1377891403-ECG_Job_aid
advertisement
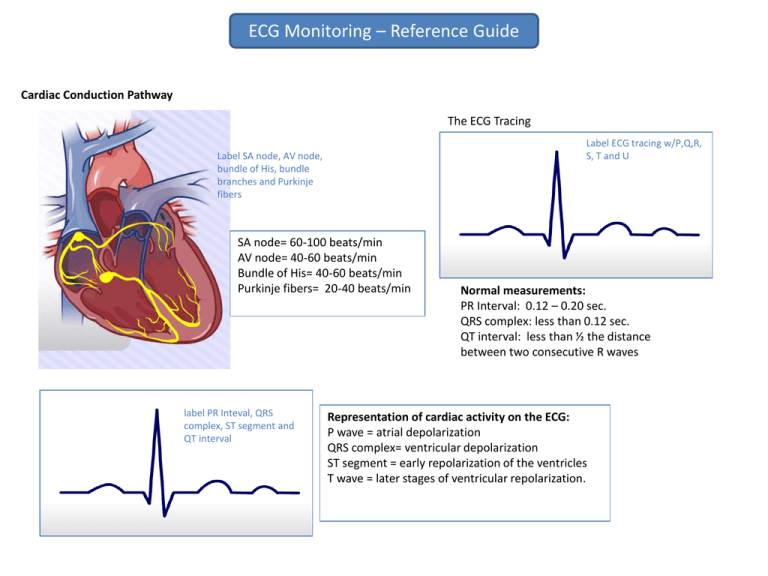
ECG Monitoring – Reference Guide Cardiac Conduction Pathway The ECG Tracing Label ECG tracing w/P,Q,R, S, T and U Label SA node, AV node, bundle of His, bundle branches and Purkinje fibers SA node= 60-100 beats/min AV node= 40-60 beats/min Bundle of His= 40-60 beats/min Purkinje fibers= 20-40 beats/min label PR Inteval, QRS complex, ST segment and QT interval Normal measurements: PR Interval: 0.12 – 0.20 sec. QRS complex: less than 0.12 sec. QT interval: less than ½ the distance between two consecutive R waves Representation of cardiac activity on the ECG: P wave = atrial depolarization QRS complex= ventricular depolarization ST segment = early repolarization of the ventricles T wave = later stages of ventricular repolarization. ECG Monitoring – Guide to Leads View of the heart provided by each lead: 264 Area Lead Lateral I, AVL (high lateral) V5, V6 (low lateral) Inferior Wall Anterior Wall Septum II, III, AVF. V1-V4/ V2-V4 V1, V2. American Heart Association’s standard color coding for ECG leads Location Inscription Color Right Arm Left Arm Right Leg Left Leg RA LA RL LL White Black Green Red Chest V1 Brown Lead placement for 5 lead ECGs Lead placement mnemonic: White is right. Snow over trees (white over green). Smoke over fire (black over red). Chocolate (brown) is close to the heart. ECG Monitoring – 5 Step Analysis Step 1: Assess the regularity of the rhythm Are the P waves (for atrial rhythm) or the R waves (for ventricular rhythm) consistently equidistant from each other? If there is a variation of more than 3 small boxes (0.12 seconds), the rhythm is considered irregular. Step 2: Calculating the heart rate The Six-Second Method This method can be used to easily measure the heart rate in nonregular rhythms. To calculate the ventricular rate, simply count the number of QRS complexes in a 6 second strip and multiply by 10. To calculate the atrial rate, count the P waves instead of the QRS complexes. The Large Box Method For this method, count the number of large boxes between two sequential R or P waves. Divide this number into 300 to obtain the rate. The Square Counting, or Sequence, Method The square counting method can be used for regular heart rhythms. First, find an R wave that falls on a thick line. The next thick lines will be counted as follows: 300, 150, 100, 75, 60, 50, 43, 37. Stop the sequence at the next R wave. If the second R wave falls between two thick lines, use the mean of the two numbers (for example, if the R wave falls between 150 and 100, the rate would be 125) The Small Box Method Count the small boxes between two sequential R waves (for the ventricular rate) or two sequential P waves (for the atrial rate). Divide this number into 1500 to obtain the rate. ECG Monitoring – 5 Step Analysis 3rd Step: Assessment of the P waves The P wave represents atrial depolarization. 4th Step: Assessment of the PR interval An absent P wave indicates that the electrical impulse is being generated from somewhere other than the SA node. The PR interval reflects the total time it takes for the electrical impulse to travel from the SA node through the AV node into the ventricles. An inverted P wave can be seen with ectopic atrial and junctional rhythms. A shortened PR interval (> 0.12 seconds) can indicate a junctional rhythm where the impulse originates in the AV junction, or an abnormal conduction pathway. Peaked P waves may be seen with right atrial enlargement, usually due to pulmonary hypertension A prolonged PR interval indicates that the impulse is being delayed before entering the ventricles. This is called first degree block and can be caused by myocarditis, acute myocardial infarction, hyperkalemia, medication effects, AV septal defects and enhanced vagal tone. Notched P waves can be seen with left atrial enlargement, usually due to mitral stenosis. (#2b) Variable P waves are indicative of multifocal atrial rhythms (meaning multiple sites within the atrium or AV junction are acting as ectopic pacemakers). 5th Step: Assessment of the QRS Complex The fifth step is to assess the QRS complex. The QRS complex represents ventricular depolarization. As with the PR interval, the QRS complex needs to be assessed for both duration (width) and consistency. The QRS can be classified as narrow (<0.10 sec) or wide (>0.12 sec). An abnormally wide QRS complex can indicate a delay or abnormality in conduction through the ventricle. Causes of wide QRS complexes can include bundle branch blocks, Wolff-Parkinson White syndrome, hyperkalemia, medication effects, and ventricular tachycardia, fibrillation or ectopic beats. A variable PR interval can indicate a wandering atrial pacemaker, Wenckebach rhythm (2nd degree Mobitz Type I), 3rd degree (complete ) AV block. Additional Assessments: The T wave & the QT interval The T wave represents ventricular repolarization. It usually deflects upright in all leads except aVR and V1. Assess the T wave for abnormalities in shape or consistency and for inversion in leads where it normally is upright. T wave abnormalities may be seen with myocardial ischemia or infarction, bundle branch blocks, pulmonary embolism, electrolyte imbalances and ventricular hypertrophy, among other conditions. The QT interval represents the total time for ventricular depolarization and repolarization. Abnormalities in the QT interval can indicate risk for serious ventricular arrhythmias. Prolonged QT intervals can also be caused by medication effects, hypocalcemia, myocarditis and CNS lesions. ECG Monitoring Arrhythmia Review Sinus Rhythms Normal Sinus Rhythm Rate: 60-100 beats per minute (BPM) Rhythm: Regular P waves: upright, normal shape, consistent, one before each QRS complex PR interval: 0.12 – 0.20 seconds (normal) QRS: 0.10 seconds or less Sinus Bradycardia Rate less than 60 BPM Can result in decreased cardiac output Show strips from module Causes : medication effects (calcium channel blockers, digoxin, beta blockers), increased vagal tone sinus node disease, hypothyroidism, hypothermia, ischemia, increased intracranial pressure Treatments: atropine (drug of choice), epinephrine or dopamine, transcutaneous of tranvenous pacing Sinus Tachycardia Rate usually 100-160 bpm Causes: increased activity, fever, anxiety/fear, pain, infection, hypoxia, acute MI, hypovolemia, medication effects (epinephrine, atropine), stimulants (caffeine, nicotine, or cocaine), CHF Treatment: Treat the underlying cause. Sinus Arrhythmia Rate usually 60-100 bpm but may be faster or slower Rhythm is irregular (shortened R-R intervals during inspiration, lengthened during expiration) There is not usually any treatment required for sinus arrhythmia.. If significant sinus bradydysrhythmia occurs and patient is symptomatic, treat for sinus bradycardia. ECG Monitoring Arrhythmia Review Sinus Rhythms (continued) Sinoatrial Block Rate is usually normal but will decrease with pauses Rhythm is irregular Causes: SA node disease, acute MI, medication effects (digoxin, quinidine, procainamide), CAD, myocarditis, CHF, increased vagal tone or stimulation. Treatment: treatment is the same for symptomatic bradycardia, if present. Sinus Pause/ Arrest Rate is usually normal but will decrease with pauses Rhythm is irregular Causes: SA node disease, acute MI, medication effects (digoxin, quinidine, procainamide), myocarditis, hyperkalemia, increased vagal tone or stimulation. Treatment: treatment is the same for symptomatic bradycardia, if present. Atrial Rhythms Premature Atrial Contractions (PACs) Rate is variable, depending on underlying rhythm Rhythm will be irregular at point of PACs Premature P waves will be different than sinus P waves , but vary depending on site Causes : hypokalemia, hypomagnesemia, anxiety, stimulants (caffeine, tobacco or alcohol),digitalis toxicity, and myocardial ischemia or injury. Treatment: not usually required if PACs are infrequent; treat underlying cause Ectopic Atrial Rhythms Rate is less than 100 bpm Regular rhythm P waves are different than sinus P waves , but will depending on site; may be inverted Causes : same as PACs. Treatment: not usually required. ECG Monitoring Arrhythmia Review Atrial Rhythms (continued) Wandering Atrial Pacemaker Rate is less than 100 bpm Irregular rhythm At least three different morphologies of P waves (all vary from sinus P waves) Causes: digitalis toxicity, acute rheumatic fever, asthma, COPD, SA node disease, atrial hypertrophy and acute MI. Treatment: does not usually require treatment. Multifocal atrial tachycardia Rate is greater than 100 bpm Irregular rhythm At least three different morphologies of P waves (all vary from sinus P waves) Causes: COPD, CHF, and hypoxia. Treatment: treat the underlying disorder. Atrial Flutter Atrial rate is 250-350 bpm; ventricular rate is variable. Saw-toothed flutter waves (no regular P waves) Causes: stimulants (alcohol, nicotine, etc.), stress, fatigue, electrolyte imbalances, acute MI, ischemic heart disease, valvular disease, pulmonary embolism, digitalis or quinidine toxicity. It can also occur following open-heart surgery. Treatment: may include: cardioversion, calcium-channel blockers, beta-blockers, digoxin, warfarin (to prevent emboli) Atrial Fibrillation Atrial rate is usually >350-400 bpm; ventricular rate is variable Fibrillatory waves (no regular P waves) Causes: stimulants (alcohol, nicotine, etc.), stress, fatigue, electrolyte imbalances, acute MI, openheart surgery, ischemic heart disease, valvular disease, and hypertension. Treatments : cardioversion, calcium-channel blockers, beta-blockers, digoxin, warfarin (to prevent emboli) Atrioventricular Nodal Reentrant Tachycardia (AVNRT) Rate is 150-250 bpm P waves may be hidden in QRS or may appear a pseudo S or R wave In AVNRT, reentry is due to the presence of both a fast and slow pathway within the AV node that can allow the electrical impulse to reverse direction and generate another heartbeat. Treatments: Vagal maneuvers are the initial treatment for stable AVNRT. If vagal maneuvers are unsuccessful, adenosine may be administered. ECG Monitoring Arrhythmia Review Junctional Arrhythmias Premature Junctional Complexes Rate depends on underlying rhythm Regular rhythm with premature beats P waves may be before, after or hidden in QRS; if visible, inverted in leads II, III and aVF. Causes: stimulants (caffeine, tobacco, alcohol), electrolyte imbalance, heart disease, ischemia or MI, hypoxia, digitalis toxicity and sinus node dysfunction. Treatments: no treatment is usually necessary; treat the underlying cause. Junctional Escape Beats & Rhythms Junctional escape rhythm is comprised of three or more junctional escape beats in a row. Rate is 40-60 bpm P waves may be before, after or hidden in QRS; if visible, inverted in leads II, III and aVF. Causes: heart disease, acute MI, hypoxia, sinus node dysfunction, cardiac surgery and with certain medications (digitalis toxicity, beta-blockers, calcium-channel blockers). Treatment: if infrequent, treatment may not be necessary. If patient is symptomatic, may include atropine, pacing, or digibind (if related to digitalis toxicity). Accelerated Junctional Rhythms & Junctional Tachycardia Rate is 60-100 for accelerated junctional rhythm; 100-150 for junctional tachycardia P waves may be before, after or hidden in QRS; if visible, inverted in leads II, III and aVF. Causes: electrolyte imbalances, digitalis toxicity, ischemia, MI and myocarditis. Treatment: depends on severity of symptoms; may include vagal maneuvers, adenosine, digibind (if related to digitalis toxicity), antiarrhythmics, pacing or ablation therapy. ECG Monitoring Arrhythmia Review Ventricular Rhythms Premature Ventricular Complexes (PVCs) *Frequent PVCs (more than 6 per minute) can be life threatening. Rate depends on underlying rhythm Regular rhythm with premature beats No P waves with PVC Wide, abnormal QRS ; T wave is usually in opposite direction of QRS complex. Causes: stimulants (caffeine, nicotine, alcohol), stress, and fatigue, ischemia, MI, CHF, electrolyte imbalance, acid-base imbalance, digitalis toxicity, and medication effects (sympathomimetics, beta-agonists, tricyclic antidepressants). Treatments: based on the cause and the patient’s symptoms. Idioventricular rhythms (IVR) Idioventricular rhythms are composed of 3 or more continuous ventricular escape beats. Ventricular rate is 20-40 bpm (atrial rate not discernible) No P waves Wide, abnormal QRS ; T wave is usually in opposite direction of QRS complex. Causes: electrolyte imbalances, digitalis toxicity, myocardial ischemia or injury, and cardiomyopathy. Treatment: increase heart rate, may require transcutaneous pacing, atropine Accelerated Idioventricular Rhythm (AIVR) Ventricular rate is 40-100 bpm (atrial rate not discernible) No p waves Wide, abnormal QRS complex; T wave is usually in opposite direction of QRS complex. Causes: digitalis toxicity, MI, myocardial ischemia or injury, and cardiomyopathy. Treatment: if unstable, cardioversion or pacing may be needed. ECG Monitoring Arrhythmia Review Ventricular Rhythms (continued) Ventricular Tachycardia *Life threatening arrhythmia Ventricular rate 100-250 bpm (atrial rate not discernible) P waves may or may not be present; not associated with QRS complex Wide, abnormal QRS complex Causes : electrolyte imbalance, acid-base imbalance, myocardial ischemia or infarction, drug toxicity (digitalis, other antiarrhythmics), cardiomyopathy, infection (myocarditis, Chagas disease), CNS stimulants (cocaine, amphetamines) Treatment: If the patient is symptomatic and has palpable pulses, cardioversion is the treatment of choice. If the patient does not have palpable pulses, immediate defibrillation is required. Torsades de pointes *Life threatening arrhythmia Ventricular rate 150-250 bpm (atrial rate not discernible) No P waves Wide, abnormal QRS complex Changes in QRS shape, amplitude (height) and width Causes: conditions associated with prolonged QT interval , including medications (quinidine and procainamide, among others) and electrolyte imbalances (hypokalemia, hypomagnesia, hypocalcemia). Treatment : address the cause of the prolonged QT interval. Unstable patients should be treated with defibrillation. Ventricular fibrillation *Life threatening arrhythmia No discernible rate Chaotic, rapid, irregular rhythm No discernible P waves or QRS complexes Causes: myocardial ischemia or infarction, electrolyte imbalance, cardiomyopathy, hypoxia, congenital conditions, electrocution, untreated ventricular tachycardia, R-on-T PVCs. Treatment: Unless advanced life support is started immediately, ventricular fibrillation is a fatal rhythm. VF requires defibrillation as soon as possible. Vasopressors (epinephrine, vasopressin) and antiarrhythmics (amiodarone) may also be used – follow current ACLS protocol. ECG Monitoring Arrhythmia Review Atrioventricular Blocks First Degree Atrioventricular (AV) Block PR interval >0.20 seconds Causes: acute MI,medication effects (digitalis, calcium channel blockers, beta-blockers, among others), electrolyte imbalances, myocarditis, AV node disease Treatments: usually no treatment needed for first-degree AV block. Second Degree Atrioventricular (AV) Block, Mobitz Type 1 PR interval lengthens after each P wave until QRS is eventually dropped, then cycle starts again Causes: acute MI,medication effects (digitalis, calcium channel blockers, beta-blockers, among others), electrolyte imbalances, myocarditis, AV node disease Treatments: usually no treatment needed. Second-Degree Atrioventricular (AV) block, Mobitz Type II Impulses intermittently blocked resulting in dropped QRS complexes P waves occur at consistent intervals Causes: anteroseptal MI, structural heart disease ,cardiac surgery, medication effects , infiltrative conditions , inflammatory conditions , autoimmune conditions , hyperkalemia Treatment: temporary pacing until a permanent pacemaker can be placed. Mobitz type II is a more serious condition than type I and can rapidly progress to third-degree heart block. Third-degree Atrioventricular (AV) block Atrial impulse are not conducted to the ventricles. Secondary pacemaker in the AV node or below pace s the ventricles. No correlation between P waves and QRS complexes. QRS will be narrow if secondary pacemaker is junctional, wide if it is ventricular. Causes: same as second-degree AV block Treatment: most patients will require placement of a permanent pacemaker. ECG Monitoring Arrhythmia Review Pulseless Electrical Activity Pacemakers Pulseless electrical activity (PEA) is not a specific arrhythmia, but occurs when an organized rhythm is seen on the ECG tracing but ventricular contraction does not occur and, therefore, the patient is pulseless. Pacemakers can pace either the atria or the ventricles (single chamber pacemakers) or both (dual chamber pacemakers). Show strip from module • Pulseless electrical activity can present as various rhythms on the ECG tracing, including sinus rhythm, bradycardias and tachycardia. • • In atrial pacing, a spike will be seen prior to the P wave. In ventricular pacing, a spike will be seen before the QRS complex. Spikes before the P wave and QRS complex will be present when the patient has a dual chamber pacemaker. Show pacemaker strips from module Pacemaker Problems Notable on the ECG Failure to pace Absence of pacemaker spikes when the patient’s heart rate is below the pacemaker rate. Failure to capture Pacemaker spikes will be seen on the ECG but they will not be followed by a P wave (in atrial pacing) or a QRS complex (in ventricular pacing). Failure to sense The pacemaker spike will be seen in an inappropriate place on the ECG (for example, after or near a QRS complex in ventricular pacing).