A55(Th) Appropriate heparin use in thromboprophylaxis and the
advertisement
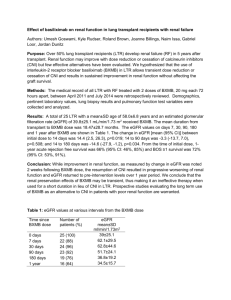
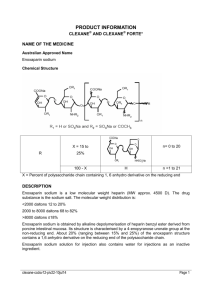
A55(Th) APPROPRIATE HEPARIN USE IN THROMBOPROPHYLAXIS AND THE TREATMENT OF ACUTE CORONARY SYNDROME IN PATIENTS WITH RENAL FAILURE Yiu, V1, Namagondlu, G2, Camilleri, B2 Addenbrookes Hospital, 2Ipswich Hospital 1 INTRODUCTION: Evidence based guidelines recommend the use of thromboprophylaxis in hospitalised patients at risk of venous thromboembolism (VTE). The most commonly used agent is heparin, usually low molecular weight heparin (LMWH). This is also commonly used in the treatment of acute coronary syndrome (ACS). Unfractionated heparin (UFH) has a narrow therapeutic window, requires monitoring and can rarely be associated with thrombocytopenia. LMWH has similar efficacy but has the advantage of fixed dosing. It is renally excreted and hence dose adjustment is needed for patients with renal impairment. Ipswich Hospital recently published guidelines on screening all patients admitted for VTE risk factors and appropriate dosing of LMWH (if eGFR <30ml/min, half dose Clexane should be used). Guidelines on ACS treatment recommended 1mg/kg once daily if eGFR<30ml/min, or the use of UFH if eGFR <15ml/min. METHODS: We audited compliance with these guidelines in 30 medical patients and 15 patients with ACS admitted over a 3 month period who also had renal impairment. Consecutive patients’ notes were reviewed and a proforma used to collect data. RESULTS: The mean age of patients was 80.4years, and two thirds were male. The mean eGFR was 20.5ml/min. The majority of patients admitted were screened for VTE risk (86%) and had Clexane prescribed (70%). However, over half the patients did not have a dose appropriate for reduced eGFR. 1 patient whose eGFR improved did not have the Clexane dose adjusted; another had their dose adjusted only after 4 days. 60% patients admitted for ACS were male, with a mean age of 77.8years. Patients who were already on warfarin with a therapeutic INR did not have clexane for ACS treatment. There were several patients who were deemed too frail for further treatment, hence 80% were prescribed LMWH/UFH. Around half had inappropriate dosing and one third had longer duration of treatment than the recommended 48 hours. Over half did not have an eGFR appropriate prophylactic dose of Clexane prescribed after treatment. CONCLUSIONS: VTE prophylaxis is now commonly prescribed and is vital to reduce morbidity and mortality in hospital patients. However, patients frequently have renal impairment on admission and they are at increased risk of bleeding from inappropriately high doses of Clexane. If their GFR improves during admission and the Clexane dose is not revised, they do not derive the benefits of this treatment. Bleeding risk is especially important in patients with ACS who also receive antiplatelet therapy and may undergo invasive procedures such as angiograms. We proposed measures such as mandatory documentation of eGFR on the admission clerking, VTE/ACS treatment guidelines to be placed on all wards, improving awareness through Trust induction and collaborating with other health professionals (nurses, pharmacists) to help ensure all patients with renal impairment receive appropriate VTE prophylaxis and ACS treatment. This study was a snapshot of practice at Ipswich Hospital, and more studies are needed to address optimum dosing regimens and practice on a national scale.