Small vessel disease in the CNS: an overview
advertisement
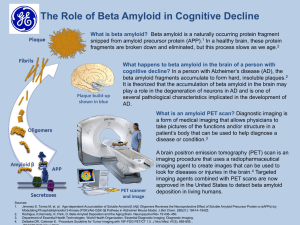
Small vessel disease in the CNS: an overview Alex Easton Capital Health and Dalhousie University, Halifax Injury to the CNS • Reduced cerebral blood flow (due to occlusion) causes ischemic injury (stroke) • Increased cerebral blood flow (eg due to acute hypertension) causes vessel rupture and hemorrhage • Primary rupture (eg because the wall is weakened as in an aneurysm) also leads to hemorrhage • Hemorrhage can result in secondary vasospasm (more ischemia) and both hemorrhage and ischemia increase vessel permeability (cerebral edema) Diseases of perforating arteries • This refers to perforating arteries with a diameter between 40 to 900 microns • The vessel wall can be structurally abnormal • The vessel wall can be inflamed • The vessel can be malformed or focally dilated The vessel wall can be structurally abnormal • There are 4 structural pathologies: – – – – Atherosclerosis (hypertension, diabetes) Fibrinoid necrosis (hypertension) Arteriolosclerosis (aging) Microaneurysms (hypertension) • The vessel wall is thickened in 3 main categories: – Arteriolosclerosis – Cerebral amyloid angiopathy – CADASIL The vessel wall can be inflamed (CNS vasculitis) • CNS vasculitis can be classified as: – Infectious – Non-infectious • Or as due to: – Immune injury – Direct infection The vessel wall can be malformed or dilated: • The two main categories are: – Vascular malformations – Aneurysms Structural pathologies • Atherosclerosis – Hypertension, diabetes and aging lead to extension of atherosclerosis into small vessels – The point of stenosis and occlusion is reached earlier than in larger vessels Structural pathologies Fibrinoid necrosis versus arteriolosclerosis • Both look very similar on H&E sections • Fibrinoid necrosis – Associated with hypertension – With atherosclerosis it tends to cause lacunar infarcts or primary brain hemorrhage • Arteriolosclerosis – Associated with aging – Tends to cause subcortical ischemic vascular dementia – These vessels tend NOT to rupture and bleed Microaneurysms • They may not exist Microaneurysms • They can rupture and bleed • But many patients don’t have hypertension • And the majority of hypertensive bleeds in some series don’t have microaneurysms Thickening of small arteries • Arteriolosclerosis • Cerebral amyloid angiopathy • CADASIL Cerebral amyloid angiopathy Cerebral amyloid angiopathy CAA – take home points • In most cases the amyloid is beta amyloid, a cleavage product of amyloid beta precursor protein encoded on chromosome 21 • Most cases are sporadic with or without Alzheimer’s disease • Familial causes include Down’s syndrome (Trisomy 21), familial Alzheimer’s disease, and hereditary cerebral hemorrhage with amyloid angiopathy of the Dutch and Flemish types CAA – take home points • Sporadic Aβ-CAA not associated with Alzheimer’s is rare under 60, with a 30% prevalence over 60 in autopsy series • 80-90% of Alzheimer patients have Aβ-CAA • In most people the disease is clinically silent CAA – take home points • Complications include: – Lobar hemorrhage (usually frontal and parietal lobes) – Isolated subarachnoid hemorrhage – Infarcts or white matter ischemia – Amyloid-beta related angiitis (a form of CNS vasculitis) CAA – take home points • Other forms of CAA are due to mutated precursor proteins giving rise to fragments that are prone to form amyloid: – Cystatin C – Gelsolin – ABri precursor protein (Bri=British) – ADan precursor protein (Dan=Danish) – Transthyretin – Prion protein CADASIL • Cerebral autosomal dominant arteriopathy with subcortical infarcts and leucoencephalopathy Vasculitis • Non-infectious or infectious Non-infectious v infectious • Non-infectious Either primary cranio-cerebral diseases Or related to systemic disease Primary diseases • • • • Primary CNS angiitis (and variants) Giant cell (temporal) arteritis Takayasu’s arteritis Kawasaki’s disease Systemic diseases • Systemic lupus erythematosis • Polyarteritis nodosa • ANCA-associated vasculitides (Wegener’s and ChurgStrauss) • Sjögren’s syndrome • Behçet’s syndrome • Rheumatoid arthritis • Hodgkin’s disease • Drug-induced Etc… Infectious causes • Bacterial – Spirochetal (eg borrelia/Lyme disease) – Purulent (eg streptococcal) – Granulomatous (eg due to TB) • Viral – Eg herpes zoster, Epstein-Barr virus • Other – Fungal, protozoal, mycoplasmal, rickettsial