BASIC ECG INTERPRETATION
advertisement
ECG Basics Module 2( Arrhythmias
level 1)
Dr. Jeffrey Elliot Field, HBSc. DDS,
Fellow, American Dental Society of Anesthesia
Diploma, the National Dental Board of Anesthesia.
1
4/13/2015
OBJECTIVES
TO LEARN TO INTERPRET BASIC ARRYTHMIAS
4/13/2015
3
Lets Review What an ECG Is.
An ECG is a recording of the electrical activity within heart
muscle.
Heart muscle unlike other muscle can contract without a
an external nerve input or action potential.
The interesting thing about cardiac muscle is:
it can depolarize as the result of adjacent cells depolarizing. Like a wave
in the crowd at a football game.
Pacemaker cells can spontaneously depolarize as a result of spontaneous
intracellular mechanisms.
All other muscle cells only depolarize as the result an external
mechanism ( motor neuron stimulation)
This depolarization and repolarization cycle is what we see
on an ECG
Basic Cardiac Physiology
The pacemaker sites within the heart are the SA node,
AV node and Purkinge fibers in the heart.
As discussed earlier each pacemaker site within the
heart has its own unique firing rate.
As a result the heart rate can often be a clue as to
which pacemaker is in charge at that point in time. (
see diagram on next slide)
4/13/2015
6
HOW TO READ A THREE
LEAD RYTHYM STRIP
4/13/2015
7
The 3 Steps In ECG Determination
Are:
1) Establish whether are not there
is there electrical activity.
2)Rate determination.
3) Rhythm identification.
4/13/2015
8
STEP 1
IS THERE ANY ELECTRICAL ACTIVITY?
IF NO ACTIVITY IS SEEN YOU MUST FIRST
CHECK THE LEADS ARE ADHERING TO THE
SKIN AND ALL CONNECTIONS ARE INTACT.
IF THE CONNECTIONS ARE ALL OK, THEN
CHECK THE PULSE. IF NO PULSE EXISTS AND
IF EVERYTHING IS HOOKED UP PROPERLY
AND THERE IS NO ELECTRICAL ACTIVITY
,THEN A DIAGNOSIS OF ASYSTOLE IS MADE.
4/13/2015
9
Note: In asystole the straight baseline
wanders. If a true straight line exists
this usually indicates that a lead has
come loose.
10
4/13/2015
P wave Asystole
In this case asystole exists even though there is P
wave electrical activity . Please note that there is NO
ventricular activity and therefore NO blood Flow.
11
4/13/2015
AGONAL RYTHYM
This is another example of asystole in which the
heart displays the last moments of it’s electrical
activity. This rhythm is also called dying heart.
4/13/2015
12
To REVIEW , THESE ARE THE THREE FORMS
OF ASYSTOLE
4/13/2015
13
Step 2 Basic Rhythm Determination
Next if there is electrical activity is there a
rhythm ?
If there is no rhythm then think about ventricular
fibrillation ( V-fib).
V-fib can be categorized as follows:
4/13/2015
Fine V-fib
Coarse V-ifib
Torsades De Pointes ( twisting pointes)
14
Fine V-Fib
4/13/2015
15
Coarse V-fib
4/13/2015
16
Torsades de pointes ( twisting
points)
This is often a sign of
hypomagnesemia
( low magnesium)
4/13/2015
17
What,s really
happening in
V-Fib ?
4/13/2015
18
Immediate action is required!!!
4/13/2015
19
STEP 2
RATE DETERMINATION
4/13/2015
20
HOW TO EVALUATE TIME/RATE ON
STANDARD ECG PAPER
4/13/2015
There are 15 large boxes in every 3 seconds
21
Since the ECG paper moves at 25
mm/second and therefore 25 of the 1.0
mm ( small)boxes or 5 of the big boxes
pass in one second.
Therefore 1 small box = 0.04 seconds
and 5 small boxes or 1 big box =0.20
seconds( as discussed in module1).
Now you have all the information you
need to calculate rates
4/13/2015
22
There Are 3 Methods To Determine
Rate
1) Counting the R-waves per
minute with respect to the large
boxes on the ECG paper.
2)Quick rate determination
) Counting R-waves per minute
with respect to small boxes on
the ECG paper.
QUICK METHOD FOR RATE
DETERMINATION.
It is possible to now calculate rate by counting the
number of R waves in one minute. However this is very
tedious and time consuming.
The quick method involves memorizing the following
chart which entails counting the number of large
boxes ( i.e. 5 small boxes) between R waves.
4/13/2015
24
Quick Method of Rate
Determination
Number of large boxes between R-waves
1 2 3 4 5 6 7 8 9 10
4/13/2015
25
A final method is to count the
number of small ( 1.0mm) boxes
between 2 consecutive R waves
and divide this into 1500.
4/13/2015
26
CAN YOU DETERMINE THIS RATE?
4/13/2015
75 bpm
27
RATE NOMENCLATURE
Normal heart rates are from 60-100
beats per minute.
Rates above 100 are termed
tachycardia.
Rates below 60 are termed
bradycardia.
4/13/2015
28
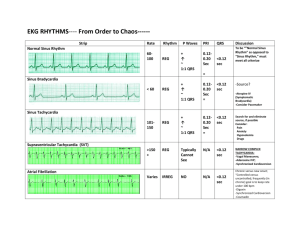
Tachycardias
Tachycardia's can be divided into two groups.
-Supraventricular are tachycardia's in which the pacemaker site is
above the AV node. In this case the QRS width is normal (under
0.12 seconds or 3 small boxes)
Supraventricular tachycardia's are:
Paroxysmal super ventricular tachycardia( an SVT that comes
and goes)
Supraventricular tachycardia( a sustained SVT)
Atrial flutter( a characteristic type of sustained SVT)
Ventricular Tachycardia's ( also called wide complex tachycardia's)
are tachycardia’s in which the pacemaker lies below the AV node. In
this case the QRS width is prolonged. (over 0.12 seconds or 3 small
boxes)
4/13/2015
29
Superventricular Tachycardia
Atrial Flutter ( Note the characteristic
sawtooth pattern)
4/13/2015
30
Classic Ventricular Tachycardia ( VTACH)
Ventricular Tachycardia with Capture Beats( see ). That is there are quasi
normal beats interspersed between the wide complex beats.
4/13/2015
31
Clinical Relevance of Tachycardias
With each heart beat blood is ejected from the
ventricles .
70% of the refill of the ventricles is passive. That is
after the ventricle squeezes the blood out it relaxes
and blood is passively drawn in.
The final 30% of ventricular filling is the result of
active pushing of blood from the atria ( also called
the atrial kick) . With atrial flutter and atrial
fibrillation you loose the atrial kick.
4/13/2015
32
also as the rate increases the time available for passive
ventricular filling is decreased.
therefore less and less blood is moved which leads to a
decrease in the pulse or even loss of the pulse.
In this case the organs and tissue receive little or no
blood and in turn little or no oxygen.
With atrial flutter and atrial fibrillation the loss of the
atrial kick ends in poor tissue perfusion. This is also
called a loss of perfusion pressure.
33
4/13/2015
Rhythm Determination
STEP 3 IS TO DETERMINE THE RYTHYM
This is done by looking at the following factors.
-Is the rhythm regular or irregular
-Is the QRS complex width normal or prolonged
-Is atrial activity present and if present how does the
atrial activity relate to the ventricular activity
4/13/2015
35
IS THE RYTHYM REGULAR OR IRREGULAR
Look at the R-R intervals and see if they all are the
same.
If so the rhythm is regular.
If not, is the rhythm totally irregular ? {“ irregularly
irregular”}
or is there cyclical variation (i.e. the pattern is irregular
but repeats)
4/13/2015
36
Use calipers to mark out the R-R interval
and see if it repeats. If it does, it’s a regular
rhythm and if it doesn’t, it is irregular.
4/13/2015
37
Regular Rhythms
4/13/2015
38
Sinus Rhythm
4/13/2015
Diagnosis of Sinus Rhythm
1) P-waves are present, upright and precede each QRS complex
2) The P-R interval is normal (0.12-2.0 seconds)
3) QRS complexes are of normal (less than o.12 seconds) size and
morphology( no pathologic Q waves-see later module)
4) The Q-T interval is normal in duration ( around 10 small boxes based
on rate-see later discusson on the QT interval)
5) The T-wave is upright
39
Paced Rhythm
Note the pacer spikes which generate a QRS complex
4/13/2015
40
Irregular Rhythms
IRREGULARLY IRREGULAR Rhythm
This is always atrial fibrillation.
In this case the atrial cells are firing off in a non
coordinated pattern which causes the atria to quiver
rather than contract. This of course moves NO BLOOD.
Blood still however moves between the atria and
ventricles but only via passive filling such that you loose
the 30% of ventricular filling given by the atrial kick.
Different pacemaker sites within the atria in random
order cause ventricular depolarization, which leads to
the irregularly irregular rhythm.
4/13/2015
42
Atrial fibrillation
Note there are no P-waves.
You can see QRS complexes but there is NO
PATTERN to the R-R interval. That is each RR interval is different. Hence the rhythm is
irregularly irregular.
4/13/2015
43
OTHER CAUSES OF IRREGULAR, BUT
CYCLICALLY REPEATING RYTHYMS
Ectopic beats such as:
-PVC’s ( Premature ventricular contractions).
-Junctional Escape rhythms
PAC’s ( Premature atrial contactions) -Escape
beats where a pacemaker in the atria other than
the SA node generates the beat.
Heart Blocks or AV nodal blocks
4/13/2015
44
PVC’s Classification
PVC’s are a premature ventricular contraction. That is
the ventricle contracts on its own, without receiving a
signal from the SA node.These are classified as follows:
1)UNIFOCAL
( originating from the same site in the ventricle).
Therefore all PVC’s look exactly alike.
2) MULTIFOCAL( originating from different sites in the
ventricle). Such that the PVC’s have different
morphologies.
3) PVC Nomenclature: BIGEMINY ( one normal beat
alternating with a PVC) , TRIGEMINY two normal beats
followed by a PVC) etc .
45
4/13/2015
Examples of
Unifocal and
Mutifocal PVC’s
4/13/2015
46
Unifocal PVC ( both PVC’s look
alike)
4/13/2015
↑
↑
47
Multifocal PVC’s ↑ ( with run of unifocal
PVC’s) (↑ run of unifocal PVC’s)
↑ ↑↑↑ ↑
4/13/2015
Why are PVC’S Important?
4/13/2015
49
The Answer is the R on T Phenomenon
In these cases if a PVC’s R-wave falls on the previous
QRS’s T-wave, this can generate a run of ventricular
fibrillation.
This usually is not an issue with single unifocal PVC’s
but becomes a worry in cases with multifocal PVC’s or
runs of unifocal PVC’s. In these cases you should treat
the PVC’s with either lidocaine or amiodarone.
4/13/2015
50
R on T Phenomenon triggering
course V-fib.
↑
note the triggered run of V-fib
4/13/2015
51
Junctional Beats
and Rhythms
4/13/2015
52
Junctional Beats
Note the lack of a P-wave
↑ in the junctional escape beat.
This signifies a lack of atrial depolarization associated with this beat.
In other words this beat originated at or just above the AV node
because the QRS width is normal but there is no P-wave.
4/13/2015
53
Junctional Rythms
Note the slow rate and lack of a P-wave. This rhythm is being
generated in or just below the AV-node as evidenced by the
widened QRS complex and lack of a P-wave.
Premature Atrial Contraction
This occurs when a pacemaker in the atria
other than the SA node initiates an impulse.
This results in 2 possible phenomenon:
1) A QRS complex is produced by the PAC
2) A QRS complex is not produced by the PAC
In either case there is usually some pause in the
rhythm following the PAC.
4/13/2015
55
Why Is There A Pause In The
Cycle ?
The ectopic P-wave generates a QRS
complex such that when the normal pwave occurs, the ventricle is in its
refractory phase and cannot produce a
QRS complex.
That is why there is a pause in the
cycle.
4/13/2015
56
PAC
Pause
In this Case the PAC generates a QRS complex but there is a
pause in the cycle following the PAC
4/13/2015
57
The Fates of PAC’s
4/13/2015
58
Heart Blocks
Heart Blocks.
Know When To Be Concerned!!!
There are 3 types of heart blocks, also called AV blocks
( AV refers to the AV node):
First degree heart block/AV block.
Second degree heart block/AV block. Second degree
heart block has 2 subdivisions.
Second degree block type one( also called Mobitz One).
Second degree block type two (Als0 called Mobitz Two).
Third degree heart block/AV block.
Know When To Be Concerned!!!
First degree and second degree
type 1 blocks are usually very
stable and are not of much
concern.
Alternatively second degree type 2
and third degree heart blocks are
of great concern.
Know When To Be Concerned!!!
Second degree type 2 blocks can
deteriorate to third degree blocks.
Third degree blocks require
immediate pacing in most
instances as they only support rates
of under 40-60 bpm and usually are
more in the 40s.
How to Diagnose
Heart Blocks
First DEGREE AV BLOCK
In First degree AV Block there is a constant
prolongation of the PR interval above 0.20 seconds or
5 small boxes. This is a fixed conduction block such
that the P-R interval does not vary beat to beat.
Remember the PR interval is measured from the
beginning of the P-wave to the beginning of the Qwave.
First degree heart block is usually not of great concern
clinically.
4/13/2015
64
First degree Heart Block
Note the P-R interval is actually 9 small
boxes which equals 0.36 sec not 0.35 as the
65
author of the image notes.
4/13/2015
Second Degree AV block
(Types 1 and 2)
1. Type 1 (Mobitz 1) heart block.
2. Type 2 (Mobitz 2) heart block.
66
4/13/2015
Type 1 “Mobitz 1” Block
Almost always a disease of the AV Node
With 2nd degree type 1 heart block there is
progressive prolongation of the P-R interval
beat to beat until a beat is dropped.
Once the beat is dropped the PR interval
returns to normal or almost normal and the
cycle repeats.
67
4/13/2015
Second Degree Heart Block Type 1
Note the progressive lengthening of the PR
intervals, before a beat is dropped.
68
4/13/2015
Second degree heart block
type 1 if stable is similarly not
of great concern but no
treatment should be provided
without first consulting the
patient’s physician.
4/13/2015
69
Second Degree Heart Block Type 2 “Mobitz
2” Block
Second degree heart block type 2 is almost
always a disease of the distal conduction
system (His-Purkinge System).
Second degree heart block type 2 is
characterized by a fixed conduction block (
increased PR Interval that is stable ,beat to
beat) with dropped beats.
Second degree heart block type 2 is also
named or classified for the degree of
blockade( i.e. the number of propagated
beats).
70
4/13/2015
Mobitz Type 2 with a 2:1 heart block
( only every second beats is propogated)
Non propogatedP-waves
Mobitz Type 2 with a 3:1 heart block ( every third
beat is propogated)
4/13/2015
71
Second degree heart block type
2 is of great concern as these
often deteriorate into Third
degree heart block (Complete
Heart Block)
72
4/13/2015
Third Degree Heart Block
The impulse generated in the atria does
not propagate to the ventricles.
So, there is a complete dissociation of
the P-waves and the R-waves.
The P-waves occur at regular intervals
and seem to “March through the R
waves”.
73
4/13/2015
↑
↑
↑
↑
↑
↑
↑
↑
↑
Note the p-waves (↑) are marching through at regular intervals even
at times being buried(↑) in the QRS complexes. There is no
association between the p-waves and the QRS complexes. (see red arrows)
4/13/2015
74
With third degree heart block
The ventricles are contracting at their
own inherent rate of 20-40 beats per
minute
This often is a life threatening occurrence
as this rate usually fails to maintain an
adequate perfusion pressure( adequate
perfusion is when blood flow maintains
adequate tissue oxygenation)
These patients usually require immediate
pacing.
75
4/13/2015
Where do heart blocks occur?
4/13/2015
76
END OF PRESENTATION
Thank you for your commitment to continuing
education