Cardiac Arrythmias
advertisement
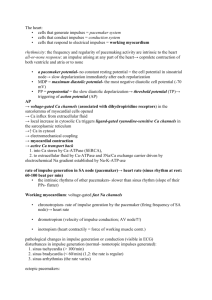
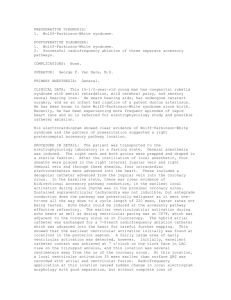
Cardiac Arrhythmias: An Update Dr N.M.Gandhi Consultant Cardiologist Spire Gatwick Park Hospital, Horley East Surrey Hospital, Redhill Royal Sussex County Hospital, Brighton Objectives • Identify common arrhythmias encountered by the family physician • Discuss initial Mg options • AF and Ventricular arrhythmias case studies • Which patients needs to be referred? ECG examples THE CONDUCTION SYSTEM Atrial Depolarization Ventricular Depolarization CARDIAC ARRHYTHMIAS Disturbances of either : • Impulse generation • Impulse propagation A R R H Y T H M I A S ELECTROPHYSIOLOGIC PRINCIPLES BRADYARRHYTHMIAS • SINUS NODE DYSFUNCTION • AV CONDUCTION DISTURBANCES TACHYARRHYTMIAS •ATRIAL TACHYCARDIAS •VENTRICULAR TACHYCARDIA Bradyarrhythmias • Impulse formation: – Decreased automaticity: Sinus bradycardia • Impulse conduction: – Conduction blocks: 1º, 2º, 3º AV blocks Tachyarrythmias • Impulse formation – Enhanced automaticity: • Sinus node: sinus tachycardia • Ectopic focus: Ectopic atrial tachycardia – Triggered activity • Early afterdepolarization: torsades de pointes • Digitalis-induced SVT • Impulse conduction – Reentry: Paroxysmal SVT, atrial flutter and fibrilation, ventricular tachycardia and fibrillation. Normal Sinus Rhythm www.uptodate.com Implies normal sequence of conduction, originating in the sinus node and proceeding to the ventricles via the AV node and His-Purkinje system. EKG Characteristics: Regular narrow-complex rhythm Rate 60-100 bpm Each QRS complex is proceeded by a P wave P wave is upright in lead II & downgoing in lead aVR PAC • Benign, common cause of perceived irregular rhythm • Can cause sxs: “skipping” beats, palpitations • No treatment, reassurance • With sxs, may advise to stop smoking, decrease caffeine and ETOH • Can use beta-blockers to reduce frequency PVC • Extremely common throughout the population, both with • and without heart disease Usually asymptomatic, except rarely dizziness or fatigue in patients that have frequent PVCs and significant LV dysfunction PVC • Reassurance • Optimize cardiac and pulmonary disease management • Beta-blocker • Ablation in a small number of cases Bradyarrhythmias • Impulse formation: – Decreased automaticity: Sinus bradycardia • Impulse conduction: – Conduction blocks: 1º, 2º, 3º AV blocks Sinus Bradycardia • HR< 60 bpm; every QRS narrow, preceded by p wave • Can be normal in well-conditioned athletes • HR can be 30 bpm in adults during sleep, with up to 2 sec pauses Sinus arrhythmia • Usually respiratory--Increase in heart rate during • • • • inspiration Exaggerated in children, young adults and athletes—decreases with age Usually asymptomatic, no treatment or referral Can be non-respiratory, often in normal or diseased heart, seen in digitalis toxicity Referral may be necessary if not clearly respiratory, history of heart disease Sick Sinus Syndrome •All result in bradycardia •Sinus bradycardia with a sinus pause •Often result of tachy-brady syndrome: where a burst of atrial tachycardia (such as afib) is then followed by a long, symptomatic sinus pause/arrest, with no breakthrough junctional rhythm. 1st Degree AV Block • PR interval >200ms • If accompanied by wide QRS, refer to cardiology, high risk of progression to 2nd and 3rd deg block • Otherwise, benign if asymptomatic 2nd Degree AV Block Mobitz type I (Wenckebach) • Progressive PR longation, with eventual non• conduction of a p wave May be in 2:1 or 3:1 2nd degree block Type II (Mobitz 2) • Normal PR intervals with sudden failure of a p wave to • • • conduct Usually below AV node and accompanied by BBB or fascicular block Often causes pre/syncope; exercise worsens sxs Generally need pacing, possibly urgently if symptomatic 3rd Degree AV Block • • • • Complete AV disassociation, HR is a ventricular rate Will often cause dizziness, syncope, angina, heart failure Can degenerate to Vtach and Vfib Will need pacing, urgent referral Tachyarrythmias • Impulse formation – Enhanced automaticity: • Sinus node: sinus tachycardia • Ectopic focus: Ectopic atrial tachycardia – Triggered activity • Early afterdepolarization: torsades de pointes • Digitalis-induced SVT • Impulse conduction – Reentry: Paroxysmal SVT, atrial flutter and fibrilation, ventricular tachycardia and fibrillation. SUPRAVENTRICULAR T. • Sinus Tachycardia • Atrial flutter • Atrial fibrilation • Paroxysmal Supraventricular • Multifocal Atrial T. • Preexcitation Syndrome (Wolff-Parkinson-white Sy.) Sinus tachycardia • HR > 100 bpm, regular • Often difficult to distinguish p and t waves Paroxysmal Supraventricular T. • Sudden onset and termination • Atrial rates of 140 to 250 /min • Normal QRS complexes • The mechanism is most often reentry. Paroxysmal Supraventricular Tachycardia • Refers to supraventricular tachycardia other • than afib, aflutter and MAT Usually due to reentry—AVNRT or AVRT PSVT • CSM or adenosine commonly terminate the arrhythmia, esp, AVRT or AVNRT • Can also use CCB or beta blockers to terminate, if available • Counsel to avoid triggers, caffeine, Etoh, pseudoephedrine, stress Multifocal Atrial T. • Is due to enchanced automaticity within the atria, resulting in abnormal discharges from several ectopic foci • Most often occurs in the setting of severe pulmonary disease and hypoxemia. • EKG: irregular rhythm with multiple (at leats 3) P waves morphologies Atrial flutter • Is caracterized by rapid coarse “sawtooth” appearing atrial activity, at rate of 250 to 350 x min. – Many of these fast impulses reach the AV node during its refractory period, so that the ventricular rate is generally lower. • Frequently it degenerates into atrial fibrilation – The most expiditious therapy is electrical cardioversion, which is undertaken directly for highly symptomatic patients. (to revert chronic refractory atrial flutter that has not responded to other approaches) Preexcitation Syndrome • Wolff-Parkinson-White Syndrome • EKG: Although different types of bypass tracts have been identified, the bundle of Kent, is the most common and can usually conduct in both the anterograde and retrograde directions. Atrial Fibrillation • • • • Irregular rhythm Absence of definite p waves Narrow QRS Can be accompanied by rapid ventricular response Atrial fibrillation--management • Rhythm vs Rate control—if onset is within last • • 24-48 hours, may be able to arrange cardioversion—use heparin around procedure Need TEE if valvular disease (high risk of thrombus) If unable to definitely conclude onset in last 2448 hours: need 4-6 weeks of anticoagulation prior to cardioversion, and warfarin for 4-12 weeks after Atrial Fibrillation: Clinical Problems • Embolism and stroke (presumably due to LA clot) • Acute hospitalization with onset of symptoms • Anticoagulation, especially in older patients (> 75 yr.) • Congestive heart failure – Loss of AV synchrony – Loss of atrial “kick” – Rate-related cardiomyopathy due to rapid ventricular response • Rate-related atrial myopathy and dilatation • Chronic symptoms and reduced sense of well-being AF: Medical Management • Treatment of underlying cause • Ventricular rate control • Anticoagulation • Antiarrhythmics with a view to restore sinus rhythm Control of Ventricular Rate in Atrial Fibrillation • Betablockers • Calcium channel blockers Verapamil, diltiazem • Digoxin • Amiodarone Anticoagulation Anticoagulation • Assessment of bleeding risk should be part of the clinical assessment of AF patients prior to starting anticoagulation • Antithrombotic benefits and potential bleeding risks of long-term coagulation should be explained and discussed with the patient • Aim for a target INR of between 2.0 and 3.0 NICE 2006 CHADS 2 scoring CCF Hypertension Age > 75 Diabetes Stroke/TIA 1 point 1 point 1point 1 point 2 points • Any patients with AF with a score of =/>2 would benefit from being on Warfarin Cardioversion Cardioversion • Cardioversion results in SR in at least 90% of cases • SR is only maintained in 30-50% at one year • Class 1a, 1c and III agents increase likelihood of maintained SR from 30-50% to 50-70% at one year Follow-up • Follow-up after cardioversion should take place at 1 month, and the frequency of subsequent reviews should be tailored to the patient • Reassess the need for anticoagulation at each review Catheter Ablation for AF AF Ablation • Success rates – approx 70% but may require repeat procedure – Often increase in symptoms for first 3-6 months after procedure does not indicate failure • Risks – – – – – damage to existing conduction mandating pacing Cardiac perforation/tamponade Bleeding Stroke/thromboembolism Death Catheter Ablation: Indications • Symptomatic patients • Refractory to Antiarrhythmics • Medical therapy contraindicated due to comorbidities or intolerance NICE 2006 Which AF patients need Specialist Referral? • Patients with: - WPW syndrome Uncontrolled ventricular rate (> 200/min) Tachy-brady syndrome For rhythm control strategy CCF Intolerant to Drugs Invasive options VENTRICULAR ARRHYTHMIAS • Ventricular tachycardia • Torsades De Pointes • Ventricular fibrillation Ventricular tachycardia • Is divided in 2 categories: – If it persist for more than 30 seconds “sustained VT” – Less than 30 seconds: “nonsustained VT” • Symptoms vary depending on the duration. – Major manifestations are hypotension and loss of consciousness. Non-sustained ventricular tachycardia • Need to exclude heart disease with Echo and • • • • stress testing May need anti-arrhythmia treatment if sxs In presence of heart disease, increased risk of sudden death Need referral for EPS and/or prolonged Holter monitoring ICD may be life saving Torsades De Pointes • Varying amplitudes of the QRS. • It can be produced by afterdepolarizations (triggered activity). • Particularly in prolonged QT interval. • Occur with some drugs (quinidine), electrolite disturbances, and congenital prolongation of the QT interval. Specialist Referral ECG Examples Contact... * E-mail: nandkumar.gandhi@sash.nhs.uk drnmgandhi@hotmail.com * Fax: 01737 231938 * Phone: Spire - 01293 785511 ESH - 01737 768511, ext.6333