WHEN IS A MOLE NOT A MOLE?
advertisement
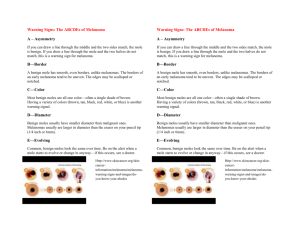
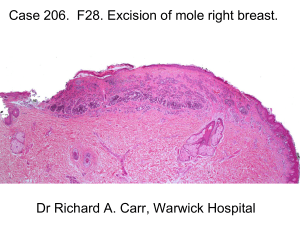
DR. OLGA WATKINS 31st July 2012 Outline Of Presentation Common Skin Lesions, Benign And Malignant Assessment Of Pigmented Lesion Points to take home Skin lesions, tumours and cancers Actinic keratosis Angiokeratoma Angiolymphoid hyperplasia Angiosarcoma Aplasia cutis Atypical fibroxanthoma Atypical naevi Basal cell carcinoma Bazex syndrome Which is Malignant? SSMM BCP Which is Benign? Amelanotic melanoma Blue naevus Which Would Worry You? Irritated BCP Pyogenic granuloma Benign Viral warts Seborrhoeic keratoses Naevi Angiomas Epidermoid cysts Other common lesions Viral warts Viral warts on fingers Seborrhoeic Keratoses Seborrhoeic Keratoses Benign naevi Atypical naevus Blue Naevus Melanocytes deep within the skin Benign but usually excised to exclude melanoma Halo Naevus Benign lesion Auto-immune reaction, with depigmentation of skin surrounding naevus. Skin eventually repigments. Remember Melanoma is rare in children under 12 years age Adults can develop benign naevi up to 50 years of age Regression surrounding melanoma Cherry Angioma Angiokeratoma Angiokeratoma of Fordyce Epidermoid (Sebaceous) Cyst Dermatofibroma Feels hard, dimples when edges pressed together Scarring due to insect bites Pinch sign Senile Comedone Keratoacanthoma Pre-malignant Actinic keratoses Bowens disease Lentigo maligna / melanoma in situ Actinic Keratosis Found on sun-exposed sites Patient with ≥ 10 lesions has 10% risk of developing SCC in one Treated with cryotherapy, 5-FU , Photodynamic Therapy (PDT) AKs on scalp Bowens disease on leg Bowens Disease Pre-cancerous 5% risk of developing SCC if not treated Lentigo Maligna Melanoma in situ LM/Melanoma-in-situ LM arises on sun-damaged skin, face and neck Melanoma-in-situ in other areas 5% develop melanoma so need to be treated Can monitor in secondary care in older people if treatment difficult Malignant Basal cell carcinoma Squamous cell carcinoma Melanoma Metastatic disease Superficial Basal Cell Carcinoma Treatment options include cryotherapy, 5- FU and PDT Nodular BCC Pigmented BCC Squamous Cell Carcinoma Squamous Cell Carcinoma Which is Which? Keratoacanthoma SCC Superficial Spreading Malignant Melanoma Nodular Melanoma Amelanotic Melanoma Similar to pyogenic granuloma but the history is different MAJOR SURGERY LONGANDWINDING ROAD GLASGOW G46 6HT Dermatology Clinic Stirling Royal Infirmary FK8 2QR Dear Doctor, DERMOT TITUS 12/04/1945 This patient has a pigmented lesion on his back that he has had for some time. It is increasing in size. It has an irregular border and is very itchy. Please can you see him urgently to exclude a melanoma? Sincerely, Dr. Doolittle Dr. Doolittle MB ChB Assessment of Naevi SEVEN POINT CHECKLIST Change in shape Change in size Change in colour Over 6 mm. in diameter Inflammation Crusting or bleeding Minor itch or irritation Assessment of Naevi ABCD(E) METHOD A - asymmetry B - borders irregular C - colour variation D - diameter larger than pinkie nail (E – rapid elevation) A – asymmetry B - borders irregular C - colour variation D - diameter larger than pinkie nail (E – rapid elevation) POINTS TO TAKE HOME Always take a full history Learn to recognise the difference between seborrhoeic keratoses and naevi The most important history in melanoma is one of rapid change in a pre-existing naevus or of a new naevus Internet Support www. pcds.org.uk www.dermnetnz.org www.gpnotebook.co.uk www.bad.org.uk www. pathways.scot.nhs.uk ( being rewritten at present)