Postoperative Renal Complications
advertisement
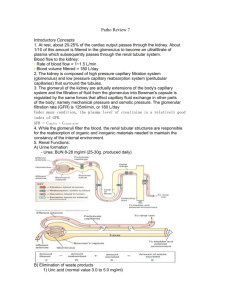
Postoperative Renal Complications By: Matthew LeDuc M.D. Ability to Void: Needs to be assessed as opioids and autonomic side effects of regional anesthesia interfere with sphincter relaxation causing retention Retention is common following urologic, inguinal and genital surgery Ultrasonic bladder scan helps access bladder volume and is less invasive than “straight cath” Reasonable to discharge patients prior to voiding however plan must be in place to insure patient returns should voiding not occur in 10-12 hours. Renal Tubular Function: Urine color not useful in assessing concentrating ability however is useful in detecting hematuria and pyuria Osmolarity >450 mOsm/L indicates intact tubular concentrating ability Urine sodium conc. Far below serum concentrations or urine potassium above concentrations indicates tubular viability. Osm, electrolyte, PH values close to serum may indicate poor tubular function or ATN. Interactions of sevoflurane with dry carbon dioxide absorbents (often found after 1st case of the day on Monday) generates compound A, a vinyl ether that degrades to release inorganic fluoride which can result in ATN. Note: This is very rare and it is accepted that use of Sevo dose not seriously affect renal function Oliguria: Def: <0.5 ml/kg/hr Often an appropriate response to hypovolemia In patients w/o catheters assess interval since last voiding and bladder volume to help differentiate oliguria from inability to void. Check indwelling urinary catheters for kinking, obstruction by blood clots or debris and for catheter tip positioned above urinary level in the bladder. Aggressively evaluate oliguria if intraoperative events could jeopardize renal function such as aortic cross clamping, severe hyptension, possible urethral ligature or massive transfusion. After urine is sent for electrolytes and osm a 300-500cc NS bolus helps to differentiate decreased tubular function from hypovolemia. Persistence of low urine output despite fluid challenge, adequate blood pressure and lasix challenge increases likelihood of ATN, urethral obstruction, renal artery or vein occlusion or SIADH. Polyuria: Def: 4-5 ml/kg/hr Profuse urine output often reflects generous intraoperative fluid administration Osmotic diuresis can occur if hyperglycemia and glycosuria is present Sustained polyuria can indicate abnormal regulation of water clearance or high-output renal failure. Diabetes insipidus (inadequate secretion of ADH from the posterior pituitary or resistance of renal tubules to ADH results in polydipsia, hypernatremia and high output urine) Causes of DI include: intracranial surgery, pituitary ablation, head trauma or increased ICP. Treatment of DI: DDAVP Reference: Paul G. Barah, Clinical Anesthesia: 5th edition 2006