Skin
advertisement
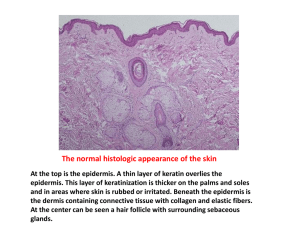
SKIN Benign skin lesions Sebaceous cyst Aka epidermal inclusion cysts. Produced by obstruction of mouth of a sebaceous gland, contain epidermal debris. Might see punctum. Can become infected./ulcerated/calcified/form a horn. They are smooth, soft/firm, and attached to the skin. Dermoid cyst Deep to skin, not attached to it. Congenital. Found at junction of lines of fusion of facial skin. Often in midline. Keratoacanthoma ? Arise from hair follicles. DDx SCC. Rapidly growing lump, like 2cm in 6 weeks. Centre ulcerates and the lesion begins to regress, eventually heals in 2-3months. Not painful. Excise for cosmetic reasons and to confirm that not an SCC. Keratoses Keratoses are lesions caused by hypertrophy of the epidermis. They are very common. Solar keratoses may undergo malignant change. Two types: - Solar keratoses – premalignant, sun-exposed skin - Seborrheic keratitis – v common, unknown aetiology, body of elderly men, multiple raised often pigmented lesions. Bowen’s disease This is an SCC in situ. Premalignant. Rare. If penis – erythroplasia de Querat. Malignant skin lesions Aetiological factors: - Sunlight – UVB, UVA - Immunosuppression – on immunosuppressants, AIDS - Radiation exposure - Chemical carcinogens - Inherited disorders – albinism, xeroderma pigmentosum - Chronic irritation – scars, with chronic ulcer (Marjolin’s ulcer) BCC Most common skin cancer. Aka rodent ulcer – invades locally if untreated, but does not metastasise. Malignant tumour arising from basal cells of the epidermis. Elderly, especially mean. Sun exposed skin, especially face, especially superior to line joining angle of mouth and tragus. Crator at centre, can ulcerate. Pearly rolled edges. Tx: wide local excision. CO2 laser if cant excise completely (near eye?). SCC Arises from keratinocytes of epidermis. Solar keratoses and Bowen’s disease are precursors. Elderly. Sun exposed skin. Flat red mobile lesions initially, then become fixed to skin and underlying tissues. Ulcerated necrotic centre. Heaped edges. Can get in areas of chronic irritation – Marjolin’s ulcer. Aggressive tumour, will invade structures deep to dermis with metastasis to regional lymph nodes. Tx: wide local excision. Generally follow for 5 years after treatment. Kaposi’s sarcoma A multicentric angiosarcoma, get purple-brown tumour nodules varying from 1mm-1cm in diameter. Most commonly on hands and feet. An AIDS-defining illness. Naevi Benign, pigmented lesions that arise from increased number of melanocytes. Different types, depending on site of melanocye accumulation: - Lentigo – hands and face of elderly - Junctional – arise at or after puberty. Smooth, flat, often irregularly pigmented. - Dermal – entirely within dermis. Elevated.Usually in adults. - Compound – like junctional + dermal. May develop into melanomas. - Blue – melanocytes deep within dermis. Malignant melanoma Incidence increasing faster than any other human cancer. About 1% of all children born today will develop it? Incidence 10 per 100,000. 50% arise in pre-existing naevi. Age – 50s. Exposure to intense UV radiation is biggest risk factor. Fair-skinned people. Other RFs are giant congenital naevi, FHx, severe sunburn before age 18, freckly, white race, blonde/red hair, ?actinic keratoses. In females mostly on legs, in males on back. Types: 1. Superficial spreading (80% of cases) – slow growing, mets late, flat 2. Nodular – most aggressive, black/blue colour 3. Lentigo maligna – older people 4. Acral lentiginous melanoma – on palms/soles, dark-skinned people, mets early. Diagnosis… A – Asymmetry in 2 axis B – Borders – irregular C – Colour – variation D – Diameter – (>6mm) E – Elevation If any of these are present, refer. Major criteria – size, colour shape Minor criteria – oozing, inflammation, diam (>7mm), itching, decreased sensation Refer if 1 major or 2/3 minor. Staging of melanoma (Clark’s levels) I Melanoma confined to the epidermis II Melanoma infiltrates the papillary dermis without filling it III Plugs papillary dermis and compresses the reticular dermis without Infiltrating it IV Infiltrates the reticular dermis V Infiltrates the subcutaneous fat tissue Staging of melanoma (Breslow depth) 0 – 0.75mm 0.76 – 1.5mm 1.51 – 4.0mm >4.0mm <1mm depth – very rarely have mets to nodes. >2mm – about 25% chance of nodal mets >4mm – about 50% chance of nodal mets When your excision biopsy comes back positive for melanoma, excise your scar again and try achieve primary closure. If <1mm – no further treatment. If up to 2mm, want 10mm margin. If greater than 2mm – want 20mm margin. If <1mm and no palpable nodes – treatment complete If >1mm and no palpable nodes – do sentinel lymph node biopsy. If node neg – treatment complete. If node pos - lymphadenectomy If >2mm – have to search for nodal mets (bloods, CXR, SLNM, CT brain/thorax/abdo/pelvis or liver US) Only consider chemo for node positive patients, if no distant mets. Use dacarbazine, IFN. High dose, lots of toxicity. Trials going looking at BCG, vaccines, Interleukin 2 and tauroludine. MDT important. Review by original surgeon usually.