Dr Vu Kwan - CIDM Public Health
advertisement
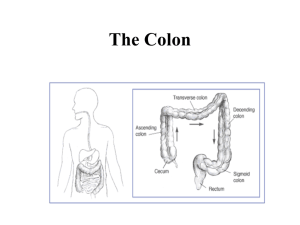
Dr Vu Kwan Staff Specialist Department of Gastroenterology Westmead Hospital 72 year old male Background: • Ischaemic heart disease NSTEMI 2009 Coronary stent Echocardiogram: EF 25% • Atrial fibrillation Warfarin • Chronic kidney disease Baseline creatinine ~180 Per rectum bleeding • Admitted for observation • Discharged for outpatient colonoscopy Recurrent bleeding • Admitted for inpatient colonoscopy Colonoscopy: • Multiple large colonic polyps • Endoscopic mucosal resection performed • Histology Multiple tubular adenomas Invasive malignancy not excluded Represented 3 days post-procedure with recurrent rectal bleeding ED assessment: • “Post-polypectomy bleeding” • “Possible peptic ulcer bleeding” Commenced on high dose proton-pump inhibitor infusion Observed for several days bleeding cessation Discharged home Represented 2 days later with bloody diarrhoea Up to 10 episodes per day Initially assumed to be ongoing postpolypectomy bleeding No stool tests performed Pseudomembranous colitis No history of recent antibiotics Only history: • Elderly male • Multiple co-morbidities • Repeated hospitalisations • Only new medication = PPI Commenced on oral metronidazole Ongoing fluid balance problems Dehydration due to diarrhoea Worsening renal function Fluid therapy resulting in pulmonary oedema Prolonged HDU admission with other medical complications Eventual resolution of diarrhoea & discharge 3 weeks later One of the most common healthcareassociated infections Spectrum of disease ranging from asymptomatic carriage to fulminant colitis Commonly a result of antibiotic therapy due to alteration of normal gut flora Can occur without antibiotic use, importantly via nosocomial transmission Mortality rates of up to ~25% reported, particularly in elderly1 1. Crogan et al, Geriatr Nurs 2007 Asymptomatic carriage C.difficile diarrhoea C.difficile colitis Pseudomembranous colitis Fulminant colitis Approximately 20% of hospitalised patients are C. difficile carriers Significant reservoir for disease transmission Contribution is unclear of host’s immune response Watery diarrhoea • >3 times per day • >2 days duration More severe cases • • • • Up to 15 motions per day Lower abdominal pain and cramping Low grade fever Leucocytosis Onset may be during antibiotic therapy or 5-10 days after treatment • Can present up to 10 weeks after antibiotic cessation More significant illness than diarrhoea alone Constitutional symptoms, fever, abdominal pain + watery diarrhoea Colonoscopy: • Non-specific diffuse or patchy erythematous colitis The classic manifestation of full-blown C.difficile colitis Symptoms similar to, but often more severe than, colitis due to other causes Unwell, WCC, hypoalbuminaemia Colonoscopy: • Classical raised white/yellow plaques Severe manifestation affecting ~3% Account for the Perforation Prolonged ileus Toxic megacolon Death Clinical most serious complications: features of fever, leucocytosis, abdominal distension 1 Small bowel 2 Bacteraemia 3 Reactive arthritis 4 Others Particularly described in small bowel subjected to recent surgery • Inflammatory bowel disease post ileal-anal anastomosis Pseudomembrane May formation act as a reservoir for recurrent colonic infection? Uncommon Associated with high mortality rate1 May be more common in patients with underlying gastrointestinal diseases2 1. Daruwala et al, Clin Med Case Reports 2009 2. Libby et al, Int J Infect Dis 2009 Polyarticular arthritis • Knee and wrist in 50% of cases Onset average 11 days after diarrhoea1 Prolonged resolve2 illness : average 68 days to 1. 2. Birnbaum et al, Clin Rheumatol 2008 Jacobs et al, Medicine (Baltimore) 2001 Cellultis Necrotising fasciitis Osteomyelitis Prosthesis infection Intra-abdominal abscess Empyema etc General risk factors 1. Long duration antibiotics 2. Multiple antibiotics 3. Nature of faecal flora 4. Production of requisite cytotoxins 5. Presence of host risk factors Specific risk factors 1. Immunosuppressive drugs 2. Gastric acid suppression 3. Cancer chemotherapy with antibiotic properties Advanced age Nasogastric tube Severe underlying illness Prolonged hospitalisation Enema therapy GI stimulants Stool softeners Chronic, relapsing inflammatory disorders of the bowel of unknown aetiology Ulcerative colitis Crohn’s disease Enteric infections account for ~10% of ‘relapses’ • C.difficile in about half • May mimic a relapse, OR trigger a true relapse Crucial that C.difficile is considered in the differential diagnosis of every ‘flare’ Otherwise inappropriate escalation of immunosuppression may result in severe infection High index of suspicion required as classical pseudomembranes don’t form in IBD Treatment is to REDUCE their usual immunosuppressive drugs Gastric acid inhibits germination of ingested C.dificile spores Therefore, medications lowering gastric acid could increase risk of C.difficile infection • Clinical data are conflicting Abdominal CT xray scan Colonoscopy Important in patients who are unwell with C.difficile infection Findings: • Ileus • Toxic megacolon • Perforation Diagnosis Several can often be made on CT alone characteristic findings: • Gross bowel wall thickening • Luminal narrowing • Characteristic signs: “Accordion sign” “Target sign” Pathognomonic appearance of pseudomembranes • Raised, white/yellow plaques Up to 1/3 right-sided only, so full colonoscopy better than sigmoidoscopy Biopsies reveal spectrum of mucosal inflammation and necrosis Beware colonoscopy in unwell patients with ileus or megacolon • Risk of perforation If clinical picture and stool tests are suggestive, minimal role for colonoscopy Health-care associated infection of great clinical significance Spectrum of disease ranging from asymptomatic infection to fuliminant colitis and death Imaging investigations are complimentary to clinical index of suspicion Approximately 15-20% of patients with CDAD relapse following successful treatment • One relapse predicts further relapses! Sudden recurrence of diarrhoea within ~1 week of treatment cessation