Clinical Case Conference

Clinical Case Conference
Shivan Mehta, MD
August 11, 2010
Case
43M h/o Mulitiple Myeloma, chronic kidney disease presents with 2 weeks of hematochezia.
HPI
Initially diagnosed with Multiple Myeloma 1 year prior to presentation. Disease course c/b acute renal failure requiring short course of dialysis.
Presented to outpatient GI with intermittent hematochezia x 2 weeks. Reports bright red blood up to
4 times a day on toilet paper and mixed with stool. No melena. Mild abdominal pain.
ROS significant for 25 lb weight loss, mild abd cramping and pain, no dizziness/lt headedness/chest pain/sob
PMH
PMH: Multiple Myeloma (IgA monoclonal gammopathy) c/b CKD presenting with renal failure requiring HD and plasmapheresis. Bone marrow biopsy/ fat pad neg for amyloid.
PSH: None
Allergies: NKDA
Meds: Velcade/Decadron/Cytoxan (1 course 3 months prior), Renagel 800mg tid, Nephrocap 1tab daily,
Acyclovir
SH: Works as office manager. Married with no children.
Social Etoh. Denies tobacco/illicits
FH: no malignancy or other GI issues
Physical Exam
VS- T 97.8, BP 102/63, HR 85, RR 16, 99% RA
Gen- NAD, Ox3, pleasant, comfortable
HEENT- anicteric, pale conjunctivae
CV- RRR, no m/r/g
Chest- CTA b/l
Abd- soft, ND, + BS, mild diffuse TTP
Ext- 1+ lower extremity edema
Rectal- no masses, brown stool with streaks of red blood
140| 106| 36
------------------< 82
4.5 | 25 | 3.4
8.1
5.8 >-----< 186
24
MCV 88, RDW 16.1
Labs
TP 7.4, Alb 3.0
Tbili 1.0, Alk 73
ALT 45, AST 38
PT 13.2, INR 1.1
PTT 26.4
LDH 90
Differential Diagnosis
What is your differential diagnosis for hematochezia in a patient with multiple myeloma?
Differential Diagnosis
Ischemic colitis
Infectious colitis
CMV, Salmonella, Shigella, Campylobacter, E. Coli, Entameoba
Diverticulosis
AVM
Upper GI bleed
Neoplasm
Adenocarcinoma, Lymphoma, Plasmacytoma
Colonic ulcers
Medications, Idiopathic
GI amyloid
Inflammatory bowel disease
Hemorrhoids
EGD
Normal esophagus
Mild antritis-> pathology shows mild lymphocytic infiltrate, otherwise normal.
Normal duodenum
Colonoscopy
A large 5cm mass lesion with ulceration was seen in the cecum.
Small fragment of colonic mucosa within normal limits.
Fragment of fibrinopurulent exudate consistent with nearby ulcer.
Additional areas of ulceration were seen in the left colon.
Colonic mucosal biopsies with areas of acute inflammation and ulceration, granulation tissue formation and reactive atypia.
Underlying homogeneous material favor negative for Congo without typical polarization properties
Repeat Colonoscopy (1 month)
Resolution of large cecal mass with improvement in ulceration throughout colon. Only areas of mild erythema.
•Colonic mucosal biopsies with focal acute inflammation and granulation tissue formation. Submucosal pink amorphous material present which stains with
Congo red but does not show characteristic apple-green birefringence.
•Addendum: A PAS stain was performed and showed no definitive staining in the amorphous material. A Congo Red stain was repeated and also was negative for apple-green birefringence. Electon microscopy was performed as an aid to evaluate the amorphous material and electron microscopy photographs did not support the presence of amyloid deposition.
Clinical Course
1 month later, patient admitted with multiple episodes of hematochezia. Hemoglobin down to 5.3. Stool studies negative.
CT scan shows:
Transmural wall thickening with pericolonic fat stranding involving the rectum and sigmoid . There is also thickening of the cecum. In addition, this could also represent hemorrhage into the bowel wall in the setting of thrombocytopenia.
Repeat Colonoscopy (#3)
There were innumerable medium-sized punched-out ulcers in the rectum, rectosigmoid junction, and sigmoid colon.
Appeared to have progressed since prior endoscopy.
Extensive blood, fibrin, and inflammatory cells, with extremely scant epithelial cells. Inadequate tissue to evaluate for amyloid or plasmacytoma.
Repeat EGD/Colonoscopy (#4)
EGD normal.
Colonoscopy showed similar ulceration throughout colon with multiple biopsies taken.
Ischemic changes with ulceration, colonic epithelium. Congo red stain negative for amyloid.
Differential
With multiple unrevealing biopsies, what do you think is still on the differential for colonic ulcers?
Medication-associated ulcers (Velcade, Acyclovir)
Ischemic ulcers
Infectious ulcers
Amyloid
Plasmacytoma
Medication-associated colitis
“Acylovir- induced colitis”
3 cases of hematochezia within 24 hours of starting oral acyclovir (guanosine analog that inhibits viral DNA synthesis)
No other causes was found, and symptoms resolved with cessation
Colonoscopy showed friable mucosa with biopsy revealing ulcerated large bowel
Thought to be caused by local irritation to mucosal surfaces.
Wardle TD et al.
Medication-associated colitis
Case report of MM patient treated with Velcade (26S proteosome inhibitor) presenting with abdominal pain, hematochezia.
Colonoscopy showed multiple colonic ulcers, with pathology c/w severe interstitial inflammation.
Thought to be iatrogenic colitis 2/2 mucositis.
Sinischalchi et al.
Intestinal Plasmacytoma
Case reports of plasmacytoma in GI tract causing bleeding.
Extramedullary plasmacytoma account for 4% of plasma cell tumors.
Most occur in stomach and 20-30% in small intestine.
Biopsy shows plasma cell infiltrate, reactive for
CD138 (plasma cell marker).
Hypothesis that extramedullary plasmacytomas represent low-grade lymphoma of mucosal lymphoid tissues (MALT) with extensive plasmacytic differentiation.
Ammar et al. , Carneiro et al
Clinical course
Patient’s bleeding stabilized and he was discharged to home with stable hemoglobin.
Patient received Revlamid, Dexamethasone, but
Velcade was stopped due to possible association with ischemic colitis.
Re-admitted 1 month later with abdominal pain, diarrhea, hematochezia. Stool studies negative.
EGD/ Flex sig was performed.
EGD/Flex Sig (#5)
EGD
Multiple small patchy areas of irregular erosion in the incisura and antrum and on the lesser curvature of the stomach body.
Normal duodenum.
Flex sig
Multiple small ulcers in rectum and circumferential ulcers in sigmoid. Biopsies taken.
Pathology
Diagnosis
Amyloidosis of the Colon
Amyloidosis
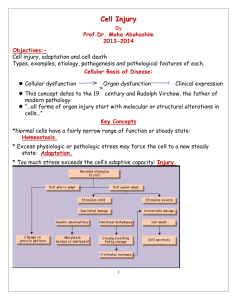
Extracellular deposition of protein fibrils with a β-sheet fibrillar structure.
Deposits appear homogeneous and amorphous under light microscope, but produce a green birefringence when stained with Congo red and viewed in polarizing microscope.
Types of Amyloid:
•Primary or light-chain associated (AL)- 15% have MM
•Secondary or reactive (AA)- chronic inflammatory disorders
•Hemodialysis associated (Aβ2M)
•Familial amyloid polyneuropathy (ATTR)
•Senile amyloidosis
Ebert EC et al.
Gastrointestinal Amyloid
Amyloid may cause GI symptoms extending from mouth to anus
Amyloid deposition in the GI tract is near universal in systemic AL amyloidosis, but only 30-60% develop GI symptoms.
When GI tract is involved, frequency of amyloid in biopsy specimens area 100% in the duodenum, 95% in the stomach, 91% in the colorectum, and 72% in the esophagus. Best in blood vessel wall.
Endoscopically, AL typically forms polypoid protrusions, while AA amyloidosis is characterized by a fine granular appearance
Sleisinger and Fordtran., Menke DM et al., Tada S et al., James et al.
GI manifestations
Amyloid deposition
Blood vessel wall
Muscle layers
GI bleeding
Dysmotility
Signs/ symptoms
Ulcers
Erosions
Polypoid lesions
Submucosal hemorrhage
Dysphagia
Gastroparesis
Constipation,
Pseudo-obstruction
Nausea/vomiting
Malabsorption
Mucosa
Weight loss
Diarrhea
Steatorrhea
Protein-losing enteropathy
Ebert et al.
Prognosis/ Treatment
Median survival for AL amyloidosis less than 2 years, if treated with melphalan and prednisone
5-year survival improved to 60% with hematopoietic stem cell transplantation
Treatment of AL involves chemotherapy, while
AA involved treatment of underlying disease.
Follow-up Course
After amyloid diagnosis, pt given Etoposide,
Cyclophosphamide, Dexamethasone.
2 weeks after EGD/Colonoscopy, pt with fevers, abdominal pain, hypotension. KUB showed no perforation.
Patient went to the OR. Ex-lap, lysis of adhesions, diverting ileostomy, and blow-hole colostomy was performed, but colectomy deferred due to patient instability.
Pt with prolonged post-operative hospital course. Restarted on Revlamid. On HD. Just discharged to home.
References
Ammar T et al. “Primary Antral Duodenal Extramedullary Plasmacytoma Presenting
With Melena” Clinical Gastroenterology and Hepatology. 2010;8:xxxii
Carneiro FP et al. “Extramedullary plasmocytoma associated with a massive deposit of amyloid in the duodenum.” World J Gastroenterol 2009 July 28; 15(28): 3565-3568
Ebert EC et al. “Gastrointestinal Manifestations of Amyloidosis.” Am J Gastroenterol
2008;103:776–787
James DG et al. “Clinical Recognition of AL Type Amyloidosis of the Luminal
Gastrointestinal Tract” Clinical Gastroenterology and Hepatology. 2007; 5:582–588.
Maza I et al. “Rectal bleeding as a presenting symptom of AL amyloidosis and multiple myeloma” World J Gastrointest Endosc 2010 January 16; 2(1): 44-46.
Menke DM et al. “Symptomatic gastric amyloidosis in patients with primary systemic amyloidosis.” Mayo Clin Proc 1993 Aug; 68(8):763-7.
Sinischalchi A et al. “Bortezomib-related colon mucositis in a multiple myeloma patient”
Support Care Cancer (2009) 17:325–327.
Sleisenger and Fordtran’s “Gastrointestinal and Liver Disease” Ninth ed, 2010.
Tada S et al. “Endoscopic and biopsy findings of the upper digestive tract in patients with amyloidosis.” Gastrointest Endosc 1990 Jan-Feb;36(1):10-4.
Wardle TD et al. “Acyclovir-induced colitis” Aliment Pharmacol Ther. 1997 (11): 415-
417