SKIN TUMOURS
advertisement

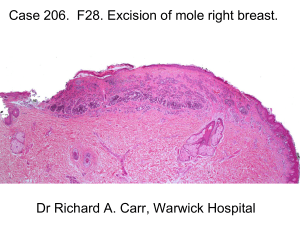
SKIN TUMOURS DR IMRANA ZULFIKAR ASSITANT PROFESSOR SURGERY CLASSIFICATION OF SKIN TUMOURS BENIGN TUMOURS MALIGNANT TUMOURS BENIGN TUMOURS • • • • • • • BASAL CELL PAPILLOMAS PAPILLARY WART FRECKLE LENTIGO NAEVI/MOLES HALO NAVUS CAFÉ AU LAIT SPOTS BASAL CELL PAPILLOMA SOFT WARTY LESIONS,PIGMENTED AND HYPERKERATOTIC IN BASAL LAYER PAPILLARY WART BENIGN SKIN TUMOURS HPV FRECKLE NORMAL NUMBER OF MELANOCYTES WITH INCREASE PRODUCTION LENTIGO • SHARPLY CIRCOMSCRIBED PIGMENTED MACULES • MAY AT TIMES ASSOCIATED WITH PEUTZ JEGHERS SYNDROME MOLES/NAEVUS • MOLES/NAEVUS ARE LAYERED OR AGGREGATES OF MELONICYTES IN EPIDERMIS BASAL CELL PAPILLOMAS PAPILLARY WART FRECKLE LENTIGO NAEVIMOLES HALO NAVUS CAFÉ AU LAIT SPOTS PREMALIGNANT LESIONS • • • • • • • ACTINIC KERTOSES CUTANEOUS HORN KERATOACANTHAOMA BOWENS DISEASE EXTRA MAMMARY PAGETS DISEASE GIANT HAIRY NAEVUS DYSPLASTIC NAEVUS ACTINIC KERATOSES • DYSKERATOSIS WITH CELLULAR ATYPIA • 20% SCC CUTANEOUS HORN • CUTANEOUS ACCUMULATION (HEIGHT GREATER THAN BASE) • 10% SCC • KERATOACANTHOMA • CUP SHAPED GROWTH PLUG OF KERATIN • M>F,50-70 YR ,ON FACE. • PAPPILLOMA VIRUS,SMOKING ,CHEMICAL CARCINOGENIC • SURGICAL EXCISION ACTINIC KERATOSES CUTANEOUS HORN KERATOACANTHOMA BOWENS DISEASE • • • • • • SCC IN SITU CHRONIC SOLAR DAMAGE,ARSENIC EXPOSURE ,HPV 16 SLOW ENLARGINGERYTHMATOUS PATCH OR PLAGUE TOPICAL THERAPY 5 –FLUOROURACIL SURGICAL EXCISION 4MM MOHS MICROSCOPIC SURGERY EXTRAMMARY PAGETS DISEASE • INTRA DERMAL ADENOCARCINOMA • GENITAL OR PERIANAL REGIONSOR AXILLA • SURGICAL EXCISION BOWENS DISEASE EXTRAMMARY PAGETS DISEASE GIANT CONGINATAL PIGMENTED NAEVUS GCPNSPRECURSORS FOR MM MORE LIKELY WITH AXIAL LESIONS RETROPERITONEAL OR INTRACRANIAL LESIONS MULTIDICSIPILANARY MANAGEMENT PERINATAL CURETTAGE,DERMAABRASION,LASER RESURFACING, SURGICAL EXCISION WITH SKIN GRAFTS DYSPLASTIC NAEVUS IRREGULAR PROLIFERATIONS ATYPICAL MELANOCYTES AT BASAL LAYER OF EPIDERMIS GIANT CONGINATAL PIGMENTED NAEVUS DYSPLASTIC NAEVUS MALIGNANT LESION • BASAL CELL CARCINOMA • SUAMOUS CELL CARCINOMA • MALIGNANT MELANOMA ACTINIC SOLAR KREATOSIS CUTANEOUS HORN KERATOACHANTHOM A BOWENS DISEASE 20% S CC 10”% SCC SCC 3-11% SCC EXTRA MAMMARY PAGETS 25% SCC GIANT CONGENITAL PIMEMENTD NAEVUS 3-5% MM BASAL CELL CARCINOMA EPIDEMIOLOGY • • • • • • SLOW GROWING LOCALLY INVASIVE MALIGNANT TUMOUR PLURIPOTENT EPITHELIAL CELLS UVR IS STRONGEST PREDISPOSING FACTOR OTHERS MAY BEARSENICAL COMPOUNDS,COAL TAR,AROMATIC HYDROCARBONS 90%LESION ON FACE ABOVE ALINE FROM THE LOBE OF THE EAR TO THE CORNER OF MOUTH WHITE SKIN 40-80 YRS M>F PATHOGENESIS • • • SLOW GROWING PROPOTIANTE TO DOSE OF CARCINOGEN RARLY METASTISE HARD TO CULTURE MACROSCOPIC APPEARANCE • • • NODULAR NODULOCYSTIC CYSTIC MICROSCOPIOC APPEAREANCE • OVOID CELLS IN NEST WITH SINGLE OUTER PALISADING LAYER BASAL CELL CARCINOMA Nodular BCC • Chronic lesion • Easy bleeding • Pearly border • Surface telangiectasias • Head and neck, trunk, PROGNOSIS HIGH RISK GROUPS • • • • • >2CM NEAR EAR NOSE OR EYE ILL DEFIND MARGINS RECURRENT TUMOURS IMMUNOCOMPROMISED MANAGEMENT SURGICAL EXCISION MOHS MICROSCOPIC SURGERY NON SURGICAL RADIOTHERAPY TOPICAL 5-FLUROURASIL SQUAMOUS CELL CARCINOMA EPIDEMIOLOGY MALIGNANT TUMOUR OF KERATINISING CELLS OF EPIDERMIS OR ITS APPENDAGES SECOND MOST COMMON TUMOUR WHITE SKIN ELDERLY MEN WITH CUMULATIVE SUN EXPOSURE ALSO ASSOCIATED CHRONIC INFLAMMATION(SINUS TRACTS , PREEXISTING SCARS ,OSTEOMYLETIS,BURNS,IMMUNOSUPPRESION,MARJOLINS )2% METASTASIS 20% RECURRENCE MACROSCOPIC • • • • EVERTED EDGES WITH INFLAMMED SKIN SMOOTH NODULAR,VERROCOUS PAPILLOMATOUS ULCERATING MICROSCOPIC • • IRREGULAR MASSES OF SQUAMOUS EPITHELIUM CELLULAR MORPHOLOGY,BRODERS GRADE ,DEPTH OF INVASIONPERINEURAL OR VASCULAR INVASION SQUAMOUS CELL CARCINOMA PROGNOSIS INVASION>6CM HISTOLOGICAL GRADE HIGHER THE BRODER GRADE SITE LIPS AND EARS HAVE HIGH LEVEL OF RECURRENCE AEITOLOGY IMMUNOSUPPRESION MANAGEMENT • DEFINTE TREATMENT SURGICAL LOUPE EXCISION(4MM CLEARANCE MARGIN IF <2 AND 1CM MARGIN >2CM LESIONS ) • IN TRANSIT METSTASIS • LYMPHATIC METSTASIS MALIGNANT MALENOMA • EPIDEMIOLOGY • MM IS CANCER MELNOCYTES • MM ACCOUNTS FOR 5% OF SKIN MALIGNANCY • INCREASES UVR EXPOSURE • 3%OF ALL MALIGNANCYS • 75% OF ALL DEATHS • 7%OCCULT METASTASIS RISK FACTORS: • • • • • • • XERODERMAPIGMENTOSUM PAST MEDICAL OR FAMILY HISTORY HIGH NUMBER OF NAEVI TENDENCY TO FRECKLE GCPN DYSPLASTIC NAEVUS IMMUNOCOMPROMISED MACROSCOPIC APPEANRANCE • • • • SUPERFICIAL SPREADING MELANOMA75% NODULAR MELANOMA 15% LENTIGO MALIGNA MELANOMA5-10% ACRAL LENTIGIOUS MELANOMA2-8% FEATURES IN NAEVI SUGGESTING MM • CHANGE IN SIZE ,SHAPE COLOUR ,ITCHING,SATELLITE LESIONS • BLOOD SUPPLY Clinical types- MM Superficial spreading melanoma Lentigo maligna melanoma Acral lentiginous melanoma Nodular melanoma MALIGNANT MELANOMA ABCD of Melanoma • Asymmetry • Border irregularity • Color variegation • Diameter >6mm BRESLOWS THICKNESS GRADE • AJC STAGING Prognostic features- MM • Good prognosis – Breslow < 1mm • Intermediate prognosis – Breslow 1-4mm • Bad prognosis – Breslow >4mm • Good prognosis – Breslow < 1mm • Intermediate prognosis – Breslow 1-4mm • Bad prognosis – Breslow >4mm MANAGEMENT • HISTORY /CLINICAL EXMINATION • SKIN BIOPSY • SENTINEL LYMPH NODE BIOPSY • LOCAL TREAMENT • REGIONAL LYMPH NODES • • • • PROGNOSIS TUMOUR THICKNESS LYMPH NODES DISTANT METSTASIS VASCULAR LESIONS • CONGENITAL: HEAMANGIOMAS VASCULAR MALFORMATIONS • ACCUIRED: SIDER NAEVI CAMPBELL DE MORGAN SPOTS PYOGENIC GRANULOMAS ANGISARCOMAS KAPOSIS SARCOMA