Basic ECG Interpretation
Christopher Wenger, DO
August 2012
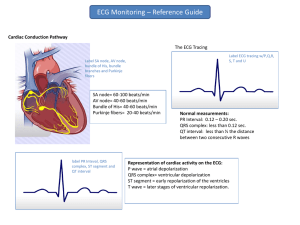
The Conduction System
The conduction system
http://www.unm.edu/~lkravitz/EKG/ekgdepolmyocyte.html
Nomenclature
Nomenclature
Waves
-P wave
-T wave
-U wave
Complex
-QRS
Segments
-PR segment
-ST segment
Intervals
-PR interval
-QT interval
Point
-J point
http://cal.vet.upenn.edu/projects/lgcardiac/ecg_tutorial/heartrate.htm
Putting it all together
(Conduction system + Nomenclature)
Atrial depolarization
(P wave)
Ventricular
repolarization
(T wave)
Time lag of impulse from
atrial depolarization to
onset of ventricular
depolarization
(PR segment)
Systole: QRS complex to end of T wave
Diastole: End of T wave to QRS complex
Plateau phase of
repolarization
(ST segment)
Ventricular
depolarization
(QRS complex)
Timing of the ECG Paper
Timing of the ECG paper
• 1 “little box” = 0.04 seconds (or 40 msec)
• 1 “big box” = 0.2 seconds (or 200 msec)
▫ 5 “little boxes” = 1 “big box”
▫ 5 “big boxes” = 1 second
http://www.unm.edu/~lkravitz/EKG/ekgpaper.html
Timing of the ECG paper
© 2012 UpToDate, Inc. All rights reserved
Timing of the ECG paper
Full standard: ECG was not reduced in size in order to fit on the paper
(10 mm/mV)
Half standard: ECG was reduced in size by 1/2 in order to fit on the paper (all
(5 mm/mV) deflections should be multiplied by two for proper interpretation)
Full/Half standard: The limb leads are in full standard, however the chest (precordial)
(10/5 mm/mV)
leads are in half standard.
Phase I: Rate, Rhythm, Axis
In what order do you read an ECG?
• 1st: What is heart rate (HR)?
▫ Normal, bradycardic, tachycardic
• 2nd: What is the QRS axis?
▫ Normal, left, right, extreme right (aka northwest)
• 3rd: What is the rhythm?
▫ Sinus, supraventricular, junctional, ventricular
Although there is no absolute particular order, YOU MUST
ALWAYS BEGIN YOUR ECG INTERPRETATION WITH THE
ABOVE 3 ASSESSMENTS!!!
Step 1: Heart Rate (defined)
• Normal
▫ 60 - 100 bpm
• Bradycardia
▫ <60 bpm
• Tachycardia
▫ >100 bpm
Step 1: Heart Rate (how to calculate)
• 4 ways to calculate HR:
▫ 1st: Memorize incremental box counts:
▫ 2nd: Divide 1500 by the # little boxes between RR interval
Example (above): 1500 / 20 little boxes = 75 beats/minute
▫ 3rd: Divide 300 by the # big boxes between RR interval
Example (above): 300 / 4 big boxes = 75 beats/minute
▫ 4th: Count # R waves on entire ECG strip and multiply by 6
Use this method when the rhythm is irregular
Step 2: QRS Axis (defined)
• Normal axis
▫ 0 ° to 105°
▫ -30 ° to 0° (normal variant)
• Right axis deviation
▫ +105 ° to +/-180°
• Left axis deviation
▫ -90° to -30°
• Extreme right axis deviation (aka Northwest axis)
▫ +/- 108° to -90°
Step 2: QRS Axis
http://www.unm.edu/~lkravitz/EKG/qrsaxisdetermine.html
Step 2: QRS Axis (how to determine)
Lead I:
Is R wave > S wave?
NO
YES
Lead aVF:
Is R wave > S wave?
Right axis deviation
NO
YES
Normal variant or Left
axis deviation
Normal axis
Lead II:
Is R wave > S wave?
YES
Hkjhkjhjhkjhkj
jhkh
Normal variant
NO
Left axis deviation
Step 3: Rhythms
•
•
•
•
•
Sinus rhythm
Premature beats
Supraventricular arrhythmias
Junctional rhythms
Ventricular rhythms
Step 3: Rhythms
• Sinus rhythms
▫ Normal sinus rhythm
▫ Sinus bradycardia/tachycardia
▫ Sinus arrhythmia
•
•
•
•
Premature beats
Supraventricular arrhythmias
Junctional rhythms
Ventricular rhythms
Sinus rhythm
Normal sinus rhythm
What makes a rhythm ‘sinus’?
-P wave axis is positive in the inferior leads (II, III, aVF)
-P wave morphology is the same
-Cadence is regular
Sinus rhythm is not strictly defined as a “P wave before every QRS”
Sinus rhythm
Sinus bradycardia
Heart rate is < 60 beats per minute (bpm)
-In this example, the HR is 55 bpm
(1500 / 27 = 55) or (300 / 5.3 = 56 bpm)
Sinus tachycardia
Heart rate is > 100 bpm
-In this example, the HR is 107 bpm
(1500 / 14 = 107) or (300 / 2.8 = 107 bpm)
Sinus rhythm
Sinus rhythm with sinus arrhythmia
Sinus arrhythmia
-Normal P wave morphology and axis
-Phasic change in P-P interval, usually in response to breath cycle
-Longest and shortest P-P intervals vary by >0.16 seconds or 10%
*This rhythm is typically seen with respiration due to fluctuations in
parasympathetic vagal tone
*Treatment is not usually required unless symptomatic bradycardia is present
Rhythms
• Sinus rhythm
• Premature beats
▫ Premature atrial contraction (PAC)
▫ Premature ventricular contraction (PVC)
▫ Fusion beat
• Supraventricular arrhythmias
• Junctional rhythms
• Ventricular rhythms
Sinus rhythm (with premature beats)
Sinus rhythm with PACs
Premature atrial contraction (PAC)
-P wave is abnormal in configuration and premature relative to the normal P-P interval
-QRS complex is usually similar in morphology to the QRS complex present during
sinus rhythm
Sinus rhythm (with premature beats)
Sinus rhythm with PVCs
Premature ventricular contraction (PVC)
-A wide, notched or slurred QRS complex that is:
~premature relative to the normal R-R interval, and
~not preceded by a P wave
-Note: a PVC contains a QRS that is almost always >0.12 seconds
-Note: Initial direction of the QRS is often different from the QRS during sinus rhythm
If the above telemetry strip had…..
-2 PVCs in a row = Sinus rhythm with a couplet
-3 PVCs in a row = Sinus rhythm with a triplet
-PVCs occurring every second beat = Sinus rhythm with bigeminy
-PVCs occurring every third beat = Sinus rhythm with trigeminy
Sinus rhythm (with premature beats)
Sinus rhythm with PVC and fusion beat
Fusion beat
http://www.lex-co.com
-Occurs when a supraventicular & ventricular impulse coincide to create a hybrid complex
~indicative of two foci of pacemaker cells firing simultaneously:
1. a supraventicular pacemaker (e.g. the sinus node), and
2. a competing ventricular pacemaker (source of ventricular ectopic activity)
Rhythms
• Sinus rhythm
• Premature beats
• Supraventricular arrhythmias
▫
▫
▫
▫
▫
Atrial fibrillation
Atrial flutter
Multifocal atrial tachycardia
Wandering atrial pacemaker
Supraventricular tachycardia
• Junctional rhythms
• Ventricular rhythms
Supraventricular rhythms: Atrial fibrillation
Atrial fibrillation
Atrial fibrillation (AF)
-P waves absent (no organized atrial depolarization)
~impulses are not originating from the sinus node
-Atrial activity is totally irregular and represented by fibrillatory waves of varying
amplitude, duration and morphology, causing random oscillation of the baseline
-The AV node allows some of the impulses to pass through at variable intervals
~ventricular rhythm is typically irregularly irregular
~ventricular rate is usually 100-180 bpm
Conditions that can mimic atrial fibrillation:
-Atrial flutter
-Multifocal atrial tachycardia (MAT)
Supraventricular rhythms: Atrial flutter
Atrial flutter
Atrial flutter
-Rapid regular atrial undulations (flutter waves)
~forms a classic “sawtooth” pattern
-Atrial rate of 250-350 bpm
-Ventricular rate depends on conduction via the AV node to the ventricles
~the reentrant pathway in the right atrium with every 2nd, 3rd, or 4th impulse
generates a QRS (while the others are blocked in the AV node as the node
repolarizes
Supraventricular rhythms: Multifocal atrial
tachycardia & Wandering atrial pacemaker
Multifocal atrial tachycardia
Multifocal atrial tachycardia (MAT)
-P waves with ≥3 morphologies (each originating from a separate atrial focus)
-Atrial rate typically 100-150 bpm
-Irregular rhythm with varying PP and PR intervals
-Isoelectric baseline between P waves (i.e. no flutter waves)
-P waves may be blocked (i.e. not followed by a QRS complex)
Wandering atrial pacemaker
Wandering atrial pacemaker (WAP)
- P waves with ≥3 morphologies (just like MAT, however HR is <100 bpm)
Supraventricular rhythms: SVT
SVT
SVT
-Regular rhythm
-HR >100 bpm
-QRS duration is normal
-P wave often buried in QRS complex or preceding T wave
-Impulses stimulating the heart are not being generated by the sinus node, but instead
are coming from a collection of tissue around and involving the AV node
Rhythms
•
•
•
•
Sinus rhythm
Premature beats
Supraventricular arrhythmias
Junctional rhythms
▫ Junctional rhythm
▫ Accelerated junctional rhythm
▫ Junctional tachycardia
• Ventricular rhythms
Junctional rhythms: Junctional rhythm
Junctional rhythm
Junctional rhythm
-P wave may proceed, be buried in, or follow the QRS complex
-QRS is narrow; RR interval is usually regular
-HR 40-60 bpm
~if HR 60-100 bpm, then the rhythm is called Accelerated junctional rhythm
~if HR >100 bpm, then the rhythm is called Junctional tachycardia
Junctional rhythms: Accelerated junctional
rhythm/Junctional tachycardia
Accelerated junctional rhythm
Accelerated junctional rhythm
-Same as Junctional rhythm, however HR is now 60-100 bpm
Junctional tachycardia
Junctional tachycardia
-Same as Junctional rhythm, however HR is now >100 bpm
Rhythms
•
•
•
•
•
Sinus rhythm
Premature beats
Supraventricular arrhythmias
Junctional rhythms
Ventricular rhythms
▫
▫
▫
▫
Accelerated idioventricular rhythm (AIVR)
Ventricular tachycardia (VT)
Ventricular fibrillation (VF)
Torsade de pointes
Ventricular rhythms: Accelerated idioventricular
rhythm (AIVR)
Accelerated idioventricular rhythm
Accelerated idioventricular rhythm (AIVR)
-Regular or slightly irregular ventricular (wide complex) rhythm
-HR of 60-110 bpm
-QRS morphology similar to PVCs
*Tip: Think of this rhythm as a slow ventricular tachycardia (VT)
[however unlike VT, AIVR is not associated with an adverse prognosis]
Ventricular rhythms: Ventricular tachycardia (VT)
Ventricular tachycardia
Ventricular tachycardia (VT)
-Rapid succession of ≥3 ventricular premature complexes at a rate >100 bpm
-This rhythm originates in the ventricles (thus no P waves and wide QRS)
-R-R interval is usually regular
-Abrupt onset and termination of arrhythmia is evident
-AV dissociation is common
*This is a lethal arrhythmia!
Ventricular rhythms: Ventricular fibrillation (VF)
Ventricular fibrillation
Ventricular fibrillation (VF)
-Extremely rapid and irregular ventricular rhythm demonstrating:
~chaotic and irregular deflections of varying amplitude and contour
~Absence of distinct P waves, QRS complexes, and T waves
*This is a lethal arrhythmia!
Ventricular rhythms: Torsade de pointes (TdP)
Ventricular tachycardia
Torsade de pointes (TdP)
-Type of polymorphic ventricular tachycardia (VT)
~initiated in the presence of a long QT interval
-HR 240-300 bpm
-progressive reduction of QRS amplitude with reversal that occurs cyclically
~creates an oscillating apperance around the isoelectric line
-AV dissociation present
*This is a lethal arrhythmia!
Phase II: Conduction Blocks
Conduction Blocks
• Sinoatrial exit blocks
▫ 1st degree SA block
▫ 2nd degree SA block
Type (Mobitz) I SA block
Type (Mobitz) II SA block
▫ 3rd degree SA
• AV blocks
▫ 1st degree AV block
▫ 2nd degree AV block
Type (Mobitz) I or Wenckebach AV block
Type (Mobitz) II AV block
▫ 3rd degree AV block (Complete heart block)
• Bundle branch blocks
▫ Right bundle branch block (RBBB)
▫ Left bundle branch block (LBBB)
Left anterior fasicular block (or left anterior hemiblock)
Left posterior fasicular block (or left posterior hemiblock)
Conduction Blocks
• Sinoatrial exit blocks
▫ 1st degree SA block
▫ 2nd degree SA block
Type (Mobitz) I SA block
Type (Mobitz) II SA block
▫ 3rd degree SA
• AV blocks
• Bundle branch blocks
Conduction blocks: Sinoatrial exit blocks
1st degree SA block
-Delay between impulse generation and transmission to the atrium
-Not detectable on a surface ECG
2nd degree SA block, Type (Mobitz) I
2nd degree SA block, Type (Mobitz) I
-P wave morphology and axis consistent with a sinus node origin
-”Group beating” with:
~progressive shortening of PP interval up to pause
~constant PR interval
~PP pause <2x the normal PP interval
-Progressive lengthening of the interval between impulse generation and transmission,
culminating in failure
~the gradually lengthening transmission interval pushes successive P waves
closer together which results in grouping of the P-QRS complexes
Conduction blocks: Sinoatrial exit blocks
2nd degree SA block, Type (Mobitz) II
2nd degree SA block, Type (Mobitz) II
-Constant PP interval followed by a pause that is a multiple (e.g. 2x, 3x, etc.) of the normal
PP interval
~pause may be slightly less than 2x the normal P-P interval (usually within 0.10 seconds)
3rd degree SA block
-No sinus impulses are conducted to the right atrium (complete sinoatrial failure)
~complete absence of P waves
~rhythm may be maintained by a junctional escape rhythm
~indistinguishable on ECG from sinus arrest
Conduction Blocks
• Sinoatrial exit blocks
• AV blocks
▫ 1st degree AV block
▫ 2nd degree AV block
Type (Mobitz) I or Wenckebach AV block
Type (Mobitz) II AV block
▫ 3rd degree AV block (Complete heart block)
• Bundle branch blocks
Atrioventricular (AV) blocks
1st degree AV block
1st degree AV block
-PR interval ≥0.20 seconds
-Each P wave is followed by a QRS complex
*Remember: the PR interval represents the time from the onset of atrial depolarization to the
onset of ventricular repolarization
Atrioventricular (AV) blocks
2nd degree AV block, Mobitz I
2nd degree AV block, Type (Mobitz) I
-Progressive prolongation of the PR interval and progressive shortening of the RR interval
until a P wave is blocked
~RR interval containing the nonconducted P wave is less than 2 PP intervals
*This type of block occurs at the level of the AV node, thus has narrow QRS complex
Atrioventricular (AV) blocks
2nd degree AV block, Mobitz II
2nd degree AV block, Type (Mobitz) II
-Regular rhythm with intermittent nonconducted P waves and no evidence for atrial
prematurity
-PR interval in the conducted beats is constant
-RR interval containing the nonconducted P wave is equal to two PP intervals
*This type of block typically occurs below the bundle of His, thus has wide QRS complex
(80% of cases)
Atrioventricular (AV) blocks
3rd degree AV block
3rd degree AV block
-Atrial impulses consistently fail to reach the ventricles, resulting in atrial and ventricular
rhythms that are independent of each other
-PR interval varies
-PP and RR intervals are constant
-Atrial rate >> Ventricular rate
-Ventricular rhythm is maintained by a junctional or idioventricular escape rhythm or a
ventricular pacemaker
*Note: If Atrial rate << Ventricular rate, then the rhythm is called AV dissociation
Conduction Blocks
• Sinoatrial exit blocks
• AV blocks
• Bundle branch blocks
▫ Right bundle branch block (RBBB)
▫ Left bundle branch block (LBBB)
Left anterior fasicular block (or left anterior hemiblock)
Left posterior fasicular block (or left posterior hemiblock)
Bundle branch blocks
http://www.cvphysiology.com
Bundle branch blocks
r wave
R’ wave
S waves
Right bundle branch block (RBBB)
-Prolonged QRS duration (≥0.12 seconds)
-Secondary R wave (R’) in leads V1 and V2 (rsR’ or rSR’) with R’ usually taller than the initial
R wave
-Typically have wide slurred S wave in leads I, V5, and V6
*Incomplete RBBB = when RBBB criteria are met, but the QRS duration is 0.10-0.12 seconds
Bundle branch blocks
rS complex
Broad monophasic R waves
Left bundle branch block (LBBB)
-Prolonged QRS duration (≥0.12 seconds)
-Broad monophasic R waves in leads I, V5, V6 that are usually notched or slurred
-Secondary ST & T wave changes opposite in direction to the major QRS deflection
-rS or QS complex in right precordial leads
*Incomplete LBBB = when LBBB criteria are met, but the QRS duration is 0.10-0.12 seconds
Bundle branch blocks
rS complex
Left anterior fascicular block (hemiblock)
-Left axis deviation with mean QRS axis between -45° and -90°
-qR complex (or an R wave) in leads I and aVL
-rS complex in lead III
-No other factors responsible for left axis deviation
qR complex
Bundle branch blocks
S wave
Q wave
Right axis
deviation
Left posterior fascicular block (hemiblock)
-Right axis deviation with mean QRS axis between +100° and +180°
-Q waves in lead III
-S waves in lead I
-No other factors responsible for right axis deviation
*Compared to the left anterior fascicule, the left posterior fascicle is shorter, thicker, and receives
dual blood supply (from the LAD and RCA ); thus more rare
*CAD is the most common cause of LPFB; when it develops during AMI, MV-CAD and extensive
infarction are typically present and prognosis is poor
Phase III: Intervals,
Hypertrophy, Infarction
Intervals
• Length of PR interval
• Length of QRS complex
• Length of QT interval
Intervals: PR
< 0.12 seconds
0.12 – 0.20 seconds
>0.20 seconds
Pre-excitation
Normal
AV nodal blocks
(i.e. Wolff-Parkinson-White)
Intervals: QRS
≤ 0.10 seconds
0.10 – 0.12 seconds
>0.12 seconds
Normal
Incomplete bundle branch
block
Bundle branch block
PVC
Ventricular rhythm
Pictured: Incomplete RBBB
Pictured: Sinus rhythm with PVC
Intervals: QT
• Proportional to heart rate:
▫ Slower HR = Longer QT interval
▫ Faster HR = Shorter QT interval
• To calculate accurate QT interval (taking into account HR),
you must calculate the corrected QT interval (QTc):
▫ Bazett’s formula:
QTc = QT / square root of R-R interval
▫ Quick tip: Instead of calculating a QTc, you can perform a quick
estimate to determine if the QT interval is normal or
prolonged:
A QT interval > half of the R-R interval is probably prolonged
Intervals: QT
≤ 0.44 seconds
> 0.44 seconds
Normal
Prolonged QT interval
Pictured: Prolonged QT interval
Pictured: Torsade de Pointes
Hypertrophy
• Types:
▫
▫
▫
▫
Right atrial abnormality (RAA)
Left atrial abnormality (LAA)
Right ventricular hypertrophy (RVH)
Left ventricular hypertrophy (LVH)
• Note:
▫ To determine atrial abnormality, analyze the P waves
▫ To determine ventricular hypertrophy, analyze the QRS
complex
▫ We use the term ‘abnormality’ instead of ‘enlargement’ when
referring to the atria since an ECG reflects augmentation of
electrical current only (and not necessarily the actual size of the
chamber)
Hypertrophy: RAA
Alpaslan, Dr. Mete. doktorekg.com
Diagnostic criteria:
1. Lead II, III, and aVF: P wave >2.5 mm, or
2. Lead V1 or V2: P wave >1.5 mm
*Remember: 1 small box = 1 mm
Hypertrophy: LAA
Alpaslan, Dr. Mete. doktorekg.com
Diagnostic criteria:
1. Lead V1: P wave ≥1 mm deep and ≥0.04 seconds in duration
(1 small box deep and one small box wide), or
2. Lead II, III, or aVF: Notched P wave with duration of ≥0.12 seconds
(P-mitrale)
Hypertrophy: RVH
Diagnostic criteria:
Lifeinthefastlane.com. Aug 2012
1. Right axis deviation
2. Dominant R wave:
R/S ratio in V1 or R/S ratio in V5 or V6 ≤1
R wave in V1 ≥7 mm
R wave in V1 + S wave in V5 or V6 >10.5 mm
Hypertrophy: LVH
Diagnostic criteria (any of the following):
Lifeinthefastlane.com. Aug 2012
1. Cornell Criteria (most accurate):
R wave in aVL + S wave in V3: >28 mm (male), >20 mm (female)
2. Maximum R wave + S wave in precordial leads >45 mm
3. R wave in V5 >26 mm
4. R wave in V6 >20 mm
Infarction
• When assessing for infarction, take note of the
following:
▫ Abnormal Q waves
▫ ST segment deviation (elevation or depression)
▫ Peaked, flat, or inverted T waves
• Acute MI ECG diagnostic criteria:
▫ ST segment elevation or depression of ≥1 mm in ≥2
contiguous leads
Infarction (Q waves)
Normal (non-pathologic) Q wave: note that the Q
wave is both shallow and brief
http://www.medicine-on-line.com
Pathologic Q waves: >40 ms or deeper than 1/3 the
height of the entire QRS complex
http://www.medicine-on-line.com
*Tip: Pathologic Q waves = infarction (however they
do not tell you if the infarct is acute, sub-acute, or old!
(the timing is determined by the ST segment)
Infarction (ST segments)
Transmural MI = Q wave MI = STEMI
(note Q wave and ST segment elevation
>1 mm)
http://www.medicine-on-line.com
Subendocardial MI = Non-Q wave MI = NSTEMI
(note absence of Q waves; ST segment
depression >1 mm)
http://www.medicine-on-line.com
Infarction (ST segments)
Acute inferior wall STEMI
Infarction (T waves)
Hyperacute (tall positive) T waves:
-T waves may precede ST segment elevation (A), or
-T waves may be seen with ST elevation during the acute
phase (B)
http://www.medicine-on-line.com
Infarction (coronary artery
distribution)
Peter J. Zimetbaum, M.D., and Mark E. Josephson, M.D. Use
of the Electrocardiogram in Acute Myocardial Infarction N
Engl J Med 2003; 348:933-940March 6, 2003
Infarction (Timing)
Emerg Med Clin N Am 2006; 24:53-89
Abnormal Q waves….
-with ST segment elevation/depression = acute MI
-without ST segment changes and normal T wave = old MI
-without ST segment changes and inverted T wave = MI of undetermined age