Case Study 26
advertisement
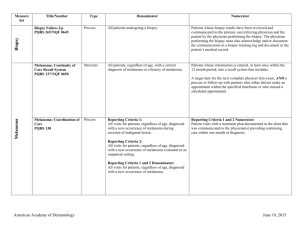
Case Study 26 Craig Horbinski, M.D., Ph.D. Question 1 The patient is a 79-year-old female with expressive aphasia for the past three to four days. Past medical history included hypertension, glaucoma, status post CABG and status post cholecystectomy. MRI was done. Describe the scans. Answer MRI: Enhancing mass in the left frontal lobe with central necrosis, midline shift, and extensive surrounding edema. Question 2 What is your differential at this time? Answer 1. High grade glioma 2. Metastatic disease 3. Lymphoma 4. Bacterial abscess Question 3 During surgery, the neurosurgeon asks you to look at some tissue he’s taken from the site. You do a couple of touch preparations on some grossly abnormal tissue. What do you tell him? Click here to view slide. Answer This is neoplastic. There is hypercellularity with clumpy chromatin, some vacuoles in the relatively abundant cytoplasm, and necrosis (the granular, grimy stuff). The tumor cells are broad, epithelioid, and seem to mostly stick together, although some are isolated. A few lymphocytes and foamy macrophages are scattered around. An adenocarcinoma is a possibility since the cells have an epithelioid appearance and show some vacuoles. Question 4 The permanent section arrives the next day. Describe what you see. Click here to view slide. Answer Sections show an epithelioid tumor consisting of large round cells with well-demarcated cell borders. Some cells have prominent nucleoli, and most have clumpy chromatin. A minor fasciculating spindle cell population is also present. There is patchy necrosis, scattered mitoses, thrombosed vessels, and endothelial proliferation. The tumor has a pushing border with adjacent brain which is gliotic and has a modest inflammatory reaction. Question 5 What is your differential now? Any immunostains you’d like to order to prove your suspicion (Hint: the answer is YES). Answer This is definitely a high-grade neoplasm that looks epithelioid and is highly necrotic. The differential here is glioma versus metastatic carcinoma (unknown primary) versus metastatic melanoma (primary site is often missed clinically). Immunostains to resolve this include: 1.GFAP—positive in gliomas, negative in carcinoma and melanoma 2.Cytokeratins 7/20 or CAM5.2*—positive in carcinomas, negative in gliomas and melanomas 3.S100—positive in gliomas and melanoma, negative in carcinoma 4.HMB45—positive in melanoma, negative in glioma and carcinoma 5.Vimentin—positive in all three, just a control to make sure the tissue is of decent quality for immunostaining *Of note, pankeratin is a bad choice for a carcinoma marker, because the antibody mixture cross-reacts with glial filament proteins and makes gliomas seem positive. Cytokeratin AE1/3 used to be a good antibody to avoid this problem, but recently for some reason it too has false-positive staining in gliomas. Question 6 Some immunostains arrive. S100 is shown. HMB45 and cytokeratins are negative (not shown). GFAP stain failed; the immunohistochemistry lab will send another stain tomorrow. How do you interpret these findings? What is your diagnosis? Are you ready to sign out the case? Click here to view slide. Answer If you’re thinking melanoma, reasoning that HMB45 can sometimes be negative in melanomas, think again. S100 is positive in glial cells, too. Best to wait for the GFAP stain to come out. Question 7 The GFAP stain finally arrives. What is your diagnosis NOW? Click here to view slide. Answer Glioblastoma. This is a classic case of a glioblastoma mimicking an epithelioid neoplasm, either a carcinoma or melanoma. Cases like this are why the original name for this glial tumor was “glioblastoma multiforme,” and why it’s best to wait for all the immunostains to arrive before signing the case out. If you were thinking it was some sort of metastatic carcinoma during the intraoperative phase of the case, don’t feel too bad—the neuropath attending on the case made that same diagnostic mistake. Just goes to show you’re never too good to be fooled…