URINARY lecture notes
advertisement

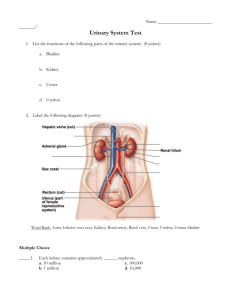
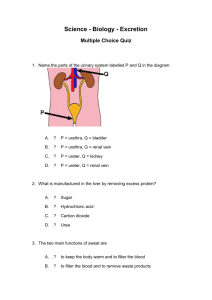
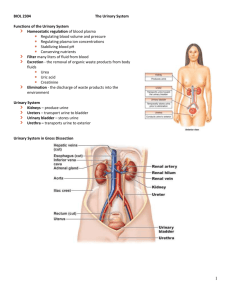
URINARY SYSTEM NOTES ZOO 200 1. Organs of the Urinary System a. Kidneys b. Ureters c. Bladder d. Urethra 2. Functions of the Urinary System a. Excretion of excess water, ions, and nitrogenous wastes b. Regulation of body fluid levels, solute concentrations, and pH of ECF 3. Other Organ Systems Involved with Excretion a. Integumentary System: excretes urea and NaCl b. Respiratory System: excretes CO2, H2O, and ketones (in diabetes) c. Digestive System: excretes bilirubin and H2O 4. Other Functions of the Kidney a. Assists in the production of vitamin D b. Produces erythropoietin 5. Kidney anatomy (when reviewing anatomy, refer to models and/or diagrams in the text) a. Location: retroperitoneal, high in the posterior abdominal cavity; partially protected by ribs b. Basic anatomy 1) Surrounded by a layer of adipose tissue; a renal capsule of dense CT forms its outer layer 2) Renal cortex: 1/2 inch layer just deep to capsule; made mostly of nephrons 3) Renal medulla: deep to the cortex; consists of alternating renal columns (composed of more nephrons) and renal pyramids (composed of collecting ducts and loops of Henle) 4) Calyces (pronounced “KAY-la-seez” and renal pelvis (a) Urine produced in nephrons passes into collecting ducts which travel down through a renal pyramid; collecting ducts converge at the tip of a pyramid in (a “renal papilla”) where they empty into a minor calyx (“KAY-licks”, singular form of “calyces”) (b) Two or more minor calyces converge to form a major calyx (c) Major calyces empty into a renal pelvis (d) Renal pelvis funnels urine into a ureter which carries urine to the urinary bladder 5) Note by looking at a model or diagram: the ureter, pelvis, major and minor calyces are all part of one continuous structure 6. Functional Unit of the Kidney: the nephron a. Each kidney contains around one million nephrons b. Structural components of the nephron 1)Bowman's capsule (surrounds the glomerlus; Bowman’s capsule plus the glomerulus form the renal corpuscle) 2)Proximal Convoluted Tubule 3)Loop of Henle (dips down into a renal pyramind) 4)Distal Convoluted Tubule -- empties into the collecting duct(aka collecting tubule) c. Nephron blood supply: afferent arteriole, glomerulus (where indiscriminate filtration of the plasma takes place — the filtrate enters Bowman’s capsule of the nephron), efferent arteriole, peritubular (“around the nephron”) capillary (into which selective reabsorption of much of what was initially filtered into the nephron occurs, including vitals like glucose and 99% of the filtered water; what isn’t completely reabsorbed, waste products such as urea for example, forms the urine) -2d. Juxtaglomnerular apparatus: formed where an afferent arteriole touches a distal convoluted tubule: secretes an enzyme, renin, into the plasma which helps to increase blood pressure whenever blood flow to the kidney decreases 7. Ureters a. Left and right muscular tubes, retroperitoneal b. Through peristaltic contractions of the ureter smooth muscle layer, urine is conveyed to the urinary bladder (pelvic cavity) c. Mucosa composed of transitional epithelium which allows stretching 8. Urinary bladder (located in the true pelvis) a. Muscular sac that temporarily stores urine; capacity: 600 to 800 ml; micturition point is between 150 and 300 ml b. Mucosa composed of transitional epithelium which allows stretching and is folded into rugae for same purpose c. Muscle layer is a smooth muscle called the detrusor muscle, which contracts during urination d. On the floor of the bladder is a flattened, triangular region of mucosa -- the trigone; at each corner of the trigone is an opening: 2 are for the ureters, 1 is for the urethra e. The detrusor muscle at the beginning of the urethra forms the internal urethral sphincter (smooth muscle and thus involuntarily controlled) 9. Urethra a. Tube lined with stratified squamous epithelium that drains urine to the outside b. About in inch from the bladder the urethra passes through the floor of the pelvic cavity (the urogential diaphragm) where a ring of skeletal muscle surrounds it – this is the external urethral sphincter and is voluntarily controlled 10. Urination (Micturition) a. Unconscious control: the micturition reflex (a spinal reflex) 1) Urine fills the bladder, stimulating stretch receptors 2) Sensory nerve impulses sent to sacral spinal cord 3) Integration of impulses occurs in the micturition reflex center 4) Autonomic (parasympathetic) motor nerve impulses sent to the detrusor muscle of the bladder wall and the internal urethral sphincter; the bladder contracts, the sphincter relaxes; urination begins (but only if the external urethral sphincter is also relaxed; see below) b. Conscious control 1) Motor impulses originate in the primary motor cortex of cerebrum 2) Axons from cortical neurons descend to the sacral region of the spinal cord, synapsing with motor neurons whose axons travel to the skeletal muscle cells of the external urethral sphincter. 3) Inhibitory motor impulses are sent to pelvic diaphragm, the urethra is no longer squeezed closed by the pelvic diaphragm; urination begins.