Renal function in chronically hepatitis B virus infected patients
advertisement

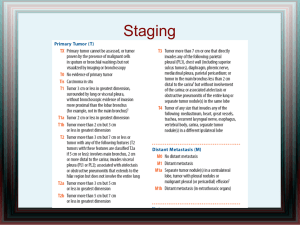
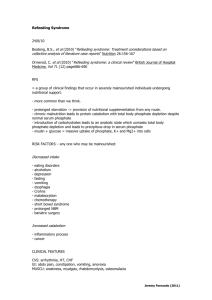
P381 CHANGES IN SERUM PHOSPHATE AND RENAL FUNCTION IN PATIENTS WITH CHRONIC HEPATITIS B VIRUS INFECTION TREATED WITH ADEFOVIR AND TENOFOVIR O’ Riordan, A1, Carey, I2, Agarwal, K2, Harrison, P2,3, Hendry, B1,3 1 Department of Renal Medicine and 2Institute of Liver Studies at King’s College Hospital, London and 3King’s College London INTRODUCTION: Effective treatments for chronic hepatitis B virus infection (HBV) include the nucleotide analogues, adefovir (ADV) and tenofovir (TDF) and their use is expected to increase significantly in coming years. However both can potentially cause hypophosphataemia and renal impairment and Fanconi syndrome has also been described. This has been more widely reported in HIV infected patients but may be a cause for concern in mono-infected HBV individuals. This study aimed to evaluate changes in estimated glomerular filtration rate (eGFR) and serum phosphate in patients with chronic HBV treated with ADV or TDF and to compare the results to those seen when patients were treated with other agents (OA) i.e. lamivudine monotherapy / interferon alfa 2a / pegylated interferon alpha 2a. METHODS: Patients with HBV treated with 10mg ADV (n = 193) or 245mg TDF (n = 20) between 2002 and 2008, were identified. Those on dialysis or co-infection with HIV or hepatitis C virus were excluded. Serum phosphate and creatinine were recorded and the eGFR calculated pre-treatment and longitudinally thereafter. Changes in phosphate were graded using a modified National Institute of Allergy and Infections Diseases toxicity grading scale and reductions in eGFR were graded as 0 – 25%, 26 – 50%, 51 – 75% or > 75%. Eighty-three of these patients had previously been treated with OA and baseline and subsequent biochemistry data was available in 58 of them. This group was used as the reference category. Changes in phosphate and renal function were adjusted for baseline differences between the 3 groups in terms of patient demographics, co-morbidities, liver function, HBV DNA levels and liver biopsy data. Statistical analysis was performed using SPSS and a significant difference (P < 0.05) between ADV / TDF and OA is designated as *. Percentages and mean + standard deviation are displayed. RESULTS: The majority were male (81%) and black (45%) with a mean age of 42 + 11 and follow up of 2 + 1 years. The duration of follow up was significantly less in those treated with TDF. Using linear mixed modelling, there was no difference between the 3 groups in terms of the changes in phosphate or eGFR over time compared with the pre-treatment values. Similarly, there was also no difference in the proportion of patients developing all grades of hypophosphataemia or reduction in eGFR while on treatment. Severe hypophosphataemia (< 0.31 mmol/L) or reductions in eGFR by > 75% occurred with ADV and OA but were very rare. However the percentage decline in phosphate (ADV*, -15%; TDF*, -14%; OA, -22%) and eGFR (ADV*, -10%; TDF - 11%; OA, -14%) from prior to treatment to the minimum values recorded, were significantly greater with OA. There was also no difference between the 3 groups in terms of sustainability or reversibility of hypophosphataemia and decline in eGFR. CONCLUSION: In those with chronic HBV there was no overall difference in the change in serum phosphate and eGFR from baseline in those treated with ADV or TDF compared with OA. However those on OA were more likely to have a lower trough phosphate and eGFR. Nonetheless renal adverse effects do occur so phosphate and eGFR monitoring is recommended with these agents.