LDL-C levels were calculated using the Friedewald equation (Friedewald et al. Clin Chem 2 MENDEL-2 MS Supplement (Koren) J Am Coll Cardiol 1972;18:499-502). For calculated LDL-C values <40 mg/dL or triglycerides >400 mg/dL, ultracentrifugation determined LDL-C was measured and reported. All analyses were performed in a Center for Disease Control Part III standardized central laboratory, Medpace Reference Laboratory (Cincinnati, OH and Leuven, Belgium). Safety testing was conducted in an accredited central laboratory as previously described (Raal et al. Circulation 2012;126:2408-17). Immunoassays for detection of anti-evolocumab binding antibodies were conducted by EMD Millipore Corporation (St. Charles, MO) and Amgen Inc. Statistical analysis The planned enrollment of 600 patients (300 evolocumab) had ≥92% power to detect the superiority of both evolocumab administration regimens over placebo and ezetimibe based on a 2-sided t-test with a 0.025 significance level for each co-primary endpoint. Efficacy and safety analysis included all randomized patients who received at least one dose of the study drug. The co-primary and co-secondary efficacy endpoints were analyzed using a repeated measures linear effects model for each dose frequency with no imputation of missing data, except for achievement of LDL-C <70 mg/dL, which was analyzed using the Cochran-Mantel-Haenszel test. Multiplicity adjustment was based on a combination of sequential testing, the Hochberg procedure (Hochberg. Biometrika 1988;75:800-2), and fallback procedure to control the overall significance level for all primary and secondary endpoints. Sensitivity analyses were conducted by applying a repeated measures linear effects model and Quade test (Quade. J Am Stat Assoc. 1967;62:1187-1200) to patients who adhered to the scheduled study drug administration and had non-missing co-primary endpoints. Covariate analysis was conducted using a similar repeated measures model but included the covariates of interest, one at a time, as a fixed effect. 3 MENDEL-2 MS Supplement (Koren) J Am Coll Cardiol Safety analyses were conducted using descriptive statistics. Adverse events were classified by MedDRA (version 16.1). 4