Chapter 21: Genitourinary and Renal Emergencies
advertisement

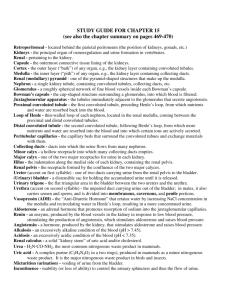
Chapter 21: Ready for Review • Chronic kidney disease is the most common renal disorder. Kidney stones and urinary tract infections also affect many people. • The genitourinary system includes the kidneys, urinary bladder, ureters, urethra, male and female reproductive organs, and specific structures within the kidneys. • Blood flows through the kidney into the afferent arteriole and then through the glomerulus, the main filter. It then enters the efferent arteriole, followed by the peritubular capillaries, where it is reabsorbed. • Urine forms in the nephrons. The nephrons are composed of the glomerulus, the glomerular capsule, the proximal convoluted tubule, the loop of Henle, and the distal convoluted tubule. • In the glomerular capsule, filtrate from the blood—which contains salts, minerals, glucose, water, and metabolic wastes—passes through a membrane. Next, it passes through the rest of the nephron, after which it is converted into urine. This urine passes through the proximal convoluted tubule and the loop of Henle to be further concentrated. • In the distal convoluted tubule, the composition of urine is further refined based on the body’s needs. Two hormones, antidiuretic hormone and aldosterone, are involved in adjusting the urine composition. • The juxtaglomerular apparatus in the kidneys releases renin, an enzyme that causes reactions in the body such as an increase in blood pressure. • Diuretics are chemicals that increase urinary output. • As urine collects in the bladder, the micturition reflex causes the bladder to contract, stimulating the urge to void. • The anatomy of the urethra is different in males and females. The female urethra is shorter and therefore more prone to urinary tract infections. • In the physical examination, use the four-quadrant system and abdominal region mapping. Perform cardiac monitoring, and do not give urologic patients anything by mouth. • Visceral pain is the type most often associated with genitourinary problems. Referred pain originates in one organ or tissue but is perceived by the patient to be located in a different area of the body. • The OPQRST (onset, provocation, quality, region/radiation/referral, severity, timing) mnemonic is used during the primary and secondary assessments to evaluate and reevaluate the type and severity of pain. • Pain is managed with patient positioning, analgesics and fluids as indicated, and supportive care. • Symptoms of urinary tract infection include painful urination, frequent urges to urinate, difficulty urinating, and possibly referred pain in the shoulder or neck. The urine may have a foul odor and be cloudy. Management of patients with UTIs consists mainly of supportive care of the ABCs, allowing the patient to remain in a position of comfort, administering IV fluid, and possibly administering analgesics. • Catheterization of the bladder allows a continuous outflow of urine and provides a means of measuring urine output in hemodynamically unstable patients. To avoid backflow of urine, the drainage bag should not be lifted above the level of the patient’s bladder. • Kidney stones result when an excess of insoluble salts or uric acid crystallizes in the urine. Symptoms include severe flank pain that may migrate to the groin. The pain may produce a spike in blood pressure and pulse rate. • Acute renal failure is a sudden decrease in filtration through the glomeruli, resulting in a release of toxins into the blood. The three types of acute renal failure are prerenal, intrarenal, and postrenal. Signs and symptoms range from hypotension, tachycardia, dizziness, and thirst, to pain, oliguria, distended bladder, hematuria, and peripheral edema. • Chronic renal failure is progressive and irreversible inadequate kidney function. Nephrons become damaged, losing their functionality and causing a buildup of wastes and fluid in the blood. Symptoms can include an altered level of consciousness, lethargy, nausea, headaches, cramps, anemia, bruised skin, edema in the extremities and face, hypotension, tachycardia, and possibly seizures or coma. • Patients with acute or chronic renal failure require support of airway, breathing, and circulation; administration of medications to regulate acidosis, electrolyte imbalances, and fluid volume; and calm transport with psychological support. • If left untreated, acute or chronic renal failure will progress to end-stage renal disease, meaning that the kidneys have lost all ability to function. Toxic waste materials build up in the patient’s blood, leading to a multitude of potential signs and symptoms and possibly dysrhythmias. Prehospital care is supportive, including treating for shock and, under medical direction, regulating fluid imbalances, electrolyte abnormalities, and cardiovascular function. • Renal dialysis is a procedure for removing toxic wastes and excess fluid from the blood. Dialysis patients usually have a shunt through which they are connected to the dialysis machine. Such patients are vulnerable to problems such as hypotension, potassium imbalance, disequilibrium syndrome, and air embolism. • Always monitor dialysis patients for cardiac dysrhythmias. Shock secondary to bleeding is also possible from any number of causes. Watch for peaked T waves on the ECG. These are a classic sign of hyperkalemia. • When you find a shunt leaking during the dialysis cycle, attempt to tighten the connection. If it has become disconnected at the vein, clamp the cannula and disconnect the patient from the machine. • Specific conditions that may occur in the male genital tract include epididymitis, Fournier gangrene, priapism, phimosis, benign prostate hypertrophy, testicular masses, and testicular torsion. Prehospital management for most of these conditions is supportive. Because the patient is likely in pain, consider administering analgesics, and transport gently.